State level correlations between high heart attack and stroke symptomology knowledge scores and CVD risk factors and mortality rates ()
1. INTRODUCTION
An intramuscular injection (IMI) is a method of administering medications deep into the central area of specific muscle tissues. This route of administration provides rapid system absorption of medications thus enhancing the effects of the medications.
IMI drugs are generally given through the deltoid muscle and/or the gluteal muscles [1-3]. The administration of long acting injectable medications in the deltoid muscle is viewed as an alternative to the injection using the gluteal muscles by a considerable number of patients. Nevertheless, some patients experience increased injection site pain through this application while others perceive the change as beneficial in terms of practicability [4].
The most common reasons for preferring the deltoid muscle for IMIs instead of other muscles include easier access, enhanced privacy causing less embarrassment due to exposure of human body parts, and faster administration with the expectation of less pain, than injection through the gluteus route. Moreover, larger volume of fluid may be the predisposing reason for inducing greater pain when medications are administered through the deltoid muscle. The gluteal muscles are thick enough to permit the injection of larger volumes of fluid, whereas the volume limit for IMI to the deltoid muscles is only about 1 mL [5,6]. Therefore, it was considered that a long acting injection is better administered intramuscularly using the gluteal muscles, and we have to consider the volume, property of drug and its safety and absorption such as damage to tissues including subcutaneous and blood vessel or peripheral nerve.
In a previous study, Brahm NC, et al. [7] declared in their report, that determining the optimum needle length for administration of intramuscular formulations based on individual patient variables is critical, although this has not been extensively reported in patients receiving specific medications, e.g. Haloperidol and Hluphenazine decanoate IM administration. Therefore, needle length may play an important role in assuring accurate medication administration through IMI. Nevertheless, Brahm NC et al. stated that when anticipated results of intramuscular antipsychotic medication administration are not realized, practitioners are urged to consider specific patient variables, notably the thickness of adipose tissue which influences the depth of the needle insertion that will result in the accurate muscle delivery of the medication.
In a separate study, Choi DW, et al. [8] assessed optimal needle length for IMI into the gluteal muscles using the simple skinfold thickness method. In this study, 190 healthy adults were recruited and grouped into eight groups according to gender and body mass index (BMI, kg/m2). For each participant, the skinfold thickness of the dorsoguteal and ventrogluteal sites was measured using a caliper. However, subcutaneous tissue thickness was acquired through ultrasonic images. The study showed that for men in the overweight and obese groups who received IMI at the dorsoguteal site and for the obese group at the ventrogluteal site, and for women who were within normal weight, or overweight and obese, these groups were injected the medication at both IMI sites. The results illustrated that the mean subcutaneous tissue thickness of men exceeded 1.84 cm, while for the minimal needle length for IMI at the dorsoguteal site, the optimal intramuscular needle length was 1.4 times in women and 1.0 times in men compared to the skinfold thickness technique. At the ventrogluteal site, optimal intramuscular needle length was 1.3 times in women and 0.9 times in men as compared to the skinfold thickness technique. They concluded that skinfold thickness is a reliable index to determine optimal needle length with minimal effort prior to IMI.
Moreover, Zaybak A, et al. [9] reported on their study which measured subcutaneous tissue thickness at the dorsogluteal and ventrogluteal sites to determine optimal needle length for dorsogluteal and ventrogluteal IMIs in adults with BMI of more than 24.9 kg/m2. They found that problems can arise if drugs designed to be absorbed from muscle are only delivered into subcutaneous tissue. Increasing obesity in all developed and many developing countries makes this an increasing concern. Ultrasound measurements were made of the subcutaneous tissue considering overweight, obese and extremely obese people at the dorsogluteal and ventrogluteal sites with the probe held at a 90 degrees angle to the plane of the injection site. Subcutaneous tissue thickness was measured in 119 adults whose BMI was >or = to 25 kg/m2. Mean subcutaneous tissue thickness at the dorsogluteal site was 34.5 mm for overweight adults, 40.2 mm for obese adults and 51.4 mm for extremely obese adults, and at the ventrogluteal site was 38.2 mm for overweight adults, 43.1 mm for obese adults and 53.8 mm for extremely obese adults. In 98% of women and 37% of men, when IMI was administered at the dorsogluteal site and at the ventrogluteal site in 97% of women and 57% of men, it would not reach the desired muscles. A needle longer than 1.5 inches should be used in women whose body mass index is more than 24.9 kg/m2, and the dorsogluteal site may be used in all overweight and obese men, and the ventrogluteal site may be used in overweight men only.
Chan VO et al. [10] radiologically determined whether or not IMI was truly intramuscular, and they found that the majority of assumed IMIs were actually subcutaneous injections.
Kikuchi K et al. [11,12] reported that the most frequently used assessment method for the IMI to the gluteus medius is the “four-and three-way split method” which accounted for 85.5% of all IMIs in Japan. Approximately 90% of nurses use the 23 gauge needle (32 mm) for IMI. Furthermore, it was found that the length of the needle inserted as IMI by clinical nurses, was based on their experience to assess whether the needle has reached the muscle or not, rather than on credible evidence. The thickness of subcutaneous tissues for gluteal IMI sites was measured by an adipometer and by ultrasonography. In their study, the distance from the epidermis to the under-fascia (DEUF) of the gluteus maximus, and DEUF of the gluteus medius were measured, respectively. However, the distance from epidermis to the iliac bone (DEI) was not measured. Therefore, little is known about the relation between BMI, DEI, and DEUF when administering IMI.
The aim of this study was to determine the relationship between BMI, subcutaneous fat, and DEI among selected women in Japan.
2. METHODS
2.1. Study Design
The design used was a descriptive study to determine the relationship between BMI, subcutaneous Fat, and DEI among selected women in Japan. Ultrasonogaphy was used to collect the data.
2.2. Subjects
There were 39 adult healthy female subjects who volunteered and met the criteria. These criteria were that height was 160.00 ± 5.48 cm and weight was 51.30 ± 6.87 kg. Their ages ranged from 40s to 60s (50.82 ± 6.04). Of these subjects, 38 had right-foot dominance, while 1 had left-foot dominance.
2.3. Data Collection
This study was conducted between August 2011 to September 2011. To identify the injection site by the “four and three-way split”, the buttocks area was imaginarily divided into four quadrants. The proper injection site was located at the upper outer quadrant [13], and at one third the distance from the iliac crest on the imaginary 45 degree line (see Figure 1).
DEUF of the gluteus muscles and DEI were measured by ultrasonography. All ultrasonographic measurements were performed by an experienced Sonographer using a 7.5 MHz linear and convex array transducer and ultrasonograph diagnostic system (Hitachi Medical Corporation, Japan). Ultrasonograph images were made at the dorsogluteal injection site. Gluteus maximus, medius and minimus muscles are commonly used as regions for IMI. DEUF and DEI measurements were made above and outside a line drawn from the posterior superior iliac spine to the greater trochanter of the femur. Ultrasonograph probe was held at right angle to the skin at the gluteal region. These measurements were performed by an experienced female sonographer and reviewed by two sonographers (registered sonographer of the Japan Society of Ultrasound in Medicine) and one physician (registered neurosonographer of the Academy of Neurosonology) for consistency in reading the results of the sonography.
2.4. Hypothesis
Three research hypotheses were tested: 1) there is a significant difference in measurements of the DEUF of gluteus medius muscle, and the DEUF of gluteus maximus muscle, with the DEI and the BMI; 2) there is a significant difference between the right and left areas (buttocks area) from the data using each of the parameters; 3) there is significant correlation between the BMI, DEUF, and DEI.

Figure 1. IMI site in the buttocks “upper, outer quadrant” and “four-and three-way split”.
2.5. Data Analysis
The subjects’ height and the weight measurements were collected from the clinical records. The median BMI was 20.7 kg/m2. Collected data were divided into two groups based on median measurements: Group A (BMI < 21 kg/m2) and Group B (BMI ≧ 21 kg/m2). The Mann-Whitney’s U-test was used to determine the significant differences between the two groups. The Wilcoxon signed rank test was used to determine the significant differences in the data between the right and left DEUF of gluteal muscles. The Spearman’s rho correlation coefficient was used to determine the correlation between BMI and DEI, DEUF used in this study. A significance level was set at p < 0.05 (two-sided test). Statistical analysis of data was performed using SPSS (Ver. 18.0 J).
2.6. Ethical Considerations
Approval for the Ethics Committee of the Tokushima University Hospital was obtained. Both verbal and written informed consents were obtained from the 39 subjects of the study prior to commencement of the study.
3. RESULTS
The subjects were divided into two groups: Group A (n = 23) and Group B (n = 16). There was a significant difference between Group A (67.46 ± 6.36 mm) and Group B (73.34 ± 8.32 mm) using the DEI of the right gluteal muscle (p < 0.01). There was also a significant difference between Group A and Group B in DEUF using the gluteus medius muscle measurements of both areas of the buttocks (right side: p < 0.05, left side: p < 0.01). DEUF measurements of the gluteus medius muscle for Group A was 37.95 ± 6.22 mm (right side), and 36.71 ± 6.74 mm (left side), while for Group B it was 43.25 ± 8.86 mm (right side), and 43.41 ± 9.61 mm (left side). Moreover, there was a significant difference between Group A and Group B in DEUF measurements of the gluteus maximus muscle the left side (15.45 ± 3.36 vs 19.74 ± 5.20, p < 0.01). Furthermore, DEI of the right side was significantly greater than the left side (70.29 ± 7.90 vs 66.39 ± 9.32, p < 0.01) (see Tables 1 and 2).
There was a significant trend between BMI and DEI data from both sides of the buttocks (right side: ρ = 0.55, p < 0.01, left side: ρ = 0.43, p < 0.01); between BMI and DEUF of the gluteus medius muscle (left side: ρ = 0.50, p < 0.01), and between BMI and DEUF of gluteus maximus muscle (right side: ρ = 0.40, p < 0.05, left side: ρ = 0.56, p < 0.01). Also, there was a significant correlation between DEI and DEUF of the gluteus medius muscle (right side: ρ = 0.45, p < 0.01, left side: ρ = 0.69, p < 0.01), and between DEI and DEUF of gluteus maximus muscle (right side: ρ = 0.54, p < 0.01, left side: ρ = 0.51,

Table 1. BMI-based differences in DEI, DEUF of gluteus medius, and gluteus maximus by the four and three-way split.
Mann-Whitney U-test: *p < 0.05, **p < 0.01, n.s.: not significant. BMI: body mass index, DEI: distance from the epidermis to the iliac bone, DEUF: distance from the epidermis to the under-fascia.
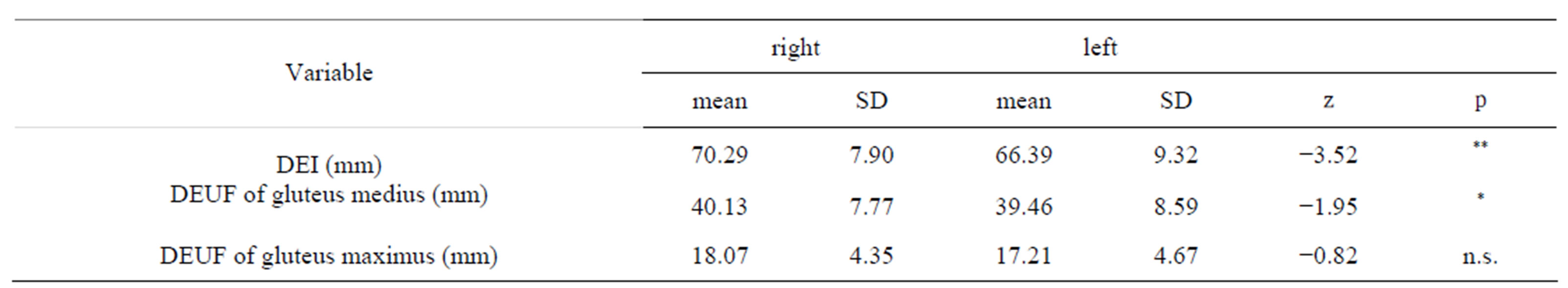
Table 2. Difference between right and left in DEI and DEUF (n = 39).
Wilcoxon signed rank test: *p < 0.05, **p < 0.01, n.s.: not significant. DEI: distance from the epidermis to the iliac bone, DEUF: distance from the epidermis to the under-fascia.
p < 0.01). Furthermore, there was significant correlations between DEUF of gluteus medius and maximus muscles in both sides (right side: ρ = 0.58, p < 0.01, left side: ρ = 0.62, p < 0.01) (see Tables 3 and 4).
4. DISCUSSION
Kikuchi K. et al. [12] declared that in the study they conducted, it was found that there was a strong correlation between BMI and the thickness of subcutaneous tissues. However, the DEI was not measured using ultrasonography. In the first hypothesis, the right side DEI, both sides of DEUF of the gluteus medius, and left side of DEUF of the gluteus maximus were significantly greater in Group B (BMI ≧ 21 kg/m2) measurements than in Group A (BMI < 21 kg/m2).
Femoral-gluteal subcutaneous adipose tissue and femoral-gluteal intramuscular adipose tissue distribution varies by gender and race [14]. In this current study, the DEUF of the gluteus maximus was dissimilar in the subject’s right and left sides.
The second hypothesis declared that the DEI of the right side was significantly greater than the left side. In this study, there was a bilateral difference in DEI, especially noting greater dispersion in the non-dominant foot. This was considered to be related to the dominant foot finding and the size of muscle mass in the specified area. Sanchis-Moysi J et al. [15] pointed out that asymmetry of gluteal muscles was inferred as possible reasons for differences in the gluteal muscle mass. They found that the muscles of the dominant foot were more developed among those with greater masses of gluteal muscles. Therefore, it is important to identify the dominant foot and assess for subcutaneous fat before administering an IMI.
In the third hypothesis, correlation was confirmed to be positive in the DEI and BMI. Also, a remarkable trend was observed in DEI and DEUF measurements of the gluteus maximus and medius in both sides of the buttocks. There was no significant correlation between BMI and DEUF of the gluteus medius based on data collected at the right side of the buttocks. The right side DEI of the Group B was significantly greater than those of Group A. However, on the left buttocks side, there was no significant difference between both groups.
From both sides of the buttocks, the DEUF of gluteus medius of the Group B subjects were significantly greater than those of Group A subjects. Also, there was a positive correlation in the DEI and BMI data. Therefore, it was understood that in fact the DEI may be approximately proportional to BMI. Therefore, the DEI of the right side was significantly greater than the left side. This finding supports that the higher BMI was correlated with a greater DEI, and that it is important to identify the dominant foot and to assess subcutaneous fat presence when considering the administration of IMI.
Generally in Japan, it is common to use the 23 gauge needle (32 mm) for IM injection [1]. However, DEUF of
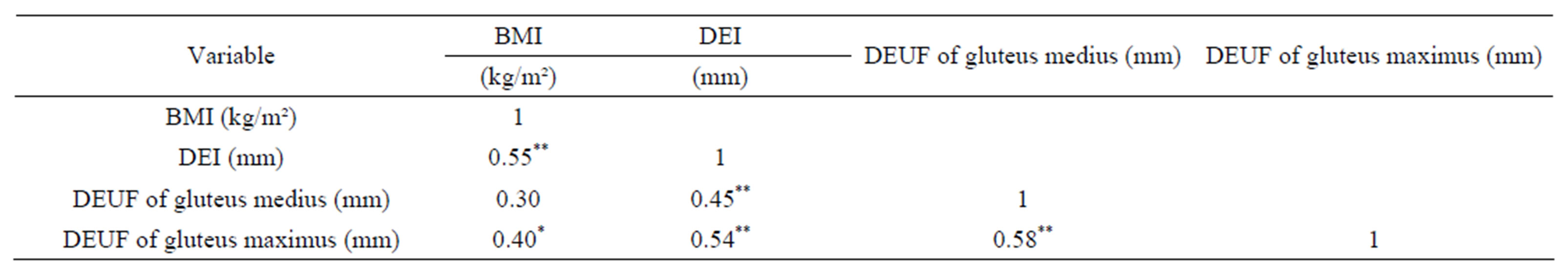
Table 3. Correlation between BMI, DEI, and DEUF in right side (n = 39).
Spearman’s rho correlation coefficients: *p < 0.05, **p < 0.01. BMI: body mass index, DEUF: distance from the epidermis to the under-fascia, DEI: distance from the epidermis to the iliac bone.

Table 4. Correlation between BMI, DEI, and DEUF in left side (n = 39).
Spearman’s rho correlation coefficients: *p < 0.05, **p < 0.01. BMI: body mass index, DEUF: distance from the epidermis to the under-fascia, DEI: distance from the epidermis to the iliac bone.
gluteus medius of the Group A(BMI < 21 kg/m2)was about 30 - 40 mm (on the right buttocks), and 35 - 50 mm (on the left buttocks). In the Group B (BMI ≧ 21 kg/m2), BMI was 30 - 40 mm (right buttocks), and 43 - 52 mm (on the left side). Therefore, it was thought that there is a great need to consider using gauge 20 or 21 (38 mm) needles when administering IMI.
5. LIMITATIONS
Only adult women in Japan comprised the subjects of the study; some measurements could not be obtained on every subject, at every injection site, therefore some data could not be matched or paired accordingly. On B-mode findings, the subcutaneous adipose tissues showed high echogenicity while the gluteal muscles showed relatively low echogenicity, or could not be identified correctly. In some cases, the fascia of gluteal muscles could not be detected on B-mode scan. Also, it was difficult to precisely detect the separation between gluteus maximus and gluteus medius.
6. IMPLICATIONS FOR FUTURE RESEARCH
The findings of the study provided data to support possible revisions in the procedures for administering medications via IMI. Future research can be conducted to determine the effect of administering IMI using various lengths of needles on the pain reaction of patients. Also considered is to determine other procedures for IMI which may decrease pain reactions during IMI, for example, the use of music preferred by the patient during the IMI considering various lengths of needles for the procedure. Furthermore, qualitative research focused on the description of the experience of the patients during IMI will provide increased awareness of the value of various interventions which may decrease perception of pain and reactions to painful stimulation.
7. CONCLUSION
The right side DEI, both sides of DEUF of the gluteus medius, and left side of DEUF of the gluteus maximus were significantly greater in Group B (BMI ≥ 21 kg/m2) measurements than in Group A (BMI < 21 kg/m2).
The DEI of the right side was significantly greater than the left side. In this study, there was a bilateral difference in DEI, especially noting greater dispersion in the non-dominant foot. It is important to identify the dominant foot and assess subcutaneous fat before administering an IMI.
Correlation was confirmed to be positive in the DEI and BMI. Also, a remarkable trend was observed in DEI and DEUF measurements of the gluteus maximus and medius in both sides of the buttocks. There was no significant correlation between BMI and DEUF of the gluteus medius based on data collected at the right side of the buttocks. From both sides of the buttocks, the DEUF of gluteus medius of the Group B subjects was significantly greater than those of Group A subjects. Also, there was a positive correlation in the DEI and BMI data. It was understood that in fact the DEI may be approximately proportional to BMI.
There was a positive correlation in BMI and DEI data from both sides of the buttocks. This finding supports that the higher BMI was correlated with a greater DEI, and was important to identify the dominant foot and assess subcutaneous fat at the IMI.
8. ACKNOWLEDGEMENTS
This study was supported by a grant-in-Aid for challenging exploratory research in Japan (No. 2366010000).