Pyomyoma as a Complication of Uterine Artery Embolization (A Case Report) ()
1. Introduction
Adenomyosis is a benign uterine disorder in which endometrial glands and stroma are inserted in the myometrium, and it is one of the leading causes of abnormal uterine bleeding [1] . As part of its management, physicians may offer patients Uterine Artery Embolization as a less invasive method for treating menorrhagia. A rare but serious complication of UAE is the development of Pyomyoma in the pelvic cavity.
Pyomyoma, or suppurative leiomyoma is a rare condition resulting from infarction and infection of leiomyoma [2] . Even though only 10 cases were reported of pyomyoma post UAE [3] , it still can lead to sepsis and consequently death if not treated aggressively with antibiotics and surgical intervention [4] . This case report shows the case of pyomyoma which extended into the uterine cavity causing pyometra.
2. Case Report
A 45-year-old female, P1A5L0, came to the emergency department complaining of fever and foul smelling vaginal discharge for several weeks. The patient started having these symptoms shortly after undergoing Uterine Artery Embolization in July 2023 in another facility for her menorrhagia provoked by adenomyosis.
The patient also underwent evacuation of necrotic ademomyotic material in said facility with recurrent admissions for blood transfusion and intravenous antibiotics. As the patient was not reposing to treatment and having no improvement in her symptoms, she came to our facility.
Upon admission, the patient had temperature of 38.3˚C, blood pressure 102/66mmhg, Pulse 114 bpm, O2 saturation 97% on room air.
On examination, per abdomen was soft, non-tender, the uterus was at 20 - 22 weeks. Per vaginal examination via speculum showed vaginal discharge. A high vaginal swab was obtained which came back negative for molecular vaginitis. Laboratory investigations results are summarized in Table 1.
Patient was kept on IV Tazocine, Doxycycline and Metronidazole and was admitted for further workup.
The decision was made to take the patient for evacuation of pyomyoma under ultrasound guidance. 200 ml of pus material was drained with difficulty and sent for culture and sensitivity. Result came as mixed growth, meaning the specimen was contaminated.
The patient was counseled regarding her symptoms, CT scan and Evacuation findings and pre existing condition of adeomyosis, then she was posted for hysterectomy because pyomyoma persisted after the evacuation attempt.
The patient underwent Total Abdominal Hysterectomy with Bilateral Salpingectomy and Preservation of Ovaries on 25/09/2023. Intra operative findings revealed enlarged uterus about 20 weeks in size with friable tissue and organized
![]()
Table 1. CT scan of abdomen and pelvis with IV contrast was done, it showed significantly enlarged uterus, measured about 20 cm in longitudinal axis and 13 cm * 8.8 cm in transverse axis, appeared to be severely distended due to the presence extensive intrauterine air causing significant thinned out of myometrium. The findings correlate to Pyomyoma secondary Uterine Artery Embolization (Image 1 & Image 2).
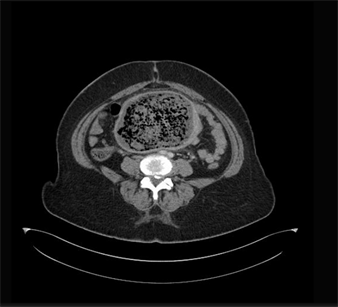
Image 1. Axial view of CT scan showing air collection in uterus, evidence of pyomyoma.
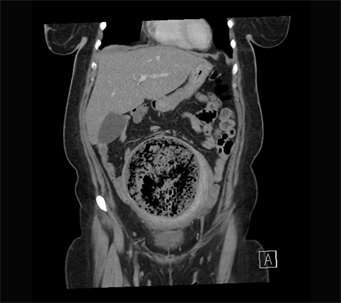
Image 2. Coronal view of CT scan showing air collection in uterus, evidence of pyomyoma.
pus inside the uterine muscle and cavity, which came out as a ball of organized pus, sized 15 * 7 cm from the uterus during manipulation (Images 3-5). Due to the nature of the pelvic infection, the omentum was densely adherent to the anterior of the uterus along with the mesentery of the small bowel and adhenolysis was successfully done.
Histopathology report showed necrotic mass with exudates weighing 180 g and showing features of adenomyosis with extensive ischemic necrosis.
The patient did well post op and was discharged after her course of antibiotics. She is currently doing well and given an appointment to follow up in the gynecology clinic.
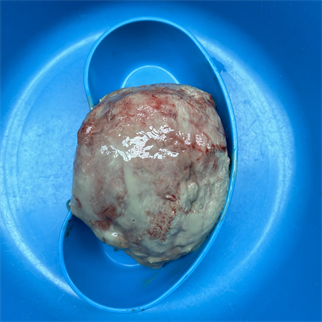
Image 3. Intra op finding of the pyomyoma, an organized pus collection, sized 15 cm * 7 cm and weighing 180 g.

Image 4. The friable uterus ruptured after removing the pyomyoma.
3. Discussion
Uterine Artery Embolization (UAE) is performed to cause ischemia and necrosis of fibroids and/or adenomyosis while preserving the function and vascularization of the uterus [5] . It is a minimally invasive procedure performed as an alternative to those who wish to preserve their fertility [6] . UAE has helped avoid hysterectomy in 96% of patients and improved the symptoms in 74% of them, according to Yuan et al. study [7] .

Image 5. Pyomyoma next to the friable uterus.
The resulting ischemia of the leiomyoma leads to its infarction and necrosis and infrequently this may lead to the development of Pyomyoma. Patients affected with Pyomyoma may present with a triad of pelvic pain, sepsis and unknown source of infection [8] . Since the nature of its vague symptoms, the diagnosis of it can be challenging as it mimics Post Embolization Syndrome (PES) which can also present with said symptoms within 1 week of undergoing UAE [3] . PES is seen in 21% of patients post UAE, and it is a self-limiting condition managed with hydration and pain control [3] . But if the symptoms persisted beyond 1 week it should raise the suspicion of other diagnosis namely, tubo-ovarian abscess, degenerated leiomyoma, infected ectopic pregnancy or malignancy [9] .
Imaging modalities such as CT scan and MRI of the pelvis and abdomen may show gas inclusion with the presence of gas collections of the necrotic fibroid can indicate Pyomyoma [10] .
Broad spectrum antibiotics and eventfully hysterectomy is the management of choice for Pyomyoma [8] [11] .
As in the case of our patient, pus material was drained with difficulty during the D&C which was offered first because she wished to preserve her fertility. Since pyomyoma was still present after the D&C, and given the patient’s bad obstetric history, she was offered and underwent Total Abdominal Hysterectomy with the preservation of the ovaries, in which an organized ball of pus was excised from inside the uterus.
4. Conclusions
Uterine Artery Embolization is offered for patients suffering from abnormal uterine bleeding secondary to adenomyosis and/or fibroid. It is offered for those who wish to preserve their fertility and avoid undergoing hysterectomy.
If a patient comes to the hospital complaining of fever, pelvic pain and vaginal discharge post UAE, it should prompt the physician into suspecting Pyomyoma as a differential no matter how rare it is. Ordering CT scan or MRI for the patient may aid in the diagnosis of Pyomyoma, as it shows as gas collection in the pelvic cavity.
Managing the patient with aggressive broad spectrum antibiotics and eventually hysterectomy is considered as the treatment choice. Once the diagnosis of Pyomyoma is made, counseling the patient for hysterectomy is encouraged to prevent the patient from going into sepsis, and to decrease the chances of morbidity and mortality.
Disclosure
Informed consent was obtained from the patient.