1. Introduction
Campylobacter enteritis is a leading cause of acute bacterial gastrointestinal infection worldwide. The genus Campylobacter includes many species of which Campylobacter jejuni and Campylobacter coli are common pathogens and account for the majority of diagnosed human Campylobacter infections. Enteric infections caused by the two major species, C. jejuni (85% - 90%) and C. coli (9% - 14%) have increased considerably in recent years [1] .
Contamination is mainly transmitted with food, such as raw milk, salad, vegetables, insufficiently cooked meat (poultry, lamb and pork), in water (either drunk or in contact) and by the environment [2] . The disease is characterized by a generally moderate fever, abdominal pain and diarrhoea, sometimes with blood in the faeces [3] . Campylobacter are fastidious organisms and require a micro-aerobic environment for growth. The organism produces diffuse, bloody, oedematous and exudative enteritis. Campylobacter causes tissue injury in the jejunum, ileum and the colon [4] . In a small number of cases, the infection may be associated with haemolytic ureamic syndrome and thrombotic thrombocytopaenic purpura through a poorly understood mechanism [5] . Molecular methods based on PCR amplification are more accurate than bacterial culture [6] [7] . Therefore, this study identified Campylobacter using cultural and molecular methods.
2. Materials and Methods
2.1. Sampling and Sample Collection Sites
This study was carried out prospectively at the General Hospitals and Private Hospitals in Osun state between January 2018 and October 2018. Osogbo is in the Southwestern part of Nigeria. Subjects were patients between the age of 1 and 36 months, who presented with watery, offensive diarrhea with or without mucus, with or without blood and fever at-the paediatric units of these hospitals. It is a non-invasive study. However, informed consent was obtained from each of the mothers of all the children. The study was approved by the Ethical and Research Committee of the Ladoke Akintola University of Technology, Ogbomoso Oyo state, Nigeria. A total of 915 subjects were examined during the period of study, 815 (89%) with diarrhea and 100 (11%) without diarrhea which served as control group.
2.2. Growth and Incubation Methods
Collected rectal swabs were used to inoculate Butzler-type―medium (a selective medium which consisted of Butzler agar, 5% sheep blood and CAT from Oxoid comprised of cefoperazone, amphotericin B and teichoplanin as selective agents). The plates were incubated in an anaerobic incubator. The incubation was done in an atmosphere with reduced oxygen (5%) but with added carbon-dioxide (10%). They were incubated at 42˚C which prohibits growth of most of the other bacteria present in faeces, thus simplifying the identification of Campylobacter. Incubation was continued for 72 hours. Growing colonies were obtained and subcultured to obtain pure ones. Biochemical tests performed include catalase, oxidase and hydrogen sulphide production. The isolates were resistant to cephalothin, and did not grow aerobically. Biotyping was done by rapid hippurate hydrolysis Test, rapid H2S test and Deoxyribonucleic acid (DNA) hydrolysis.
Rapid Hippurate Hydrolysis Test using 1% Sodium hippurate in H2O and 3.5% Ni̥nhydrin in butanol-acetone (1:1). A loopful (2 mm) of a 24 - 48 hours old culture emulsified in 0.4ml of sodium hippurate solution in a test-tube. The test-tube was incubated for 2 hours in a 37˚C water bath. After, it was slowly overlaid with 0.2 ml of Ninhydrin reagent. Incubation was continued for 10 minutes. Crystal violet-like colour was read as positive reaction.
Rapid H2S Test: A large (about 0.5 cm in diameter) ball-like inoculum of the culture was inoculated into mixture of 0.05% each of ferrous sulphate, sodium metabisulphite and sodium pyruvate (FBP) broth (Oxoid). The test-tubes were incubated in a 37˚C water bath for 2 hours. Blackening around the bacterial mass indicates positive reaction.
Deoxyribonucleic acid (DNA) hydrolysis was carried using DNA Test agar and 0.5% methyl green solution. The DNA containing medium (DNase test agar) was prepared according to be manufacturer’s instruction (Qiagen Ltd). Methyl green was added to 100 ml of DNase agar, autoclaved and dispensed into 25 ml plate. All the strains of Campylobacters were tested for DNA hydrolysis. A loopful of 48 hours growth culture from the blood agar plate was used to inoculate a circular area approximately 1.0 cm in diameter on the surface of DNase test agar plate and incubated at 37˚C in an anearobic jar. All plates were examined daily for 5 consecutive days during incubation. An area of growth surrounded by a clear or colourless zone in the green agar was a positive test of DNA hydrolysis.
2.3. Extraction of DNA from the Sample
A total of 100 ml of each Campylobacter isolates was added to isotonic buffer and 750 µl lysis solution. Later centrifuged at 10,000 xg for 1 minutes. Binding buffer was added, later pre wash buffer and DNA wash buffer. A volume of 100 µl DNA Elution Buffer was added, centrifuged at 10,000 xg for 30 seconds and DNA was eluted.
2.4. PCR Amplification for flaA Gene
One of the best characterized Campylobacter virulence markers is the flaA gene which determines the major component of the flagella, hence bacteria motility and enterocyte colonization [8] . They also participate in adhesion and colonization [9] . All isolates were further identified by a molecular method based on 16 S rRNA species specific gene amplification by PCR and subsequent sequence analysis of the PCR products. PCR amplification was done using primers: flaAF GGATTTCGTATTAACACAAATGGTGC flaA 48˚C flaAR CTGTAGTAATCTTAAACATTTTG [10] . The PCR was performed in a 25 µl volume, the PCR mixture contained 2.5 m MgCl2, primers 0.5 µl, Taq polymerase 1.25 U, PCR buffer 0.5 µl and sterile water 15.9 µl. Amplification was carried out in an eppendorf master cycler. The cycling parameter consisted of an initial denaturation of 94˚C for two minutes, followed by 35 consecutive cycles of 94˚C for one minute, annealing at 50˚C for one minute and final extension at 72˚C for one minute.
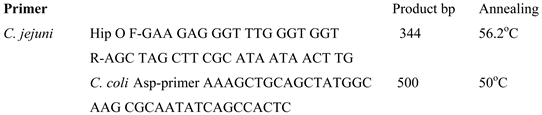
2.5. PCR Amplification Species-Specific for C. jejuni, and for C. coli
PCR was performed in 25 µl volumes, the PCR mixture contained 1 µl of template DNA, 10 mM Tris-HCl, 50 mM KCl, 2.5 mM MgCl2, 200 µM dATP, dCTP, dGTP, dTTP, 1.25 U Taq purple DNA polymerase (Fermentas), 1 µM of each oligonucleotide. The PCR was performed on a PTC-200 thermocycler, with the following programme: initial denaturation 5 min 95˚C, 2 × (1 min 94˚C, 1 min 72˚C), 2 × (1 min 60˚C, 1 min 72˚C), 2 × (1 min 94˚C, 1 min 58˚C, 1 min 72˚C),
The PCR products were visualized by electrophoresis in 1.5% agarose gel, stained with ethidium bromide (1 µg/ml) and viewed under UV light.
The SLST method was developed by Scholz and Jensen [11] to characterize the Campylobacter strains and to identify clonal lineages in this species. This method uses genetic variation at multiple chromosomal locations and allows generation of sequence data, which are deposited in internet databases for comparison with DNA sequences of other isolates. This was done using an ABI (applied Biosystem) 33,100 Genetic analyser (Life Technologies) a multicolour fluorescence based DNA analysis system with 16 capillaries operating in parallel.
2.6. Single-Locus Sequencing Typing Method
DNA amplification of gene was done using the primer described by Jonas Waldensrom.
glnA Glutamine synthetase gene was amplified
F-TAGGAACTTGGCATCATATTACC
R-TTGGACGAGCTTCTTCTACTGGC
3. Results
Cultural method gave a total of 57 Campylobacter isolates while only 25 of those 57 isolates were amplified by PCR as shown in Table 1. The result of PCR assays were not in complete agreement with phenotypic methods for identification of the bacterial isolates. From the 815 subjects with diarrhea, 347 (42.6%) were females, 468 (57.4%) were males, 25 were positive for Campylobacter species giving a prevalence of 3.06%. Eighteen C. jejuni were amplified by PCR and 7 were C. coli. as shown in Figure 1 & Figure 2. Fifteen were males while ten were females. C.jejuni biotype I were 8 while biotype II were 10 and all the C. coli belong to biotype I as shown in Table 2. All C. jejuni belong to subspp jejuni.
![]()
Table 1. Distribution of Isolates among Children with Diarrhea.
![]()
Table 2. Distribution of Biotypes of Campylobacter Species.
![]()
Figure 1. Agarose gel electrophoretogram of Campylobacter jejuni after PCR result.
![]()
Figure 2. Agarose gel electrophoretogram of Campylobacter coli after PCR results.
Result of Sequencing
glnA Glutamine synthetase PCR confirm it to be Campylobacter jejuni. All Campylobacter belong to ST-21 and ST-50. Thirteen Campylobacter jejuni belong to ST-21 and 5 Campylobacter jejuni belong to ST-50.
4. Discussion
Molecular methods were also used for the detection of Campylobacters. One of the best characterized Campylobacter pathogenic markers is the flaA gene which determines flagella formation, hence bacterial motility and enterocyte colonization [12] [13] . Results showed that all C. jejuni and C. coli confirmed by PCR possessed flaA gene. The adoption of molecular techniques in microbial diagnostic has become a promising alternative approach, as they possess inherent advantages such as shorter time to results, excellent detection limits, specificity and potential for automation. In the study, 57 isolates were gotten when cultural method was adopted; these isolates were later identified by molecular method only 25 were confirmed to be Campylobacter. Since molecular method is more confirmatory when compared with cultural method, the implication is that there could be false positive results when cultural method was used. Organisms such as Campylobacter, Helicobacter and Arcobacter belong to same class i.e. Epsilon Proteobacteria and have certain characteristics which are similar. These similar characteristics may give false-positive results. However, they can be distinguished using DNA base composition using PCR technique. Campylobacter spp. have different guanine plus cytosine (G + C) content from other members such as Wolinella and Helicobacter [14] .
Persson and Olsen (2005) observed 103 fold higher sensitivity of culturing compared to direct DNA purification is expected to be less pronounced on routine diagnostic samples, and the direct DNA purification should be considered advantageous with respect to the analysis of samples containing dead and non-cultivable bacteria that may constitute a significant proportion of the bacteria in a given stool sample [15] . No attempt was made during this study to identify Campylobacters directly in faecal samples or to determine the minimum numbers of bacteria required to produce a positive result.
However, there is evidence that PCR-based assays can be successfully applied to the direct detection of Campylobacter spp. and other pathogenic bacteria in clinical stool samples [16] .
The result obtained from study showed that C. jejuni had the highest prevalence of 72% (18 of 25) and C. coli with 28%. This fact conforms with the study by de Wit et al. that C. jejuni and C. coli are the two main species isolated in developing countries. The isolation rate of C. jejuni exceeds that of C. coli, similar to observations in most developed countries [17] . The most frequently isolated Campylobacter species was C. jejuni which is in conformity with other reports in Lagos and Ile-Ife. The result obtained from study showed that C. jejuni had the highest prevalence.