Adjuvant Therapy on Cancer of the Lower Rectum. Evaluation of the Effects of Preoperative Radiotherapy on the Prognosis of Patients with Cancer of the Lower Rectum ()
1. Introduction
Pre-operative radiotherapy as complementary to surgery, although recognized as effective on controlling the interval-free of rectal cancer, has not been utilized as frequently as expected [1-11].
Several aspects are responsible for this [2-39] but the most important is that there is no world consensus about:
1) The total tumor dose, and the daily dose;
2) Short or long radiotherapy;
3) The target volume;
4) The interval between the completion of the irradiation and surgery;
5) Effects of irradiation on surgery;
6) Which tumor needs irradiation;
7) The effectiveness of preoperative radiotherapy on long-term survival rate.
Nowadays, however, some authors have demonstrated that the association of neo-adjuvant therapy (radiotherapy or radio-chemotherapy) to surgery can improve the interval-free of cancer and alter the long-term survival rate [7,13,24-32].
Preoperative radiotherapy in cancer of the lower rectum has been used since 1975. Previous works defined the target volume and the total tumor dose [27,29]. Analyzing the results obtained in a previous randomized prospective trial [28], it was concluded that the use of preoperative radiotherapy is able to:
• Decrease, significantly, the number of undifferentiated cells;
• Diminish the grade of tumor invasion in the rectal wall;
• Reduce, statistically, the incidence of local recurrence
• Alter long-term survival rate.
In this trial, two groups of patients, randomly allocated, with cancer of the lower rectum were treated surgically following the same oncological parameters, but differing in the use of preoperative radiotherapy in one of the groups. However, frustrated criticism came from the small number of patients (68 patients) involved in the study.
Since then, the number of patients treated by preoperative radiotherapy has risen and the results obtained have been equally registered.
Some new aspects emerged from this prospective study.
The results obtained as to:
• The comparison of the biopsies taken before and after the radiotherapy;
• The evaluation of the cellular undifferentiation and of the Broders’ classification;
• The tumor volume measured before and after radiotherapy by endorectal ultrasound;
• The wall infiltration measured before and after radiotherapy by endorectal ultrasound;
• The analysis of the correlation of these results with the incidence of local recurrence;
• The percentage of long-term survival rate;
have given new insight into the concept of preoperative radiotherapy in patients with cancer of the lower rectum.
2. Methods
From 1978 to 2008, a total of 538 patients with cancer of the lower rectum were submitted to preoperative radiotherapy and all of them had a 5-year follow-up. In this study only patients with rectal adenocarcinoma situated in the lower rectum were included.
There was no gender, race and age distinction.
All patients with tumors located between the pectinate line and 4 cm above it, were submitted to abdominoperineal excision and those with tumors situated between 5 and 10 cm, were treated by a colon-anal stapled anastomoses.
Of the 538 patients, 408 (75.8%) were operated on laparoscopically.
Preoperative dosage of CEA, gamma GT, colonoscopy and abdominal ultrasound were performed in all the patients to stage the tumor. Endorectal ultrasound was performed in 200 patients, size and infiltration of the tumor were thus evaluated before and after the irradiation.
Every patient had biopsies (10) of the tumor taken at the time of the diagnosis and another one after the completion of the radiotherapy, at surgery. The number of undifferentiated cells were exhaustively noted and the results compared, in both biopsies.
Broders’ classification was equally observed and the results obtained, before and after radiotherapy, registered and compared.
Proctoscopy and digital examination were performed at diagnosis and after the end of the irradiation treatment, immediately before surgery, to evaluate tumor extension and wall infiltration.
Preoperative radiotherapy was performed according to the following scheme:
200 cGy/daily for 4 consecutive weeks up to a total of 4000 cGy, by means of a Linear Megavoltage Accelerator (25 MeV), in anterior and posterior pelvic fields. Surgery was performed 7 to 10 days after the conclusion of the radiotherapy.
Postoperative protocol included periodical examination:
• Every 3 months for the first two years, after surgery. Digital examination (or careful perineal palpation) and evaluation of the CEA were performed each time.
• Every 6 months for the next consecutive three years.
Abdominal ultrasound was performed yearly and colonoscopy every 2 or 3 years.
When clinical assessment suggested local or general recurrence, a CT scan or MR was accomplished.
It was considered local recurrence the appearance of perirectal, perineal or anastomotic metastasis.
Pelvic recurrence (bladder, prostate or ovarian) was considered generalized recurrence.
3. Results
Biopsy
Cellular undifferentiation. At diagnosis the tumors were classified as:
286 tumors (53.3%)èhigh grade of cellular undifferentiation181 tumors (33.5%)èmoderate grade of cellular undifferentiation71 tumors (13.2%)èlow grade of cellular undifferentiation.
After the radiotherapy, at surgery, the tumors were classified as:
87 tumors (16.2%)èhigh grade of cellular undifferentiation299 tumors (55.6%)èmoderate grade of cellular undifferentiation152 tumors (28.2%)èlow grade of cellular undifferentiation (Figure 1).
Broders’ classification: At diagnosis the tumors were classified as.
48 (8.8%)→Broders’ I
142 (26.5%)→Broders’ II
206 (38.3%)→Broders’ III
142 (26.5%)→Broders’ IV.
At surgery, after irradiation therapy, the tumors were classified as:
126 (23.5%)→Broders’ I
301 (55.9%)→Broders’ II
95 (17.6%)→Broders’ III
16 (2.9%)→Broders’ IV (Figure 2).
Of the 142 patients considered as Broders IV at diagnosis, 88.2% of them changed to a different classification: 52.6% changed to Broders II, 30,3% modified to Broders I (Figure 3).
Endorectal ultrasound: The endorectal ultrasound (ERUS) evaluation in 20 patients, comparing tumor size before and after radiotherapy (Figure 4), showed that:
■ In 40 patients (20%) the tumor was reduced to a small superficial ulcer;
■ In t120 patients (60%) the tumor receded between 60% to 75%;
■ In 40 patients (20%) the tumor receded between 20% to 30%.
Gross and endoscopic tumor involution: digital evaluation allows recognition of a tumor reduction in all the patients. In 166 patients (31%) the tumor mass receded more than seventy percent of its initial size.
Endoscopically almost all the exophytic tumors were converted into small ulcers or to a whitish pale fibrosis zone. The majority of the ulcer-vegetating tumors after irradiation looked like a large superficial necrotic ulceration.
According to Dukes’ classification, the tumors at surgery were classified as (Figure 5):
58 (10.6%)→Dukes A
290 (53.9%)→Dukes B and
190 (35.5%)→Dukes C.
Of the classified Dukes A tumors, 10 (2.9%) were classified as microscopic tumors.
Local Recurrence: of the 538 patients only 16 (3.0%) had a diagnosis of isolated local recurrence confirmed at the follow-up. Of them, 8 (50%) died of cancer in the first two years after surgery (Figure 6).
Generalized Recurrence: of the patients with a 5-year follow-up, 83 (15.6%) patients presented widespread recurrence:
36 (44.4% of the 83)→lung metastasis
26 (31.1% of the 83)→ liver
13 (15.5% of the 83)→disseminated peritoneal recurrence
08 (8.9% of the 83)→pelvic recurrence.
Long-term follow-up: of the 538 patients, 101 (18.9%) had a 15-years follow-up.
Of the 538 patients with a 5-year follow-up (Figure 7):
230 (80.1% of the 287 patients) were alive, with no signs of recurrence disease
53 (18.5% of the 287 patients) died of cancer
45 (15.7% of the 287 patients) died with generalized

Figure 2. Broders’ classification before and after radiotherapy.

Figure 3. Modification observed in Broders IV patients after irradiation.
recurrence
08 (2.8% of the 287 patients) died with local recurrence
04 (1.4% of the 287 patients) died of other causes.
4. Discussion
Preoperative irradiation for cancer of the lower rectum has been the object of controversies, specially when survival is discussed [2,5,8,9,11,13,15-18,20,21,24-27,30-3436-39] and only a very few randomized statistic papers are able to demonstrate better long-term results [28,35].
Recurrence, especially local recurrence, is responsible for the great majority of deaths in the first two years after surgery [1,7,19]. It is well recognized that the incidence of local recurrence is a direct consequence of the proportion of undifferentiated cells and of the tumoral invasion of the bowel wall [1,7,12,19]. Less undifferentiated and less invasive tumors tend to have better prognosis [19,22, 23,29]. So, hypothetically, any treatment that can reduce

Figure 4. Endorectal ultrasound before and after radiotherapy in 200 patients.
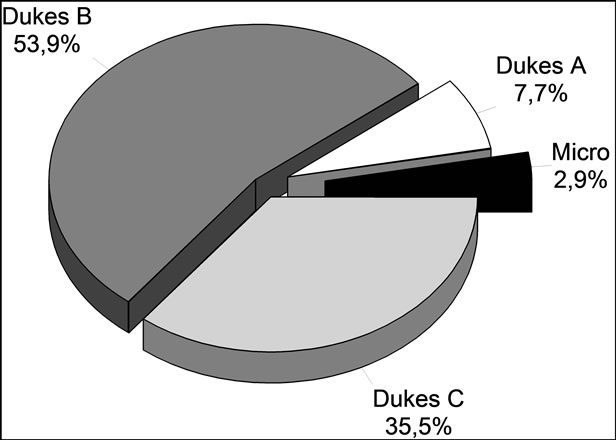
Figure 5. Dukes classification of the tumors after irradiation.

Figure 6. Incidence of local recurrence.
the number of undifferentiated cells will affect the incidence of local recurrence and will certainly increase the long-term survival rate.
In our series the comparison between biopsies taken before and after irradiation showed a very important re-
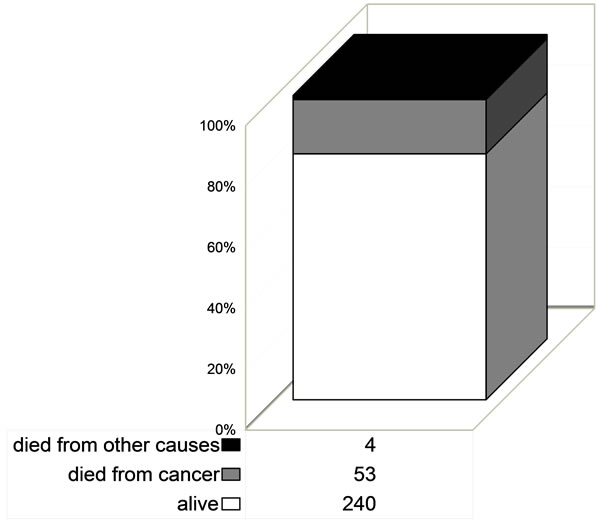
Figure 7. Deaths of patients with 5-year follow-up.
duction in the number of carcinomatous (undifferentiated) cells, statistically increasing the number of differentiated cells.
As a fact, the variation in the number of undifferentiated cells before and after irradiation was significantly proved; the number of tumors with a high grade of undifferentiated cells shows a negative variation after irradiation: 191 (53.3%) patients at diagnosis and 58 (16.2%) patients after radiotherapy, showing a significant statistical reduction in the number of undifferentiated cells (Figure 1).
At the same time, as a corollary, the number of tumors with a low grade of differentiated cells at diagnosis shows an effective increase after irradiation: of 47 (13.2%) patients at diagnosis to 101 (28.2%) patients after irradiation, with a positive variation.
The real significance of this fact is that the preoperative radiotherapy reduced the number of undifferentiated cells, enough to invert the prognosis of local recurrence.
Broders’ classification, in the same biopsy study, revealed a similar aspect: there was a significant statistical reduction in the number of undifferentiated cells. Patients with Broders IV at diagnosis changed to Broders III, II and even I after the irradiation (Figure 3):
05 tumors Broders’ IV (5.3%) became Broders’ III.
50 tumors Broders’ IV (52.8%) changed into Broders’ II.
29 tumors Broders’ IV (30.3%) were reduced to Broders’ I.
11 tumors Broders’ IV (11.8%) were resistant to radiotherapy.
As a matter of fact, the reduction in the number of undifferentiated cells because of preoperative radiotherapy had a significant influence in the incidence of local recurrence.
It is important to notice that the great majority of patients with local recurrence occurred exactly in those patients with tumors considered as resistant to irradiation: patients with high grade of undifferentiated cells at diagnosis that persisted as high grade of undifferentiation at surgery.
Of the 11 patients observed with local recurrence:
• 9 (81.8% of the 11 patients) were Broders’ IV, all of them classified as resistant to irradiation; 8 of them died postoperatively in the first 18 months after surgery and one with anastomotic recurrence underwent an abdomino-perineal excision with a satisfactory response;
• 2 patients were Broders’ IV at diagnosis, reduced to Broders’ III after radiotherapy: one with anastomotic recurrence was submitted to an abdomino-perineal excision with satisfactory response and one underwent a local excision plus with a new radiotherapy treatment.
But the most important fact was that all the 11 patients with local recurrence were classified, at the time of the diagnosis, as having tumors of a high grade of cellular undifferentiation and this cellular aspect was not reduced with radiotherapy. These patients were considered to have radio-resistant tumors.
Generalized recurrence occurred in 45 patients:
• One patient had a tumor classified as Broders’ IV at diagnosis which did not change after radiotherapy;
• 44 (97.7%) had tumors which were classified as having a high grade of cellular differentiation at the time of diagnosis and this cellular aspect did not change after radiotherapy.
All patients with recurrence (56 patients from 358) belonged to the group with high grade of cellular undifferentiation that did not respond to the irradiation treatment: radio resistant tumors.
• 11 (3.0% of the 358 patients) had local recurrence;
• 37 (10.33% of the 358 patients) acquired widespread metastasis.
• 8 (2.2% of the 358 patients) had concomitant metastasis (local and general).
• Those tumors were classified as resistant to irradiation.
Long-term survival rate (5 year follow-up) was of 83.6%: 240 patients out of 287 were alive with no clinical evidence of recurrence after 5 years.
Only 8 patients out of the 11 with local metastasis died of cancer.
Besides the observed fact of a low incidence of local recurrence (3.0%) in irradiated patients, it was also observed that not all the patients died in the first 2 years of follow-up: 27.2% of the patients with local recurrence were alive after a 5 year follow-up. The percentage of deaths with local recurrence was of 2.23%: eight patients in 358.
It is logical to conclude that the irradiation effect, diminishing the number of undifferentiated cells, not only decreased the local recurrence rate but also reduced the mortality rate in this kind of recurrence.
Nonetheless, as mentioned above [1,7,12,19,22-27,35], the incidence of local recurrence depends also on the tumoral infiltration of the rectum wall.
The results observed in this study confirmed that after the irradiation an involution of the tumor size and volume occurred, detectable not only by endorectal ultrasound (ERUS) in 20 patients, but also by digital and endoscopic examinations.
So, it is questionable to confirm, but logical to say, that besides the proven reduction in the number of undifferentiated cells, preoperative irradiation also produces a diminishing of the carcinomatous infiltration of the rectal wall. In a previous study [28], analyzing the results of a randomized analytical trial, comparing two groups of patients with cancer of the lower rectum (adenocarcinoma between the pectinate line and 10 cm above it), one of them submitted to preoperative radiotherapy plus surgery and the other one submitted only to surgery, this fact was also noted on.
In the group submitted to preoperative radiotherapy there was an increased number of B Dukes tumors.
Classifying the tumors observed at diagnosis and after radiotherapy, at surgery, according to cTNM classification it was observed a down-staging in all the patients:
• In 76% of the patients there was a reduction of 20% to 70% of the initial tumor volume;
• In 24% of the patients there was a reduction of 71% to 90% of the initial tumor volume;
• In 2.9% of the patients there was a reduction of the initial tumor to a microscopic lesion.
Undoubtedly, both radiation therapeutic effects—reducing the number of undifferentiated cells and diminishing the tumor volume and the carcinomatous infiltration of the rectal wall—are responsible for the reduction of the local recurrence rate and for a better prognosis of long-term survival rate.
Besides these effects one more very important aspect was noted on: the number of pT3 with negative lymph nodes carcinomatous invasion decreased. Nevertheless, when lymph nodes invasion was detected in patients with pT3 tumors, only less than one third of them showed cancer. In reviewing the anatomo-pathology of pT3 patients selected for an earlier trial [28] this fact was confirmed: patients that received preoperative radiotherapy and had tumors classified as pT3 at surgery there was 26.4% of lymph node cancer invasion, but in the group of patients operated on without preoperative radiotherapy the number of lymph nodes with cancer invasion arose to 47%.
This fact deserves a more objective analysis.
Was this fact responsible for better survival results observed in irradiated patients with pT3? It is very clearly demonstrated [1,7,12,19] that recurrence and survival is directly proportional to the number of lymph nodes invaded: as the incidence of lymphatic invasion decreased, there were better rates of recurrence and survival.
But why this difference?
Not frequently the pathologist demonstrates that some lymphatic with cancer invasion has altered this condition.
Anatomo-pathological studies registering effects of irradiation in lymphatic of the peri-rectal fat (mesorectum) are rare.
However, if this fact is added to the other mentioned effects of the irradiation (on tumor infiltration and carcinomatous cells) there is an explanation for the better observed curative results on C tumors survival rates of patients submitted to preoperative radiotherapy.
NOTES