Knowledge, Attitude and Practice Regarding HIV/AIDS among Students in China ()
1. Introduction
Human immune virus infects cells of the immune system which result in the progressive deterioration of the immune system, breaking down the body’s ability to fend off some infections and other diseases [1] . AIDS (Acquired immune deficiency syndrome) refers to the most advanced stages of HIV infection, defined by the occurrence of any of more than 20 opportunistic infections or related cancers [1] [2] [3] . The first case of Human immune Virus (HIV) was recognized in United States in 1981 [4] . HIV/AIDS remains one of the world’s most significant public health challenges, particularly in low and middle-income region [5] . The statisticians from joint United Nations Program on HIV/AIDS (UNAIDS) and WHO estimated that there are approximately 36.7 million people living with HIV at the end of 2016. 34.5 million are adults, 17.8 million women, 16.7 million men, and 2.1 million children below 15 years. People newly infected with HIV in 2016 are 1.8 million of which 1.7 million are adults. Total AIDS death in 2016 was 1.0 million of which 890,000 were adults [6] . Recently due to non-achievement of millennium goals on HIV/AIDS in different countries in the world especially in developing countries, the joint UN program on HIV/AIDS has fixed new objectives to overcome HIV infections by 2030 [7] [8] .
2. Overview of HIV/AIDS in China
The first case of HIV was reported in 1985 [9] . In 2011, more than 50% of people living with HIV did not know their HIV status. 55% were infected by heterosexual activities. Among them 68.7% contracted the disease through casual or commercial sexual interactions. The United States Nations, WHO and Ministry of Health of China Joint panel on HIV and AIDS presented the data that there were 780,000 estimated numbers of people living with HIV in China in 2011 [10] . The national HIV prevalence was 0.058%. 3.5 million people are living with HIV in Southeast Asia in 2016 [6] . Treatment aimed at improving prognosis and delaying morbidity is costly not only in China but in the whole world. Although government and international organizations made effort to stop new HIV infection by 2015 in China, but evidence showed that communicable infections continue to occur while decimating the lives [11] . The HIV/AIDS epidemic in China presents four major characteristics: first, the national HIV/AIDS epidemic maintains a low-prevalence trend, with higher-prevalence in some areas and among some groups; second, the number of people living with HIV/AIDS continues to increase, with HIV/AIDS showing high differentiation in prevalence among different groups; third, the number of AIDS patients rises markedly, with the number of all-cause deaths becoming stable; and fourth, sexual transmission is the primary mode of transmission with sexual transmission between men increasing markedly [12] . In 2014, according to the requirements of “the Regulations on HIV/AIDS Prevention and Control” and “China’s 12th Five-Year” Action Plan for Containment and Prevention of HIV/AIDS”, China continued to implement the major response measures of “Five Expands and Six Strengthens”, thus achieving marked progress in multiple areas. In the area of prevention and intervention, the percentage of female sex workers who are living with HIV has been comparatively low in recent years and in 2014 it was 0.22%. The percentage of people who inject drugs who are living with HIV has been stable with a slight decline, dropping from 6.33% in 2013 to 6.00% in 2014 [1] [7] [12] . During 2010-2014, reported cases of people living with HIV/AIDS continued to increase from 307,000 in 2010 to 352,000, 386,000, 437,000 and 501,000 in 2011, 2012, 2013 and 2014 respectively (Figure 1) [12] .
The main reasons for the increase include: the number of people receiving testing has been growing year by year and therefore, more cases of HIV/AIDS have been found accordingly; the number of patients receiving ART treatment has been steadily increasing by a large margin each year, prolonging the lives of people living with HIV/AIDS [7] [12] . Many studies have shown that HIV infection is shifting from men who sex with men to heterosexuals particularly among youth at reproductive age [13] . Particularly the Vulnerable groups to the HIV are young people [14] .
3. Knowledge, Attitude and Practice Regarding HIV/AIDS
In China the university students are among the effected target population because of the recent development of casual attitude towards sex, the rapid economic revolution and degradation of traditional value [15] . In these groups there is lack of adequate information regarding HIV knowledge and behavior that might be hit hard by the HIV pandemic. So it is essential to access Knowledge, Attitude and Practice of individuals before planning preventions. The purpose of this review is to summarize the latest publications about HIV/AIDS-related
![]()
Figure 1. Geographic Distribution of People Living in China with HIV/AIDS in 2014 [12] .
knowledge, beliefs and sexual behavior among students in China. This summarized study will provide knowledge and understanding of issues and lead to effective suggestions for further research and implementation. There are several articles regarding the HIV/AIDS-related knowledge, beliefs and sexual behavior among students in China.
We went through the search engine as GOOGLE SCHOLAR, PUBMED, BAIDU and SCOPUS. 79 articles related to the topic regarding HIV/AIDS were selected of which 25 articles related to HIV/AIDS in China were separated. Of the 25 articles 8 articles related to our study regarding Chinese students Knowledge; attitude and practice were finalized for the review (Figure 2).
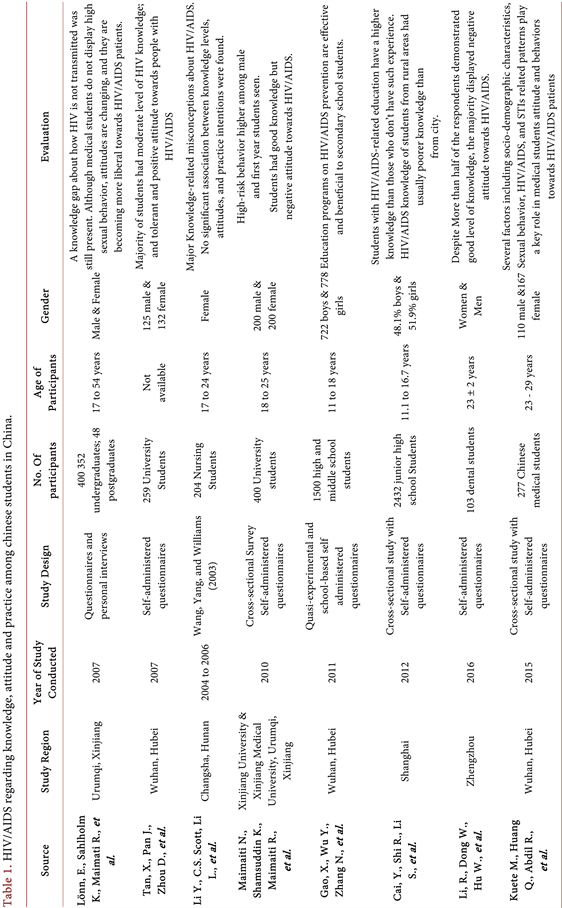
All the 8 articles were published between 2007 to 2016 and selected on their validity, reliability, number of samples, relation to the AIDS/HIV, Chinese students’ knowledge, their attitude and Practice towards the disease (Table 1).
3.1. Lönn, E., Sahlholm K., Maimati R., et al., AIDS Patient Care and STDS, 2007 [16]
The study was based on questionnaire and personal interviews of medicine
![]()
Figure 2. Flow diagram showing selection process of articles included in the review.
students at Xinjiang medical university in Urumqi during spring 2004. The questionnaire consisted of 40 questions divided into four categories: general questions, Knowledge about HIV/AIDS, personal questions and questions about the work situation. Total of 400 individuals participate with age ranged from 19 to 32. 352 undergraduates and 48 postgraduate students with both male and female had participated. Of the 352 undergraduate students, all but 1 stated that they had heard of HIV/AIDS while majority of postgraduate had heard the disease. The 69.8% of Postgraduates had heard about HIV in the media, 18% had heard of it at school, 3.5% from friends and 2.5% from their parents. A total of 9.7% of the undergraduate students and 3% of postgraduate students said that whether a person is infected with HIV/AIDS could be determined by just looking at them. 54.5% of the undergraduates’ students and 88% of the postgraduates said they know of symptoms. 44% postgraduates and 9.4% undergraduate students believed that there was a medicine that cures HIV/AIDS. 20% of all the students answered that they would talk with fathers about HIV/AIDS. 60% of undergraduate students and 52% of the postgraduate students wanted to be tested for HIV. 89.8% undergraduate and 98% postgraduate students did not want to have child if they were infected with HIV/AIDS. 79.3% of undergraduate students had not had any sexual contact. Over half (58%) of the postgraduates had one sexual partner. 69% of undergraduate and 39.8% of the undergraduate students were afraid of being infected with HIV at work.
3.2. Tan, X., Pan J., Zhou D., et al., International Journal of Environmental Research and Public Health, 2007 [15]
The validity test was 0.7 and reliability was 0.78. Self-administered questionnaire was used to investigate KAP regarding HIV/AIDS. The questionnaires were modified in accordance to WHO recommendation and Chinese culture. Total range for score was 0 to 57 with students of HIV knowledge have higher score, more accepting attitude about and engaged in fewer HIV risky behaviors. In the survey 259 students participated of which 125 male and 132 female. The mass media (newspapers and magazines, 64% television and radio 48.8%) was the major sources for getting information about HIV and AIDS. The analysis of research showed that although some has high knowledge (17.8%). The majority had moderate knowledge. The total correct answer rate regarding pertaining to source of HIV/AIDS was 69.4%. 47.5% students answered all HIV transmission questions correctly. Moderate knowledge of prevention noted in 10.9% students. The attitudes of respondents towards people with HIV/AIDS were found accepting and Positive. 153 (59.8%) voiced strong willing to live in the same community with HIV/AIDS people. Rate of expression of having sexual intercourse were 6.9%. Age of onset of sexual intercourse was from 18 to 23. 35.7% mentioned condom used during sexual practice. Boys have greater acceptance in comparison to girls towards accepting people with HIV/AIDS. Knowledge difference was between medical and non-medical student while no significant attitude difference.
3.3. Li Y., C.S. Scott, Li L., et al., Applied Nursing Research, 2008 [17]
The study was based on questionnaire that compromised 204 nursing students from 10 nursing schools at Xiangya hospital of central south university in 2004. There was 100% response rate with all female respondents. No any student has had direct contact with people with AIDS while six respondents had experienced needle stick injury. The study has four parts as demographic data, a 24-item AIDS knowledge scale, a 21-statement AIDS attitude scale and a willingness to provide care scale. There was a significant difference in levels of AIDS knowledge among students from different education backgrounds. A positive relationship between nursing education background and general HIV/AIDS knowledge was seen. 94% of nursing students understand that HIV/AIDS is an infectious disease caused by virus, 90% knows that there is no cure for HIV/AIDS. Most recognized that sharing needles can cause HIV infection (97%), an HIV- positive mother can cause HIV (87%), and HIV can be transmitted via sexual intercourse (80%). Although, 12% have only knowledge that the risk of HIV infection from needle stick injury is <1%. There were no significant difference between education level and attitudes towards PWA were noted. Most of Chinese nursing students believed that PWA has the right to the same quality of care as any other patient. Only 73% of them agreed that partners of homosexuals should receive equal respect. 34% of the nursing students believed that most people with HIV/AIDS deserved what they got. 48% of nursing students strongly agreed that young children should be removed from the home if one of the parents was HIV-positive. A weak positive relationship between attitude and willingness to provide care was found.
3.4. Maimaiti N., Shamsuddin K., Maimaiti R., et al., Global Journal of Health Science, 2010 [18]
This was a cross-sectional surgery conducted using self-administered questionnaires in two public universities in Urumqi Xinjiang in 2010. The students were registered for non-medical degree program at Xinjiang University and medical degree program in Xinjiang medical university. Total 400 students were selected that included equal number of students by sex, year of enrollment and study major (medical or non-medical). 200 male and 200 female students distributed by year of enrollment from 2 universities. The questionnaire comprised of four parts: socioeconomic background, knowledge regarding HIV/AIDS, AIDS attitude scale and high-risk behavior or practice related to HIV/AIDS transmission. The age ranged from 18 years to 25 years. Only 109 (27.3%) respondents had attended on HIV/AIDS related lecture or training program. More than 80% knew that HIV/AIDS could be transmitted via sharing syringe/needles as well as vertical transmission from mother to child and about 65% - 75% thought condom could prevent HIV transmission during sexual intercourse. 59.5% thought one can get HIV through mosquito bite, and 38.5% thought HIV/AIDS is homosexual people disease. 84.3% of the respondents thought their friends will avoid them if they were found to be HIV positive. 54% felt persons with HIV/AIDS deserve it. 30% felt that HIV infected students should be treated differently. 15.8% of all respondents had risk behavior related to HIV/AIDS transmission. 10% reported having unprotected sex, 6% had more than 1 sexual partner and 4.5% reported having sex under the influence of alcohol. There was no significant behavior difference between medical and non-medical students. Male students are reported at more risk behavior than female students.
3.5. Gao, X., Wu Y., Zhang N., et al., PLoS One, 2012 [19]
The questionnaires based on adolescent AIDS knowledge scale by Zimet (1998) and the request of knowledge about AIDS/HIV prevention for young people by the United Nations general assembly special section. The study consisted of 38 closed-ended questions including 10 questions on socio-demography information, 18 questions on HIV/AIDS knowledge, 4 questions on HIV/AIDS attitude, 5 questions on high-risk behaviors and 1 question on source of HIV/AIDS knowledge. Response rate was 97.8% (1468/1500). It constituted 877 middle school students and 59 high schools students. The mean age was 14.71 years. 691 (78.79%) of middle school students and 455 (76.99%) high school students were from middle class economy. The study showed that the middle school students had a low rate of awareness except in two questions such as “AIDS/HIV is an infected disease (84.72%) and AIDS can be prevented (83.35%). More than 65% of middle school students and 90% of the high school students identified three modes of transmission, namely sexual, blood transfusion and mother-to-child transmission. A large proportion of middle and high schools (18.70% and 26.73% respectively) believe that mosquitoes can spread the virus. Television broadcast was reported as major source of information (821, 55.93%). 537 (61.23%) middle school and 406 (60.70%) high school students prefer to help people living with HIV/AIDS. 27 (1.84%) students reported to have sexual relations. The sexual initiation age range from 11 years to 18 years old. 74.07% students among the sexually active students knew how to protect during sexual encounter. 1.50% reported drug and substance abuse and six students shared injection needles. Only 38.8% of the middle school students and 67.17% of high school students knew that no cure exists for AIDS.
3.6. Cai, Y., Shi R., Li S., et al., International Journal of STD & AIDS, 2012 [20]
Ten junior high schools were selected randomly from each district of shanghai and 2580 students were the study sample. 2432 students (94.3%) completed the HIV/AIDS related questionnaires. HIV/AIDs questionnaire were designed on socioeconomic and demographic characteristics, 31 items on HIV/AIDS related knowledge, and some items on sources of HIV/AIDS related information. The mean age of the final sample was 14.04 years of which 48.1% boys and 51% girls. Students aged 14 years or older had more HIV/AIDS related knowledge than those younger than 14. The overall correct rate of HIV/AIDS related knowledge was 62%. The education about HIV/AIDS among students in junior high schools was 50% and they were familiar with the ways by which HIV is transmitted. A student who is the single child in the family has higher HIV/AIDS related knowledge when compared with students who have sisters or brothers. Knowledge of HIV/AIDS of students from rural areas is usually poorer than those from the city. Similarly students who have discussed HIV/AIDS with their parents have a higher knowledge those who have not.
3.7. Li, R., Dong W., Hu W., et al., Journal of Dental Sciences, 2016 [21]
The study was conducted on 103 dental students at first affiliated hospital of Zhengzhou University. A self administered structured questionnaire was used as the survey instrument which composed of HIV/AIDS potential route of transmission, risk groups and attitude toward HIV positive individuals. A total score range from 0 to 11 on the basis of answers of the participant was done. The attitude of students was based on 17 questions. Students’ attitude scores were counted from 1 to 5 with the total score ranging from 17 to 85. The response rate of the survey was 92.2% of which 68.4% were women and 31.6% were men with mean age 23 ± 2 years. The total mean score on knowledge was 79.4 ± 6.3 with male students score 78.3 and female students score 79.9. Only 2.1% respondents scored > 90, indicated excellent knowledge. Also, 51.6% of students exhibited good scores, 42.1% considered moderate and 4.2% considered weak. Only 64.2% were aware of the average time interval between HIV infection and detection of HIV antibodies in blood or other fluids. 54.7% of students regarded mosquito bites as a possible transmission route. 93.7% expressed predominantly negative attitudes. Only 2.1% of the dental students exhibited professional attitudes toward the disease.
3.8. Kuete M., Huang Q., Abdil R., et al., BioMed Research International, 2016 [22]
The study was a cross-sectional study using validated self-administered questionnaire conducted in Tongji Medical College affiliated to Huazhong University of science and technology in Wuhan from March 01 to June 14, 2015. 277 Chinese medical students all sexually active were included in the study. The variables for the study were gender, age, education level, martial status, region of origin, sexual orientation, number of sex partners, frequency of condom use, history of HIV and STIs testing, and vaccination for curable infections (syphilis, hepatitis B and C, and tuberculosis). 95.67% of Chinese students provide the right answer related to the nature of pathogen. 90.97% of students agreed that condom makes sexual intercourse safe in HIV acquisition. The majority of students reported extracurricular training in HIV/STIs and almost all had wished to know more about HIV/AIDS. 45.49% of Chinese students opted to avoid condom usage after HIV testing of partners while 16.97% agreed to have unprotected sex after mutual decision without HIV testing. 28.88% of students prefer to keep away from infected individual and 25% refused promoting patient rights and considered HIV infection highly dangerous.
4. Discussion and Conclusions
All studies in this review have reported significant positive intervention effects in HIV-related knowledge, attitude and practice among Chinese students. These studies show that there has been significant improvement in the intervention and controlling of HIV/AIDS in China. All the 8 identified studies in this review were published after 2007. Most of these studies were geographically concentration at HIV/AIDS region. Although there is great effort made by international organizations, non-government organization, and institutions in developing region for education about communicable diseases, several misconceptions are persistent among students including medical students on HIV/AIDS and STIs [23] [24] . Although students have good knowledge regarding HIV/AIDS, they have still negative attitude towards HIV/AIDS patients. Knowledge alone is not enough to change the negative attitude of the students towards the HIV patients but social and culture factors also play vital role for the development of the attitude. Condom use during sexual intercourse is an essential component of HIV/AIDS prevention whereas there is less rate of wearing condom during sexual intercourse. Sexually active students are still shy to buy condom due to cultural norms related especially to unmarried youths. Condom promotion should be done. HIV/AIDS education will be more successful if education is carried out using continuous and long-term realistic objectives [25] [26] . Health promotion program need to be focused for students. There are still misconceptions among students that mosquito bite and kissing can transmit HIV. There is difficulty in separating HIV from AIDS by many students. Due to insufficient knowledge regarding HIV/AIDS among school students many of them believe that there is a medicine that can cure HIV/AIDS. This shows lack of sufficient knowledge regarding HIV/AIDS among schools students compared to university students. Today’s students live in an era of mass communication, in which they have easier access to HIV information compared with decades ago. It is essential to focus not only on knowledge but also on developing and maintaining safe sexual behavior.
It is important that all the students from schools and colleges should have knowledge regarding HIV transmission and prevention as well as they should develop positive attitude towards the HIV patients. To ameliorate the deficiencies, China desperately needs higher quality evidence-based knowledge dissemination and attitude improvement programs for students. It can be concluded from the review that Chinese students have high level of knowledge while there are several misconceptions, confusion, and fear existed among them. Students’ background and sexual activity has strong impact on their attitude and behaviors towards people infected with HIV/AIDS. All these analyses lead to the conclusions about the fight against AIDS. It is important to focus research and interventions on young people especially students. This review paper will promote our knowledge and understanding of these issues and lead to effective suggestions regarding directions for further research and implementation in the field of HIV/AIDS in China.
Acknowledgements
We would like to thank all the faculty members especially Professor Rui Chen from School of Public Health Southeast University China for his coordination. Further, we express our gratitude towards Singh Ratish from school of Medicine Southeast University China and Singh Abanish from B.P. Koirala Institute of Health Sciences Nepal for their guidance.
Conflict of Interest
The authors have no conflict of interest relevant to this article.
Neha, S. and Xiao, Z. (2017) Knowledge, Attitude and Practice Regarding HIV/AIDS among Students in China. World Journal of AIDS, 7, 247-259. https://doi.org/10.4236/wja.2017.74021
References
- 1. WHO (2017) HIV/AIDS Fact sheet N°360". http://www.who.int/mediacentre/factsheets/fs360/en/
- 2. Sepkowitz, K.A. (2001) AIDS—The First 20 Years. New England Journal of Medicine, 344, 1764-1772. https://doi.org/10.1056/NEJM200106073442306
- 3. Kramer, A., Kretzschmar, M. and Krickeberg, K. (2010) Modern Infectious Disease Epidemiology: Concepts, Methods, Mathematical Models, and Public Health. Springer, Berlin. https://doi.org/10.1007/978-0-387-93835-6
- 4. Selik, R.M., Haverkos, H.W. and Curran, J.W. (1984) Acquired Immune Deficiency Syndrome (AIDS) Trends in the United States, 1978-1982. The American Journal of Medicine, 76, 493-500. https://doi.org/10.1016/0002-9343(84)90669-7
- 5. Dandona, R., et al. (2005) High Risk of HIV in Non-Brothel Based Female Sex Workers in India. BMC Public Health, 5, 87. https://doi.org/10.1186/1471-2458-5-87
- 6. WHO (2017) Data and Statistics. World Health Organization. http://www.who.int/hiv/data/en/
- 7. UNAIDS (2017) UNAIDS Strategy. http://www.unaids.org/en/goals/unaidsstrategy
- 8. Rewari, B.B., et al. (2017) Adoption of the 2015 World Health Organization Guidelines on Antiretroviral Therapy: Programmatic Implications for India. WHO South-East Asia Journal of Public Health, 6, 90. https://doi.org/10.4103/2224-3151.206171
- 9. Wu, Z., et al. (2007) Evolution of China’s Response to HIV/AIDS. The Lancet, 369, 679-690. https://doi.org/10.1016/S0140-6736(07)60315-8
- 10. The Central People Government of the People's Republic of China (2011) An Estimate of 780,000 People Living with HIV in China. http://www.gov.cn/gzdt/2011-11/23/content_2001819.htm
- 11. Zhao, Y., et al. (2015) Risk Factors of HIV and Other Sexually Transmitted Infections in China: A Systematic Review of Reviews. PloS One, 10, Article ID: e0140426.
- 12. National Health and Family Planning Commission of the People’s Republic of China (2015) China AIDS Response Progress Report. http://www.unaids.org/sites/default/files/country/documents/CHN_narrative_report_2015.pdf
- 13. Wu, Q., et al. (2010) A Model of Expanding HIV/AIDS Education in Chinese Rural Areas. International Journal of STD & AIDS, 21, 87-92. https://doi.org/10.1258/ijsa.2009.008508
- 14. Ergene, T., et al. (2005) A Controlled-Study of Preventive Effects of Peer Education and Single-Session Lectures on HIV/AIDS Knowledge and Attitudes among University Students in Turkey. AIDS Education & Prevention, 17, 268-278. https://doi.org/10.1521/aeap.17.4.268.66533
- 15. Tan, X., et al. (2007) HIV/AIDS Knowledge, Attitudes and Behaviors Assessment of Chinese Students: A Questionnaire Study. International Journal of Environmental Research and Public Health, 4, 248-253. https://doi.org/10.3390/ijerph2007030009
- 16. Lonn, E., et al. (2007) A Traditional Society in Change Encounters HIV/AIDS: Knowledge, Attitudes, and Risk Behavior among Students in Northwestern China. AIDS Patient Care and STDS, 21, 48-56. https://doi.org/10.1089/apc.2006.0063
- 17. Li, Y., Scott, C.S. and Li, L. (2008) Chinese Nursing Students’ HIV/AIDS Knowledge, Attitudes, and Practice Intentions. Applied Nursing Research, 21, 147-152. https://doi.org/10.1016/j.apnr.2006.10.004
- 18. Maimaiti, N., et al. (2010) Knowledge, Attitude and Practice Regarding HIV/AIDS among University Students in Xinjiang. Global Journal of Health Science, 2, 51. https://doi.org/10.5539/gjhs.v2n2p51
- 19. Gao, X., et al. (2012) Effectiveness of School-Based Education on HIV/AIDS Knowledge, Attitude, and Behavior among Secondary School Students in Wuhan, China. PLoS ONE, 7, e44881. https://doi.org/10.1371/journal.pone.0044881
- 20. Cai, Y., et al. (2012) Study of HIV/AIDS-Related Knowledge among Junior High-School Students in Shanghai, China. International Journal of STD & AIDS, 23, e9-e12. https://doi.org/10.1258/ijsa.2009.009065
- 21. Li, R., et al. (2016) Chinese Dental Students’ Knowledge and Attitudes toward HIV/AIDS. Journal of Dental Sciences, 11, 72-78. https://doi.org/10.1016/j.jds.2015.09.001
- 22. Kuete, M., et al. (2016) Differences in Knowledge, Attitude, and Behavior towards HIV/AIDS and Sexually Transmitted Infections between Sexually Active Foreign and Chinese Medical Students. BioMed Research International, 2016.
- 23. Myint, K.Y., Naing, K.S. and Hanni, M. (2012) Knowledge, Awareness and Attitudes Related to HIV/AIDS among Undergraduate Medical Students of Universiti Malaysia Sabah. In: EDULEARN 12 Proceedings, IATED.
- 24. Dutcher, M.V., et al. (2011) “Positive Examples”: A Bottom-Up Approach to Identifying Best Practices in HIV Care and Treatment Based on the Experiences of Peer Educators. AIDS Patient Care and STDs, 25, 403-411. https://doi.org/10.1089/apc.2010.0388
- 25. Ungan, M. and Yaman, H. (2003) AIDS Knowledge and Educational Needs of Technical University Students in Turkey. Patient Education and Counseling, 51, 163-167. https://doi.org/10.1016/S0738-3991(02)00190-8
- 26. Kyrychenko, P., Kohler, C. and Sathiakumar, N. (2006) Evaluation of a School-Based HIV/AIDS Educational Intervention in Ukraine. Journal of Adolescent Health, 39, 900-907. https://doi.org/10.1016/j.jadohealth.2006.06.006
ACRONYMS
HIV: Human immunodeficiency virus
AIDS: Acquired immunodeficiency syndrome
STI: Sexually-transmitted Infection
KAP: Knowledge, attitude and practices
WHO: World Health Organization
UN: United Nations
UNAIDS: The Joint United Nations Programme on HIV and AIDS