Factors determining operative reduction in intussusception in children aged less than fourteen years ()
1. INTRODUCTION
Intussusception is a common cause of abdominal pain and bowel obstruction in children. Most of these intussusceptions are considered idiopathic in origin as there is usually no identifiable pathology. The underlying cause of intussusception in most infants is unknown, but has been associated with several pathogens, including adenoviruses [1-10].
Although the etiology of intussusceptions remains unclear, adenovirus infection has been associated with an increased risk of intussusceptions. Only about 6% of patients (range, 1.5% to 12%) have intussusceptions, which are associated with a pathologic defect, primarily Meckel’s diverticulum [11]. Most episodes of intussusception, termed “idiopathic”, arise in the ileum because of lymphoid hyperplasia of Peyer’s patches, [12], suggesting a response to infection. An infective etiology is further suggested by the presence, in about 50% of children with intussusception, of viral shedding in the stools, together with the demonstration of virus particles in pathologic specimens [13].
Although intussusception remains the most common cause of acute intestinal obstruction in infants and young children, it was found to be a side-effect of a vaccine administered to infants in the USA in 1998 for the prevention of rotavirus gastroenteritis. This resulted in a global need to determine the incidence of intussusception before the introduction of new rotavirus vaccines [14].
Children with intussusceptions in developed countries are likely to experience a favorable clinical outcome because of timely diagnosis and early treatment with the less invasive procedure of enema reduction. By contrast, in developing countries, delayed diagnosis with ensuing bowel necrosis, followed by attempted operative reduction, has been associated with high fatality rates, e.g., 18% in Nigeria, 20% in Indonesia and up to 54% in Ethiopia [15].
The treatment of intussusception has evolved from primarily operative management to radiologic reduction with either air or barium contrast. Radiologic reductions of intussusception have been found to decrease the length of hospitalization, shorten recovery time, and reduce the risk of complications associated with major abdominal surgery. The average success rate of radiologic reduction is 80%, but it varies widely [16].
This retrospective analysis evaluated the factors associated with operative reduction of intussusceptions, in contrast to enema reduction alone without the need for surgical intervention, in children aged <14 years.
2. METHODS
The medical records of all children aged <14 years hospitalized at Hamad General Hospital, Doha, Qatar, from January 2002 through December 2012 were reviewed. Patients who met the definition for intussusception, as determined by the Brighton Collaboration, were identified using the ICD-9 diagnosis code 560.0. Patients were included if the diagnosis of intussusception was verified by imaging (ultrasound, enema, and/or computed tomography [CT]) or surgical exploration. Patients were excluded if their records could not validate the diagnosis of intussusceptions.
For each identified child, we extracted information on demographics, admission and discharge dates, clinical signs and symptoms and their duration, and diagnostic and treatment procedures. Data were summarized on standardized questionnaires entered into an electronic database and checked for accuracy; data extraction and entry were performed by the same investigator.
Clinical outcomes were analyzed relative to patient age, sex, clinical signs, date of hospitalization and diagnostic and treatment related characteristics. Because early diagnosis and treatment could provide better outcomes, we compared the length of hospital stay of patients admitted <24 hours and ≥24 hours after the onset of symptoms.
Incidence rates were calculated by using census data, and ratios with 95% confidence intervals were calculated using Poisson regression data.
All radiologic reduction techniques were performed under fluoroscopic guidance using liquids, with the number of reduction attempts at the discretion of individual radiologists. Patients were usually in the prone position, although the supine and oblique positions were also utilized. Conscious sedation was not utilized. A rectal catheter was inserted into each patient, and the buttocks were taped to prevent contrast leakage. Liquid reduction was attempted using either barium or water-soluble diatrizoate meglumine (Gastrografin), prepared by routine methods. A column of contrast was established 1 meter above the table. Typically, 3 consecutive attempts of 3 minutes each were performed.
Descriptive statistics were used to summarize the demographic characteristics of patients. Results are reported as mean ± standard deviation or medians and inter-quartile ranges.
3. RESULTS
3.1. Patient Characteristics
Review of the medical records of our center identified 141 children aged <14 years who were diagnosed and treated for intussusceptions over the 11-year study period. These patients included 83 boys and 58 girls (ratio, 1.4:1). Of these 141 patients, 47 (31.7%), of mean age 13.6 months, underwent operative management and 96 (68.3%), of mean age 14.0 months, underwent enema reduction.
3.2. Delay in Presentation and Symptoms
Delay in presentation did not decrease the success of radiologic reduction. The rate of operative intervention was lower in patients who presented <24 hours than in those who presented ≥24 hours after symptom onset (22.2% vs. 41.5 %; Table 1).
Symptoms were similar in patients managed with enema and operative reduction (Table 2).
3.3. Length of Stay
Length of stay ranged from 1 to 7 days (mean, 2.6 days). Length of stay was longer in patients who underwent operative than enema reduction, both in patients who presented <24 hours and ≥24 hours after symptom onset (Table 3).
3.4. Coexisting Conditions
Generally speaking, the number of coexisting conditions was greater in patients managed with enema reduction than in those who needed surgical intervention (Table 4).

Table 1. Duration of symptoms in patients managed surgically or with enema reduction.
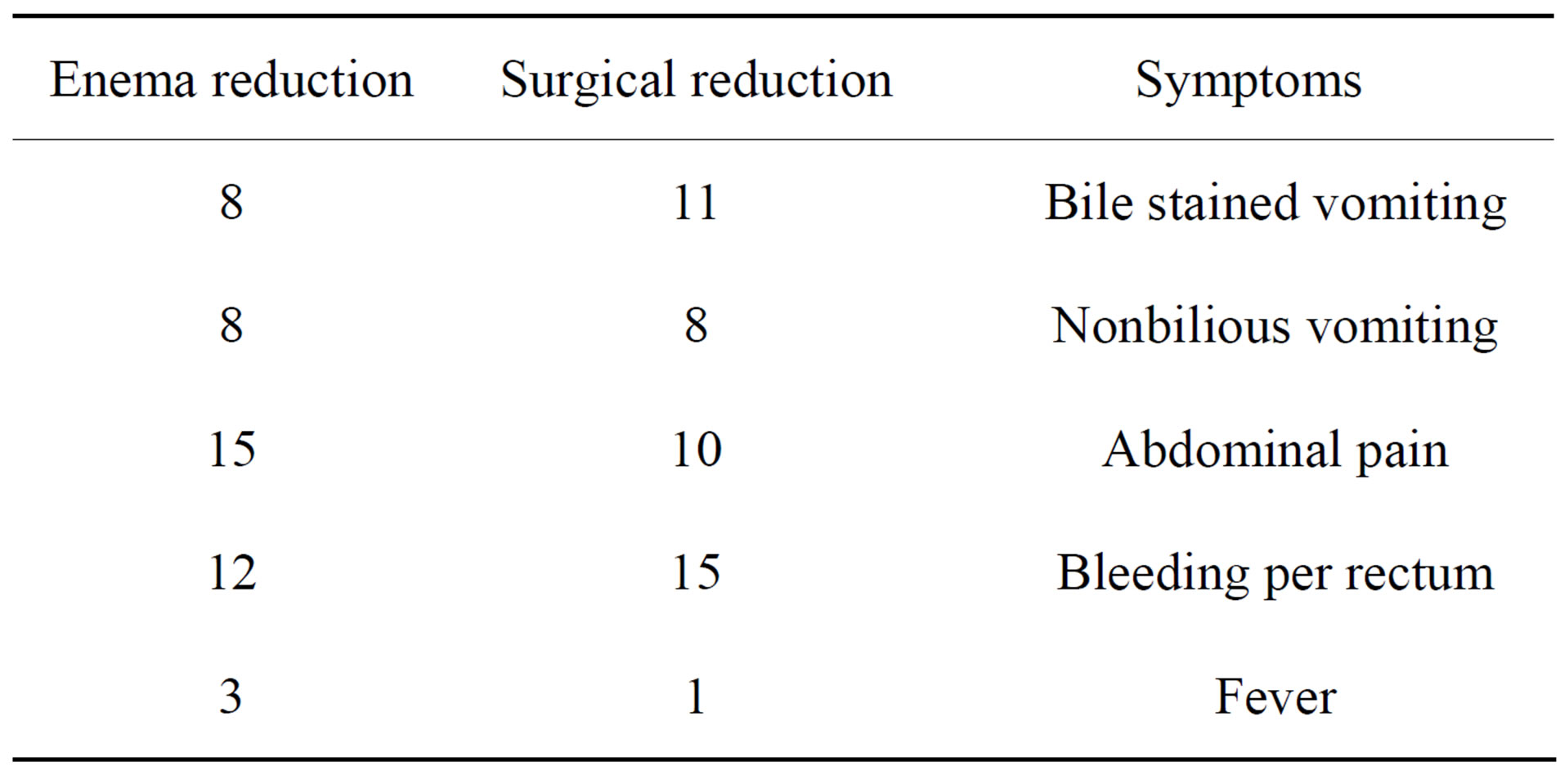
Table 2. Symptoms in patients managed surgically and by enema reduction.

Table 3. Lengths of stay in patients managed with enema reduction and operatively.

Table 4. Coexisting conditions in patients managed surgically and with enema reduction.
3.5. Presence of Free Peritoneal Fluid on Ultrasound
Peritoneal fluid was present in 10 patients (9%) who required only enema reduction and in 7 (16%) who required surgical intervention.
3.6. Recurrent Intussusceptions
Three patients experienced recurrences, with all three managed with enema reduction only.
4. DISCUSSION
Intussusception is a common childhood problem worldwide, with high rates of morbidity and mortality. In developing nations, the mortality may be as high as 20%. [11]
Nonoperative reduction of intussusceptions, performed by a radiologist using hydrostatic or pneumatic pressure under fluoroscopic or sonographic guidance, is usually successful. Nonoperative reduction has been shown to reduce length of hospital stay, shorten recovery time, decrease hospital costs, and decrease the risk of complications related to abdominal surgery [17]. The success rate of enema reduction has been found to vary widely, usually averaging 75% [18,19]. In our series, however, the success rate was somewhat lower, 68.7%.
Studies have reported that the median ages of children requiring operative and non-operative reduction were similar (0.7 years [0.4, 2.5 years] vs 0.9 years [0.5, 2.0 years]), although children aged 1 to 2 years were less likely to require operative reduction [11]. We found that children who underwent operative reduction were less likely to have a coexisting condition associated with intussusceptions, in contrast to previous findings.
Operative reduction has been associated with a longer length of hospital stay, especially when bowel resection was performed. This results in higher hospital costs, as well as inefficient use of health care resources. In addition, the need for laparotomy increases morbidity rates, pain, and long-term risks of adhesive bowel obstruction. Rarely, a delay in diagnosis may lead to bowel necrosis and overwhelming sepsis, a potentially lethal condition [19]. Studies have shown that 6% to 53% of children require surgical reduction, including children who fail enema reduction and those with contraindications to enema reduction [13,20-23].
Although intussusception is a common surgical condition in children, there are no current guidelines in Qatar regarding the treatment of children with this condition. Duration of symptoms did not affect patient outcomes, with the percentage of patients having symptoms <24 hours being lower in patients requiring surgical intervention.
Over the last two years, however, attempts have been made to standardize the referral system for children with intussusception. Patients suspected of having this condition are sent to the Pediatric Emergency Centre (PEC) from different regions throughout the country for ultrasound examination. Moreover, these patients are immediately evaluated by the on-call pediatric surgeon, with patients confirmed to have intussusceptions by ultrasound admitted to the hospital. Hydrostatic reduction is scheduled as soon as possible, to be performed by the same radiologist who performed the ultrasound. Nevertheless, it is impractical to refer all children with abdominal pain and vomiting to the radiology department of the main hospital in the country and to initiate this protocol. Thus, our results should stimulate efforts toward educating community-based physicians about the diagnosis and management of intussusception.
Although the presence of free peritoneal fluid on ultrasound was regarded as prognostic of a higher rate of failure of enema reduction, we found that free peritoneal fluid was present in 16% of patients requiring surgical intervention, compared with only 9% of patients who underwent successful enema reduction. Similarly, recurrent intussusception was not an indicator for surgical intervention.
This study had several limitations, including its retrospective design. Moreover, it was difficult to obtain accurate birth-cohort data for the catchment population. Nevertheless, the strength of this retrospective study was its analysis of patients treated at the only tertiary care facility in the country, with complete evaluations and reliable documentation.
5. CONCLUSION
In conclusion, this report, describing our 11-year experience of intussusceptions in Qatar, provides accurate baseline data. We found that a delay in presentation did not decrease the success rate of radiologic reduction and did not increase the risk of operative intervention and bowel resection.
NOTES
#Corresponding author.