The Evaluation of the Knee Joint in Terms of Magnetic Resonance Imaging Measurements in Osteoarthritis Patients: A Comparative Study Comprising a Control Group ()
1. Introduction
Osteoarthritis (OA) is the most frequently-encountered form of arthritis, and it is pathomorphologically characterized by focal loss of joint cartilage and marginal and central new bone formation. The knee is the main joint affected by the disease [1] . OAK is a serious health issue of the society, causing physical incompetency. The disease is most frequently seen among the aging and aged individuals.
Aging societies, increase in the prevalence of the disease, and lack of a definitive therapy to prevent progression of the disease, are all factors which contribute to the debilitating effects of the disease on the society. Better understanding of the pathophysiology of OA may aid the struggle to ease the devastating effects of the disease on one’s daily life.
OA was once thought to be just an end point of cartilage degeneration, but our current knowledge of the disease indicates that it is rather a general joint disease affecting almost all joint structures [2] . In OAK, structures including the cartilage, bone, bone marrow, ligaments, menisci, and the joint capsule, may all be affected during the disease process and in turn may even affect the course of the disease. Some specific findings like osteophytes are the early signs of OA. But unfortunately, conventional radiography is not very sensitive to OA. With the utilization of magnetic resonance imaging (MRI), it has been possible to detect some pathological changes in the knee joints of patients with suspected OA, whose conventional X-ray examinations had not revealed any abnormalities [3] .
In this study, a group of patients with osteoarhritis and another group comprising control individuals were comparatively investigated on the basis of their clinical and MRI findings. The quantimetric data used for comparison were as follows: leg lengths, knee circumferences, lateral femoral condyle diameters, medial femoral condyle diameters, intercondylar distances, tibial plateau heights, medial meniscus diameters, and lateral meniscus diameters.
2. Materials and Methods
29 patients, of whom 12 were males and 17 females, were included in this study. The patients had been referred to the Radiology Department from the outpatient units of the Departments of Orthopedics and Physical Therapy. All patients were diagnosed with osteoarthritis, in accordance with the European League Against Rheumatism (EULAR) criteria developed in 2009. Patients with known systemic diseases which might affect the skeletal system, together with patients who had previously undergone surgery of the knee joint, and those patients who demonstrated associating pathological conditions on their X-rays in addition to osteoarthritis, were excluded from the study. The control group consisted of 32 individuals, of whom 22 were males and 10 were females. The study was approved by the investigational ethics review board of the hospital and conducted in accordance with the principles of the Declaration of Helsinki. All of the patients and control individuals gave their informed consents prior to the study and before their MR examinations. All patients from the osteoarthritis group and all members of the control group were examined by MRI. MRI examinations covered the affected knees in the osteoarthritis patient group, and one or both knees of the members in the control group. All MRI studies were evaluated by the same radiologist. In both of the groups, certain clinical and MRI measurements were made. Clinical measurements included the leg lengths and knee circumferences, whereas MRI measurements comprised the following: lateral femoral condyle diameters, medial femoral condyle diameters, intercondylar distances, tibial plateau heights, medial meniscus diameters, and lateral meniscus diameters. The leg length and knee circumference measurements were made with the patient in the standing position, preceding the MRI examinations. MRI measurements were made on the associated axial or coronal sections, which demonstrated the optimally largest surfaces of the examined sites. The lateral and medial femoral condyle diameters, together with the intercondylar distances and tibial plateau heights, were measured on the coronal planes. Figure 1 shows the measurement of the long and short axes of the medial femoral condyle, while Figure 2 demonstrates the measurement of the intercondylar distance, on the coronal plane.
The diameters of the medial and lateral menisci were measured on the axial planes. All MRI examinations were conducted by a 0.2 T open MR system (Hitachi Airis Mate, Japan). The whole numerical data were assessed by the Statistical Package for Social Sciences (SPSS) v.15 program, and statistical evaluations were performed by the utilization of the t-test for Equality of Means, and the Receiver Operating Characteristic Test. The criterion for statistical significance of the t-test was p < 0.05.
3. Results and Discussion
There were 29 individuals in the patients, and 32 individuals in the control, groups. The mean age of the patient group was 48.0 ± 5.7 years, whereas the mean age in the control group was 27.8 ± 8.0 years. Of the 29 individuals who made up the patient group, 12 (41.4%) were males and 17 (58.6%) were females. The 32 individuals who comprised the control group were composed of 22 males (68.8%) and 10 females (31.3%). Of the 29 patients, 14 (48.3%) had his or her right knees, and 15 (51.7%) had his or her left knee, examined by MRI, whereas in the control group, half (50%) had their right, and the other half (50%) had their left, knees examined. The mean weight of the patient group was 76.5 ± 9.7 kg, whereas the mean weight of the control group was 69.3 ± 12.5 kg. The mean height was 168.7 ± 7.2 cm in the patient group, and 169.2 ± 7.8 cm in the control group. The mean leg lengths were found to be 47.8 ± 6.3 cm in the patient group, and 49.0 ± 8.2 cm in the control group. The mean values for knee circumferences were as follows: 41.0 ± 2.7 cm for the patient, and 40.1 ± 2.5 for the control, groups. The mean values for the lateral femoral condyle diameters were found to be 35.1 ± 4.0 mm and 27.8 ± 4.3 mm for the patient group, and 36.0 ± 5.6 mm and 28.4 ± 4.4 mm for the control group. The mean medial femoral condyle diameter measurements were 36.9 ± 4.1 mm and 27.9 ± 2.7 mm in the patients group, whereas they were found to be 38.3 ± 4.6 mm and 30.5 ± 3.9 mm in the control group. The mean intercondylar distance was 14.9 ± 3.2 mm in the patients, and 16.4 ± 2.2 mm in the control, groups. The mean tibial plateau height was found to be 5.4 ± 0.9 mm for the patient group and 5.6 ± 0.7 mm for the control group. The mean lateral meniscus diameters were 30.7 ± 2.4 mm and 26.8 ± 3.7 mm in the patient group, whereas they were 32.0 ± 3.7 mm and 27.6 ± 3.2 mm for the control group. The mean medial meniscus diameters were as follows: 37.8 ± 5.8 mm and 27.9 ± 3.8 mm for the patient group, and, 38.4 ± 4.3 mm and 28.4 ± 4.0 mm for the control group. All descriptives of the measured parameters of the patient and control groups are given at Table 1.
The Statistical Package for Social Sciences (SPSS) v.15 was utilized for statistical analyses, and for this purpose, the t-test for Equality of Means, and the Receiver Operating Characteristic Test, were processed. The criterion for statistical significance of the t-test was p < 0.05.
No statistically significant differences were found between the patient and control groups in terms of the following criteria: weight, height, leg length, knee circumference, lateral femoral condyle diameters, tibial plateau heights, lateral meniscus diameters, and medial meniscus diameters.
Statistically significant differences were found between the two groups in terms of the measurements of the second (short) diameter of the medial femoral condyle and the intercondylar distance (p < 0.05). In addition to these findings, the ROC curve analysis gave statistically significant results for both of these measurements. Concerning the second (short) diameter of the medial femoral condyle, a 28.0 mm cutoff value had a sensitivity of 75% and a specificity of 52% (p = 0.003; AUC = 0.723 (0.594 - 0.851)). For the intercondylar distance criterion, a cutoff value of 15.0 mm had a sensitivity and specificity of 70% (p = 0.007; AUC = 0.700 (0.561, 0.839)). The ROC curve analysis concerning these values is seen at Figure 3.
OA, the most common form of arthritis, is now understood to involve all joint tissues, with active anabolic and catabolic processes. KOA in particular is considered to be a largely mechanically-driven disease. As bone adapts to loads by remodeling to meet its mechanical demands, bone alterations likely play an important role in OA development. Subchondral bone changes in bone turnover, mineralization, and volume, result in altered apparent and material density of bone that may adversely affect the joint’s biomechanical environment [3] . This is why Ornetti et al. have concluded at the end of their study that OA modifies the motion patterns of the affected joints [4] .

Figure 1. Measurement of the long and short axes of the medial femoral condyle on the coronal plane.
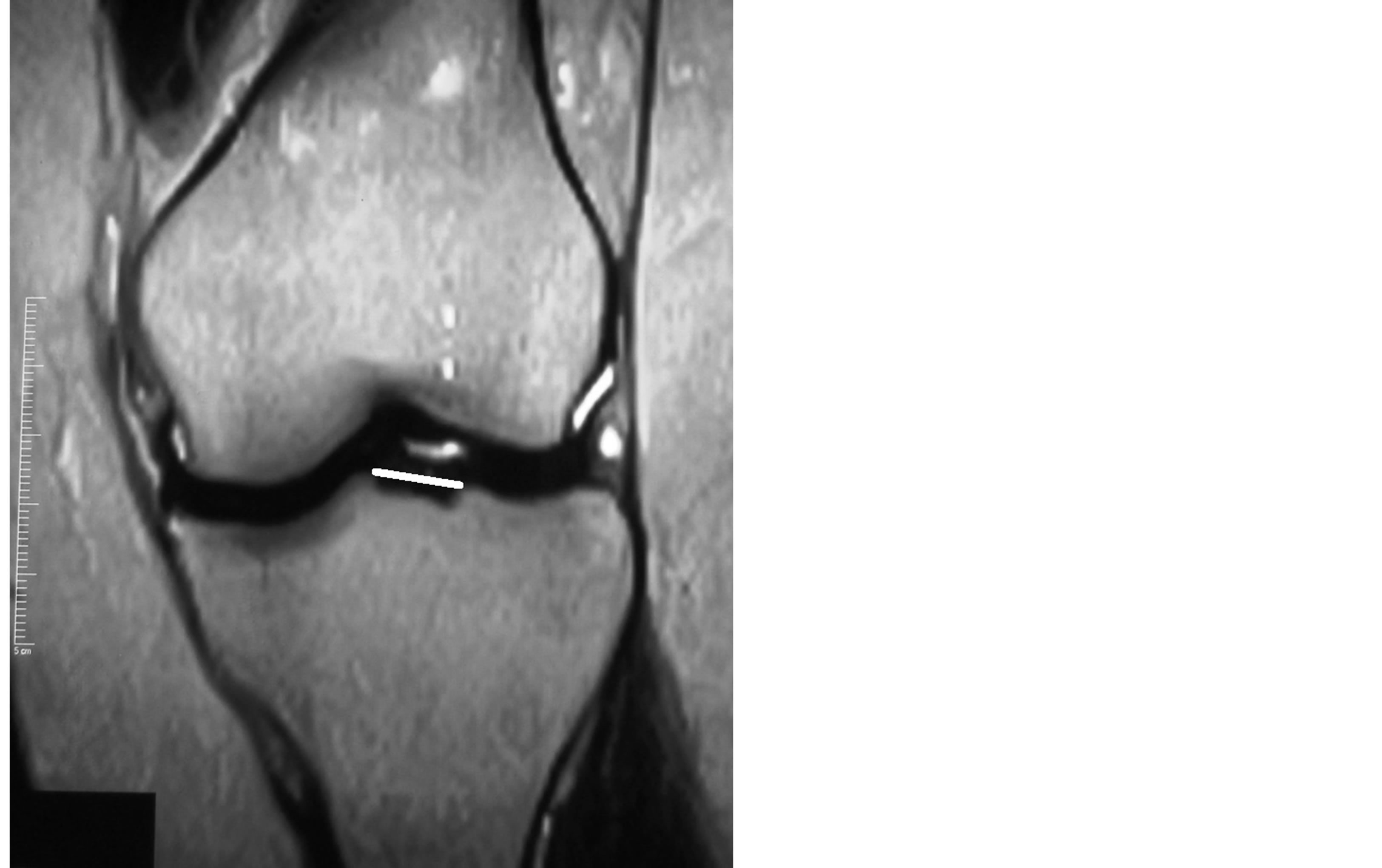
Figure 2. Measurement of the intercondylar distance on the coronal plane.

Table 1. The descriptives of the measured parameters of the patient and control groups.
(*)Significantly different for the two groups.
As mentioned above, OA is the most common form of arthritis, and KOA in particular is a leading cause of disability among older adults [5] [6] . With the aging of the population, the rising prevalence of obesity, and lack of definitive treatments to prevent the disease or halt its progression, the public health impact of OA continues to grow. A better understanding of the pathophysiology of OA and the development of more sensitive biomarkers is needed to identify and test rational treatment targets to reduce the burden of this common condition [3] .
While OA has traditionally been considered a disease of cartilage degeneration, it is being increasingly recognized as a disease of the whole joint involving all joint tissues [7] . Specific pathologic changes, such as osteophytes, the first definitive sign of radiographic OA, are a clear indication that bone changes occur in early OA. However, radiography is relatively insensitive in detecting the earliest changes. By using the advantages of MRI, it has become apparent that the majority of radiographically normal knees have some abnormality detectable on MRI. For example, in the Framingham Osteoarthritis Study, 88% of the knees without any evidence of radiographic OA (i.e. Kellgren and Lawrence grade 0), were shown to have at least one abnormality on MRI [8] . The joint cartilage is damaged in KOA, and this leads to the exposition of the bony surfaces that face the joint space. It is this exposition that leads to the pain in KOA.
Bone remodeling in the OA joint occurs preferentially in the subchondral plate. Surgical specimens from persons with OA have demonstrated that subchondral bone changes, including subchondral bone attrition, which is a flattening or depression of the subchondral bony surface unrelated to gross fracture, are common [9] . Many studies have been conducted in order to demonstrate and study the situation of the cartilage tissue of the knee joint in KOA. But the cartilage tissue is not the only tissue that undergoes changes during the course of KOA. Some bony changes, too, take place. There are some studies in the literature that have investigated these changes. Recent MRI studies have demonstrated increased tibial plateau size and alterations of the bone surface contour (subchondral bone attrition), even at the preradiographic OA stage [10] -[12] .
It has been hypothesized that cartilage loss is a mechanically mediated process that is more likely to occur in regions subjected to high stress; such areas of high stress are influenced by bone shape [13] . Pertinent to the recognition of the importance of biomechanics in knee OA, bone is known to be a dynamic tissue that adapts to loads by remodeling to meet its mechanical demands (Wolff’s Law) [14] [15] . Since alterations in joint geometry can affect load distribution and joint congruity, this can lead to maldistribution of biomechanical loads to previously relatively underloaded regions of cartilage and may contribute to cartilage breakdown [16] . The shift from thinking about OA as a degenerative disease of cartilage to one of a dynamic pathological process involving all of the tissues of the joint is an important step towards identifying treatment targets that can address the disease of the whole joint [17] .
In a study performed by Bredbenner et al., it was demonstrated that quantitative differences in tibia and femur geometry were observed between surface models based on clinical MRI data for subjects at risk of developing OA (i.e. incidence group) and control group subjects [18] .
The results of a study conducted by Cooke et al. suggest that variations in individual bone geometry may play a greater role in determining joint space geometry and underscore the importance of considering the geometry of the individual bones and other structures comprising the knee joint in advancing the understanding of KOA [19] .
Although there are controversial reports about the benefits of the use of MRI in detecting the bony and other structural changes in the knee joint affected by OA, it is obvious that the multiplanar imaging capability of MRI, together with its high-resolution demonstrative specificities, gives this imaging modality a superior place in the imaging of these alterations. For example, Kemp et al. concluded at the end of their study that although MRIdetected cartilage lesions, synovitis/effusion and loose bodies, did explain part of the muscle strength variability, their results suggested that MRI does not improve the link between joint degeneration and the clinical expression of KOA. The authors suggested that MRI contributes less than expected to the understanding of pain and function in knee OA and possibly offers little opportunity to develop structure-modifying treatments in KOA that could influence the patient's pain and function [20] . But in a study conducted by Phillips et al., it was stated that MRI imaging is a sensitive and early marker of OA that can correlate with drug efficacy [21] . It was also put in this study that MRI depicts the whole joint nature of the disease and serves as a barometer of its time course. Another study conducted by Hernandez-Molina et al. states that bone attrition detected by MRI may represent bone remodelling changes in response to mechanical stress [22] . Yusuf et al. report in their meta-analysis that MRI has been shown to be superior to plain films in the detection of alterations in the structures of the knee in KOA. The authors indicate that since MRI demonstrates the whole knee joint in a multiplanar fashion, it is a superior method in depicting these pathological changes. They also put out that knowing which structures in the knee are associated with KOA will add to our understanding of OA and, in the long term, will lead to rational therapeutic targets for OA. They point out that this will mean improvements in patient care, since at this moment the therapeutic options against OA are limited [23] .
Our aim in conducting this study was to look for measurable quantimetric changes in the bony tissues and menisci of the knee joint in OAK. In order to do this, two groups were assessed, one comprising OA patients, and the other comprising healthy control individuals.
Certain criteria were investigated in this study, including weights, heights, and leg lengths of the individuals, together with the following criteria concerning the MRI images of their knees: lateral femoral condyle diameters, medial femoral condyle diameters, intercondylar distances, tibial plateau heights, lateral meniscus diameters, and medial meniscus diameters. After obtaining these measurements, the values were compared statistically, utilizing the SPSS v.15 program. The t-test for Equality of Means were used for the comparisons, and p < 0.05 was appointed as the criterion for statistical significance. In addition to these, the Receiver Operating Characteristic (ROC) Test was utilized to search for a cutoff value to determine KOA.
No statistically significant differences were found between the patient and control groups in terms of the following criteria: weight, height, leg length, knee circumference, lateral femoral condyle diameters, tibial plateau height, lateral meniscus diameters, and medial meniscus diameters.
Statistically significant differences were found between the two groups in terms of the measurements of the second (short) diameter of the medial femoral condyle and the intercondylar distance (p < 0.05). In addition to these findings, the ROC curve analyses resulted with statistically significant outcomes for the measurements of both of these criteria. For the medial femoral condyle short axis measurement (p = 0.003), 28.0 mm was appointed as the cutoff value, and it had a sensitivity of 75% and a specificity of 52% (AUC = 0.723 (0.594 – 0.851)). The cutoff value for the intercondylar distance was 15.0 mm (p = 0.007), and it had a sensitivity and specificity of 70% (AUC = 0.700 (0.561, 0.839)).
It is well known that it is the medial aspect of the knee joint which bears most of the weight stress on the knee. That is why it is the medial meniscus which deteriorates the most during the process of KOA. In our study the second (shorter) diameter of the medial femoral condyle was found to be significantly less in the OA group, in comparison to the control group. This value was 27.9 ± 2.7 mm in the OA group, whereas it was 30.5 ± 3.9 mm in the control group. This alteration may be attributed to the degenerative process which takes place as a result of the OA process which directs most of the weight stress to the medial portion of the knee joint, and thus, the medial femoral condyle.
Another criterion which indicated an alteration due to the process of OA was the intercondylar distance. The mean value for this distance in the OA group was 14.9 ± 3.2 mm, whereas in the control group it was 16.4 ± 2.2 mm. The intercondylar distance was found to be significantly smaller in the OA group, in comparison to the control group. This alteration, too, may be attributed to the stress put on the tibial plateau during the process of OA.
Besides the t-test for Equality of Means, the Receiver Operating Characteristic Test was utilized to search for a cutoff value to determine the changes that take place during the process of KOA. The ROC curve analyses gave statistically significant results for the measurements of the second (short) diameter of the medial femoral condyle and the intercondylar distance. The 28.0 mm cutoff value for the medial femoral condyle short axis measurement (p = 0.003) demonstrated a sensitivity of 75% and a specificity of 52% (AUC = 0.723 (0.594, 0.851)). The other cutoff value was for the intercondylar distance and it was found as 15.0 mm (p = 0.007). This cutoff value had a sensitivity and a specificity of 70% (AUC = 0.700 (0.561, 0.839)). Although the study revealed these cutoff values, we are not fully confident as to draw a deterministic outcome from this result alone. But anyway, it might be wise to keep this data in mind as a significant indicator, because it is well known that it is the medial portion of the knee joint which deteriorates the most, during the process of OAK. New studies may be of help in evaluating this outcome. But when all these four statistically significant results that this study obtained are considered together as a unification of data, it is logical that together they point to the alterations at the tibial plateau and especially its medial aspect, together with the medial femoral condyle, due to the fact that it is this portion of the knee joint that bears the most of the weight stress and deteriorates the most as well.
4. Conclusion
One drawback of this study is the incongruence of the mean ages of the two groups. But although this may be seen as a disadvantage in the interpretation of the results, it must not be forgotten that KOA is a disease mostly of the later ages, and healthy volunteers for comprising control groups usually come from the younger population segments. As long as we were concerned, this was the best configuration of groups we could manage to create. Although the mean ages are not in great accordance, the results are pretty logical when the deteriorating effects of KOA which mainly affect the medial aspect of the knee, are considered. New studies will no doubt shed more light to this issue.
NOTES
*Corresponding author.