Inverse relationship between glomerular hyperfiltration and C-peptide level in Type 1 diabetes ()
C-peptide, cleavage product of insulin synthesis, is secreted from the islets of Langerhans together with insulin. In the eighties, it was suggested that C-peptide may influence biological functions [6]. It has been shown that C-peptide, at physiological concentrations, reduces glomerular hyperfiltration mainly via constriction of the afferent arteriole, dilatation of the efferent arteriole, and inhibition of tubular Na+ reabsorption [7].
The relationship between GFR and C-peptide level at diagnosis of Type 1 diabetes has been understudied in children and adolescents. By studying GFR, C-peptide level and other parameters in a large population of young Type 1 diabetic patients, we tested the hypothesis that this relationship is true also in children.
2. METHODS
2.1. Subjects
Between 1995 and 2013, five hundred thirty-nine patients were diagnosed for diabetes at the Diabetology Clinic of the University Children’s Hospital Queen Fabiola in Brussels. Inclusion criteria were patients with Type 1 diabetes (509) and without other pathology (495). All data were collected during the first week after diagnosis of Type 1 diabetes.
2.2. Measurements
GFR was determined by single bolus intravenous injection of 51Cr-EDTA. Blood samples were taken at 90, 150 and 210 minutes and the non-compartemental Russell method was used [8]. Glycated hemoglobin (HbA1c) was measured by ion exchange, high-performance liquid chromatography, DCCT aligned (normal value < 6.0%). C-peptide level was measured on a chemi-luminescence analyzer Advia Centaur. Body weight and height were measured. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared and converted to standard deviation scores (SDS) based on the 1990 English references [9]. The loss of weight at diagnosis was expressed in percentage of body weight.
2.3. Statistical Analysis
Data were reported as mean (95% IC) for normally distributed values or as median (interquartile range) for nonnormally distributed values. The Mann-Whitney U test was used to test for the difference between median GFR in the 495 diabetic patients and the normal institution reference values and the difference between genders. Linear regression analysis was used to test for the associations between GFR and HbA1c, C-peptide level, age, BMI SDS and the loss of weight at diagnosis. Multiple linear regression analysis with GFR as the dependent variable was used to assess independent relationships. P ≤ 0.05 was considered to be significant.
3. RESULTS
The clinical characteristics of the study population are listed in Table 1. In the 495 patients, median age was 8.2 (4.7 - 11.6) years. There were 231 females and 264 males. GFR (Figure 1) was increased: in children aged less than 12 years [157.0 (134.0 - 179.7) ml/min/1.73m2 vs normal values 127.0 (109.1 - 147.3) ml/min/1.73m2 (p < 0.001)]; in girls aged more than 12 years [151.7 (121.8 - 171.5) ml/min/1.73m2 vs normal values 117.0 (102.2 - 133.0) ml/min/1.73m2 (p < 0.001)] and in boys aged more than 12 years [138.6 (123.5 - 159.7) ml/min/1.73m2 vs normal values 130.7 (109.2 - 149.1) ml/min/1.73m2 (p = 0.002)] (Table 2). In 36% of the patients, GFR was superior to upper normal limit (mean + 2 SD). There were no significant difference between males and females. GFR was significantly negatively correlated with age (p < 0.001, Figure 2) and C-peptide level (p = 0.001, Figure 3), and positively correlated with weight loss at diagnosis (p = 0.02). There was no significant correlation with gender, HbA1c and BMI SDS.
Variables entered into the multiple regression analysis (Table 2) were age, C-peptide level and weight loss at diagnosis. Age (p = 0.001) and C-peptide level (p = 0.05) were independently and negatively related to GFR.

Table 1. Characteristics of the study population.

Table 2. Glomerular filtration rate.

Figure 1. Glomerular filtration rate in the study population: GFR was superior to upper normal limit in 36% of the patients.
4. DISCUSSION
This study focused on the relationship between Cpeptide level and GFR at diagnosis of Type 1 diabetes in a large population. We confirm the glomerular hyperfiltration in young Type 1 diabetic patients. Higher the GFR, younger the age and lower the C-peptide level are. This hyperfiltration is independent of gender, BMI and HbA1c.
Young age and low C-peptide level are bound to a faster course of β cell destruction [10]. Therefore, hyperglycemia could be more important which could explain
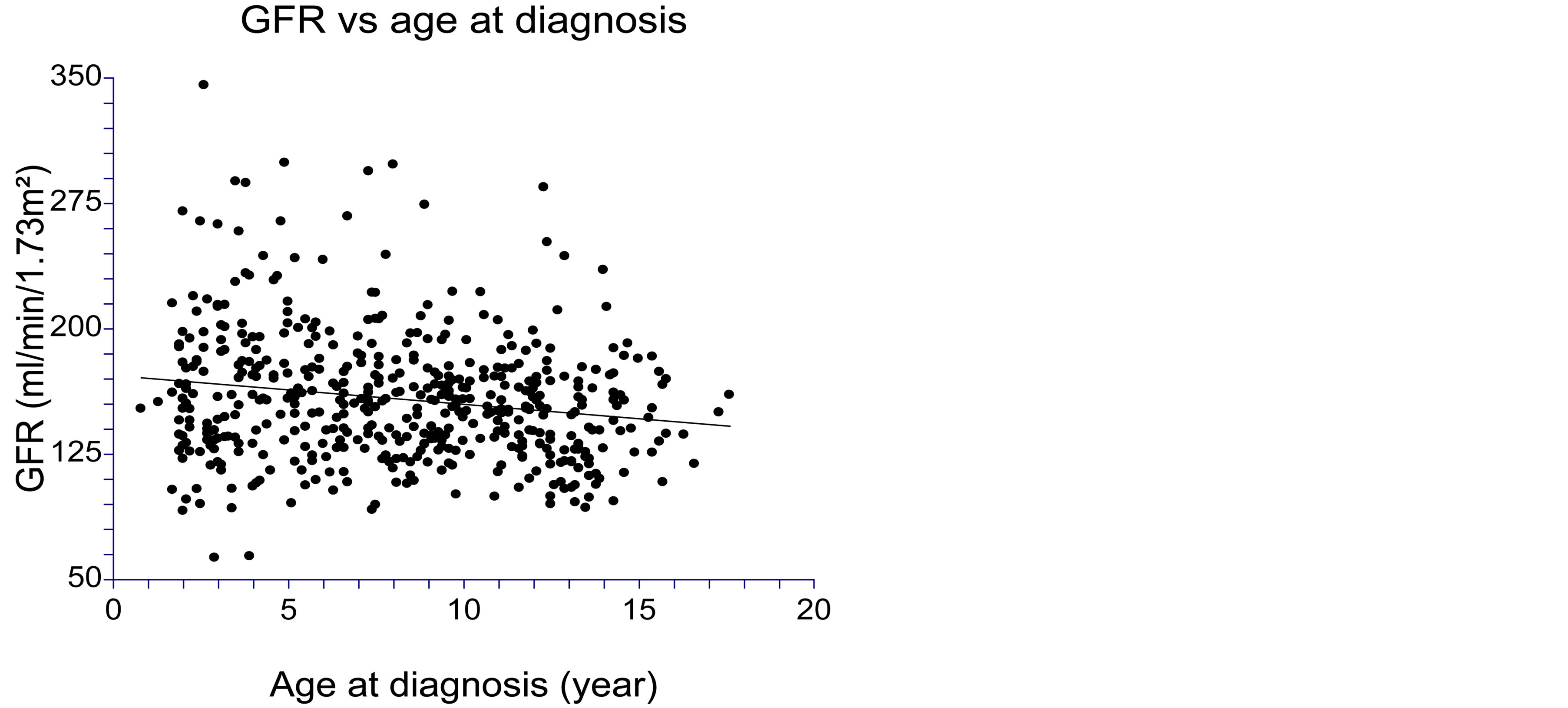
Figure 2. Glomerular filtration rate (GFR) was significantly negatively correlated with age at diagnosis at diagnosis (p < 0.001).

Figure 3. Glomerular filtration rate (GFR) was significantly negatively correlated with C-peptide level at diagnosis (p = 0.001).
part of the increased GFR. The lack of relationship with HbA1c could reflect that HbA1c is an index of mean blood glucose over more or less 120 days.
Acute hyperglycemia is known to increase GFR in normal and Type 1 diabetic patients [11,12]. It has been largely shown that the initial hyperfiltration normalized with good glycemic control [13,14]. Nevertheless, published studies reported that individuals with hyperfiltration were at increased risk of progression to diabetic nephropathy [15]. GFR at diagnosis could be a predictor of overt diabetic nephropathy, even in children. Glomerular hyperfiltration may play a crucial role in the subsequent development of diabetic nephropathy and thus represent potential therapeutic targets in the prevention of diabetic nephropathy.
We demonstrated that this hyperfiltration is associated with low C-peptide in children and adolescents. Studies have demonstrated a series of physiological effects of the C-peptide itself [16,17]: although the mechanisms are not fully understood, a hormonal therapeutic role of C-peptide as an active protective factor for the diabetic kidney should be considered. For example, beneficial effects of C-peptide on glomerular hyperfiltration and urinary albumin excretion have been shown [18,19]. C-peptide administrations could become a preventive treatment for the diabetic nephropathy.
This study has a solid base of 495 young patients. However, there were no healthy controls. Moreover, this cross-sectional study does not allow clarifying whether hyperfiltration at diagnosis predicts the development of later nephropathy.
A longitudinal long-term follow-up, during many years, should be necessary to analyze the eventual role of glomerular hyperfiltration at onset of Type 1 diabetes, associated with lowest C-peptide level in the development of later nephropathy. The early increased glomerular filtration may play a crucial role in the development of diabetic nephropathy and inhibition of the diabetesinduced hyperfiltration has been shown to have beneficial effects, delaying the progression of kidney damage [20].
Several studies have shown that administration of physiologically relevant doses of C-peptide reduces diabetes-induced glomerular hyperfiltration, decreases albuminuria, reduces renal hypertrophy and normalizes glomerular volume [7,18,19]. However, the effects of C-peptide administrations on kidney function need to be evaluated.
ABBREVIATIONS
BMI—Body mass index, GFR—Glomerular filtration rate, HbA1c—Glycated hemoglobin, SDS—Standard deviation score