Serum Calcium Ionised Rate and Materno-Perinatal Prognosis in Arterial Hypertension in Pregnancy at the Reference General Hospital of Panzi ()
1. Introduction
The occurrence of maternal complications during hypertensive disease in pregnancy depends on a number of factors, including the mother’s age and race, and the presence of pre-existing pathologies such as diabetes or vasculitis [1] . In Africa and Asia, nearly a tenth of maternal deaths are associated with hypertensive disorders during pregnancy, while in Latin America, a quarter of these deaths are linked to complications of these hypertensive diseases of pregnancy [2] . Several factors play an important role in regulating maternal blood pressure during pregnancy, including calcium and vitamin D. Although several studies have not demonstrated the protective role of calcium supplementation in the prevention of hypertensive disease during pregnancy, some studies have shown a relationship between the onset of hypertensive disease during pregnancy and a reduction in blood calcium levels in certain pregnant women.
In a randomised study of 400 patients between 20 and 24 weeks’ gestation, Marya et al. [3] gave 1200 IU/d of vitamin D and 375 mg/d of calcium versus no treatment and showed a significant reduction in blood pressure in the treated group but no significant reduction in the occurrence of hypertension during pregnancy (6 versus 9%). This study demonstrates the protective role of calcium in significantly reducing blood pressure during hypertension in pregnancy. Lafond, Simoneau et al. [4] described changes in calcium metabolism in women with hypertensive disease during pregnancy.
Sophie Haché et al. [5] in her experimental study of calcium transport in pre-eclamptic patients, found a significant decrease in calcium transport by primary syncytiotrophoblasts and a decrease in protein and mRNA expression of several genes involved in calcium transfer in the placentas of women with hypertensive disease during pregnancy. It has also been shown that a calcium-supplemented diet can alleviate the symptoms caused by hypertensive disease during pregnancy, although this does not result in complete recovery of the mother or foetus [6] .
In Nigeria, Ikaraoha Chidiebere Ikechukwu et al. [7] , in a case-control study of 209 patients, 59 of whom were pre-eclamptic and 109 pregnant with a progressive monofoetal pregnancy, observed that pre-eclamptic patients had a decrease in serum calcium concentration during pregnancy. According to WHO recommendations, supplementation is recommended for populations at risk of chronic calcium deficiency [8] , as dietary supplements are not affordable for most people living in our environment. Calcaemia is a factor that can influence blood pressure during pregnancy, and its plasma variation would influence the severity of hypertension during pregnancy.
In view of the above, we asked ourselves the following question:
Maternal hypocalcaemia would be a factor of poor maternal prognosis during hypertensive diseases during pregnancy. To answer this question, we set ourselves the following objectives:
- General objective
To determine serum ionized calcium levels in patients with hypertensive disease during pregnancy.
- Specific objectives
To determine the maternal prognosis of patients with hypertensive disease in pregnancy according to serum ionic calcium levels.
To determine the perinatal prognosis of newborn babies of mothers with hypertensive disease of pregnancy according to serum ionized calcium levels.
2. Materials and Method
2.1. Type of Study
We conducted a cross-sectional study period from 1 January 2021 to 30 June 2022.
The study was carried out at Panzi Hospital, which is a referral health facility in the Ibanda health zone, serving 17 health areas with an estimated population of 515,834. It is also a university training clinic where general practitioners, obstetricians and midwives are trained.
2.2. Type of Study
Our research is a cross-sectional study with analytical aims.
2.2.1 Study Population
Our sample will be exhaustive, consisting of pregnant women and women delivered with arterial hypertension during pregnancy and those delivered in the post-partum period who were diagnosed with arterial hypertension before the sixth week and patients transferred to us for arterial hypertension in the post-partum period.
2.2.2. Study Period
The study period is 18 months, from 1 January 2021 to 30 June 2022.
1) Inclusion criteria
It concerns all pregnant women, parturients and women who have given birth have been diagnosed with hypertensive disease during pregnancy and who have voluntarily agreed to take part in the study.
2) Exclusion criteria
All pregnant women, parturients and women in labour had not been diagnosed with hypertensive disease and patients did not voluntarily consent to the study.
2.2.3. Sample Storage and Analysis Techniques
Prevalent study was carried out in a dry tube of about 3 to 5 Cc, kept at 4˚ for a period of 2 weeks before analysis of blood calcium, the sample being stable between 20 and 8 provided it was kept in a hermetically sealed container and protected from light and contamination during use.
For analysis we used:
Analysis: Spectrophotometer or colorimeter for measurements at 620 mm Optical path 1.0 cm Serum or plasma separated from cells as quickly as possible Blood anticoagulants with loxalate, citrate or EDTA are not acceptable, since these chemicals form strong chelates with calcium.
Principle Calcium in the presence of Arsenazo III (1,8-dihydroxy-3,6-disulfo-2,7-naphthylene bis(azo) dibenzene arsonic acid) at neutral pH produces a blue coloured complex whose intensity is proportional to the concentration of calcium.
2.3. Sampling
2.3.1. Inclusion Criteria
We considered hypertensive disease to be any episode of arterial hypertension characterised by: Persistent arterial hypertension (AH) (diastolic blood pressure ≥ 90 mmHg) and significant urine dipstick proteinuria. Depending on the number of crosses, proteinuria was classified as mild if there was no proteinuria or only one cross, moderate if there were two crosses and severe if there were three or more crosses when the urine dipstick was read.
2.3.2. Data Collection, Processing and Analysis
Samples were taken on admission or within 48 hours of delivery or late abortion, and proteinuria was determined by qualitative analysis based on the number of crosses in the urine dipstick. The text was entered using Microsoft Office Word 2010 and the tables were analysed using Excel 2010. The data was analysed using SPSS version 20.0 and Stata 14.0. Qualitative variables have been summarised by Percentage and quantitative variables will be summarised by Means and Standard Deviation.
The associations of the variables were calculated using Pearson’s chi-square test, with a significance threshold set at a value of p < 0.05.
For the study of risk factors, Odds ratios and their confidence intervals were estimated in a univariate analysis. The most determining factors were identified by multivariate analysis using the Forward conditional logistic regression model. The statistical significance threshold was set at 0.05.
2.4. Variables Studied
We will analyze the different variables to arrive at the results. Two types of variables will be analyzed: We are going to analyze the different variables for our research to arrive at the results. Two types of variables were analyzed:
1) The dependent variable: Calcaemia.
2) Independent variables: Gestational age, blood pressure, paraclinical variables (haemoglobin, haematocrit, platelet count and haemocalcaemia), perinatal prognosis (foetal viability and APGAR score at 1, 5 and 10 minutes) and maternal prognosis (type of maternal haemocalcaemia, maternal complications).
2.5. Ethical considerations
Our research protocol was submitted to the university’s ethics and licensing committee to conduct this study. Free and informed consent was obtained from the study participants prior to data collection, and any subject had the right to accept or refuse to participate in the study. Confidentiality and anonymity were guaranteed in this study.
3. Results
In Table 1: for systole, the mean was 164.28 mmHg with a minimum of 100 mmHg and a maximum of 243 mmHg and for diastolic, the mean was 107.46 mmHg with a minimum of 70 mmHg and a maximum of 128 mmHg; for gestational age, the mean was 34.43 ± 4.327 amenorrhea weeks with a maximum at 41 amenorrhea weeks and a minimum at 20amenorrhea weeks (Figure 1). An average age was 34.43 ± 4.327 amenorrhea weeks (SA).
Table 1. Blood pressure and gestational age.
Haemoglobin averaged 117.29 ± 26.091 mg/dl, with a maximum of 186 mg/dl and a minimum of 44 mg/dl, haematocrit averaged 35.706% ± 7.1212% with a minimum of 13.2% and a maximum of 56.7%, platelets averaged 201.87 ± 85.591.109 elements/ml with a minimum of 46.109 elements/ml and a maximum of 453.109 elements/ml and blood calcium levels averaged 1.746 ± 0.6702 mg/dl with a minimum of 0.3 mg/dl and a maximum of 3.6 mg/dl (Table 2 and Figures 2-3).
Table 2. Distribution of patients according to haemogram and ionogram results.
![]()
Figure 3. Indications for caesarean sections.
The route of delivery for patients with arterial hypertension during pregnancy was the vaginal route (53.4%) and the caesarean section route (46.6%), of which 66.6% of the indications for vaginal deliveries were specifically related to arterial hypertension during pregnancy.
The table shows the serum calcium levels in our patients: 64.9% of patients had hypocalcaemia compared with 28.1% who had normal serum calcium levels (Table 3).
As regards the types of maternal complications, eclampsia was the most frequent complication in our patients (31.7%) (Table 4).
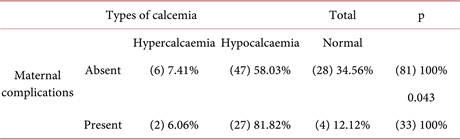
This table assesses the presence of maternal complications as a function of the type of maternal calcium levels. Of all those who presented a complication, 81.82% were hypocalcaemic, which had a significant influence on the presence of maternal complications at a significance level of 5% (Table 5).
Table 3. Frequency of serum ionised calcium types in hypertensive patients during pregnancy.
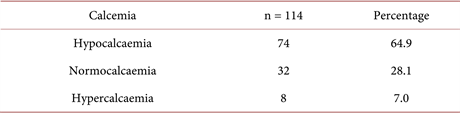
Table 4. Frequency of maternal complications.
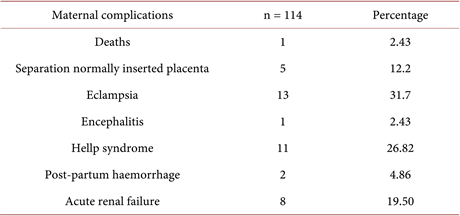
Table 5. Analysis of the relationship between the presence of maternal complications and calcaemia types.
In this table there are few complications that are significantly influenced by the types of calcaemia, with the exception of hellp syndrome (p = 0.010) at a significance level of 5%. On the other hand, the odd ratio results show a weak influence of the types of maternal complications on calcaemia at a significance level of 5% (Table 6).
In the table above, 33 cases presented a complication, a figure representing a 58% risk of exposure. This gives an odd ratio of 3.255, proving very significantly (p-value = 0.0158) three times the risk that the patient presenting a complication is likely to be hypocalcaemic at a 95% confidence level (Table 7).
This table assesses the foetal viability of patients with hypertension during pregnancy; 35% of foetus had died in utero at our admission examination (Table 8).
Table 6. Analysis of the relationship between each maternal complication in relation to hypocalcaemia and eucalcaemia.
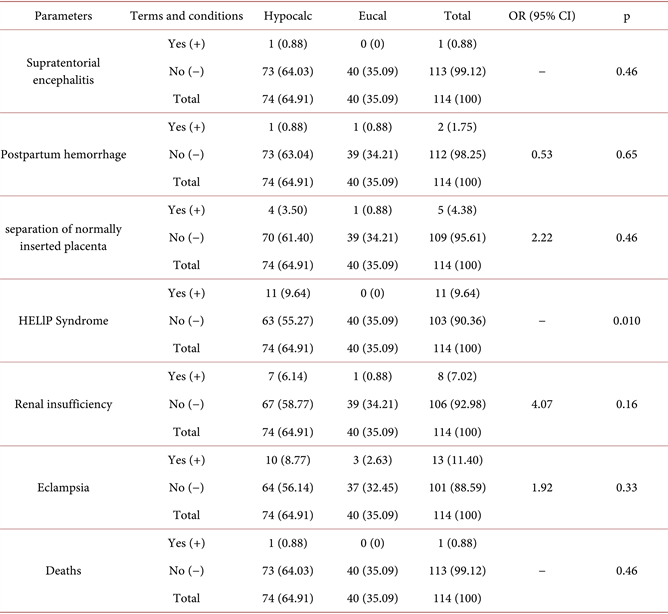
Table 7. Analysis of the relationship between maternal complications and maternal hypocalcaemia and eucalaemia.
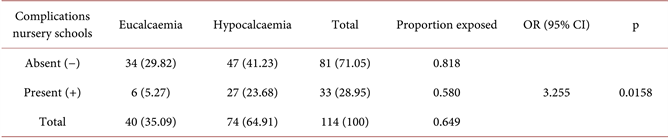
Table 8. Frequency of fetal viability on admission.
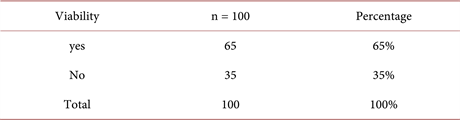
In the table, we noted that there were 19 patients with this complication who were hypocalcaemic and 55 patients without this complication but also hypocalcaemic. We found no significant influence of daed according to maternal hypocalcaemia (p = 0.11) at a significance level of 5% (Table 9).
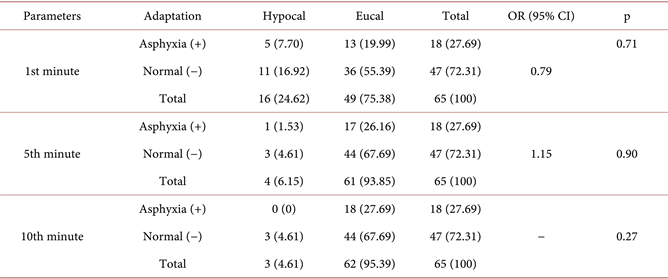
This table assesses the adaptation of newborn babies to life ex-utero: At the first minute, 3.1% of newborns had severe asphyxia, 21.5% had moderate asphyxia and 75.4% had good ex-utero adaptation, at five minutes, 6.2% of newborns had moderate asphyxia and 93.4% had adapted well in the ex-utero setting, at ten minutes, 4.6% of newborns had moderate asphyxia and 95.4% had adapted well in the ex-utero environment (Table 10).
From this APGAR score evaluation table, we can see that no parameter has a significant influence on the other at the 5% threshold (Table 11).
4. Discussion
We assessed the serum ionic calcium level in patients who had developed hypertensive disease during pregnancy. The mean ionic calcium level was 1.746 ± 0.6702 mg/dl, with a minimum of 0.3 mg/dl and a maximum of 3.6 mg/dl, the first group, made up of patients with abnormally low calcium levels, represented 64.9% of our sample, i.e. 74 patients, those with abnormal serum calcium levels represented 28.1% of cases, i.e. 32 patients, and those with abnormally high serum calcium levels represented 7% of cases, i.e. 8 patients.
In 2015, in a study comparing two groups of women, those with pregnancies complicated by pre-eclampsia and those with pregnancies without pre-eclampsia, Karabi Baruah et al. [9] found that those with pre-eclampsia had abnormally low serum calcium levels compared to those with pregnancies without pre-eclampsia (p < 0.0001).
Table 9. Analysis of the association between foetal viability and types of calcaemia.
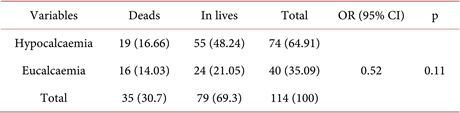
Table 10. Frequency of APGAR score in neonates.
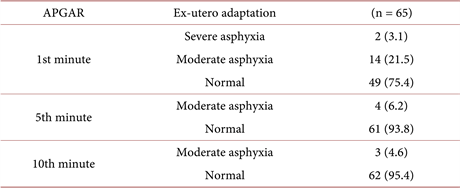
Table 11. Analysis of APGAR score as a function of maternal calcium levels.
In a 2012 study, Ikaraoha Chidiebere Ikechukwu et al. [7] analysed serum lead, calcium and phosphorus levels in women with pre-eclampsia in Edo State, Nigeria. They analysed three groups, 59 patients with pre-eclampsia, 150 women with normal pregnancies and 122 non-pregnant women, and found that patients with pre-eclampsia had low serum calcium levels (p = 0.001).
Lafond and Simoneau [4] described changes in calcium metabolism in women with pre-eclampsia. As the route of delivery is a factor in assessing maternal prognosis, delivery by the upper route is a factor in long-term maternal morbidity. We found that 46.6% of these patients delivered by caesarean section, which is a factor in both long-term and short-term maternal morbidity, with a frequency of 66.6% of caesarean section indications linked to maternal prognosis following the severity of either hypertension or a significant disturbance in maternal biological parameters that could jeopardise the mother’s vital prognosis.
With regard to the relationship between the presence of maternal complications and the different types of gestational arterial hypertension. Calcium supplementation may reduce the risk of pre-eclampsia and may help to prevent premature births ; a meta-analysis including 27 studies involving 18 064 women, G. Justsus [10] high dose calcium supplementation at ≥ 1gr/d versus placebo, the mean risk of arterial hypertension was reduced with calcium supplementation versus placebo (12 trials) 15,470 women (RR: 0.65, 95% CI: 0.53 - 0.81) There was also a reduced risk of preeclampsia associated with calcium supplementation (13 trials 15,730 women mean RR = 0.45, 95% CI: 0.31 - 0.65). A multicentre, randomised study of calcium supplementation during pregnancy by Justus Hofmeyr et al. [11] in a calcium group and a placebo group found that preeclampsia occurred in 23% of the calcium group and 29% of the placebo group with pregnancies beyond 20 days’ gestation (RR = 0.80, 95% CI: 0.61 - 1.06, p = 0.121) Calcium supplementation starting before pregnancy up to 20 weeks’ gestation, compared with placebo, did not show a significant reduction in pre-eclampsia.
In her study, Filomena Gomes et al. [12] concluded that calcium supplementation during pregnancy is known to reduce the risk of hypertensive disorders during pregnancy and associated complications including pre-eclampsia, maternal mortality and preterm delivery. A meta-analysis on supplementation and prevention of pre-eclampsia, Tito silvio [13] literature review of all studies of calcium versus placebo available in MEDLINE /PUBMED until 29/02/2012 concerning calcium supplementation during pregnancy to prevent pre-eclampsia taking into account the types of maternal complications, we found that post-partum haemorrhage (p = 0.050) and HELLP syndrome (p = 0.037) were significantly influenced by maternal hypocalcaemia at a threshold of 5%.
By analysing the relationship between the presence of maternal complications and the types of maternal calcaemia, the situation of hypocalcaemia and that of eucalcaemia (normocalcaemia and hypercalcaemia), we found a risk of 3.255 times that a patient with maternal complications linked to hypertension during pregnancy is hypocalcaemic, and very significantly (p = 0.0158) at 5% that maternal hypocalcaemia influences the presence of maternal complications.
In assessing perinatal mortality in relation to maternal serum calcium, maternal hypocalcaemia was not found to be significantly associated with fetal death in utero (p = 0.11) and the risk was small, 0.52 times the risk of hypocalcaemia affecting fetal death in utero in patients with hypertension during pregnancy.
Taking into account the adaptation to extra-uterine life of the newborns of mothers with hypertension during pregnancy, at the 1st minute, 3.1% of newborns had severe asphyxia with a score of 2 to 3 out of 10, 21.5% had moderate asphyxia with a score of 4 to 6 out of 10 and 75, 4% had a good APGAR ≥ 7, at the 5th minute, 4% of newborns had moderate asphyxia with a score between 4 and 6 out of 10 and 93.4% had a good APGAR ≥ 7, at the 10th minute, 4.6% of newborns had moderate asphyxia with a score between 4 and 6 out of 10 and 95.4% had a good APGAR ≥ 7.
In her study Joëlle M. et al. [14] found that at the end of the 1st minute, 37.9% of newborns born to hypertensive mothers had a depressed Apgar score compared with 12.6% of newborns born to non-hypertensive mothers. Neonatal depression is significantly related to the association between hypertension and pregnancy (p < 0.05 at the end of the first minute) and the risk of neonatal depression was multiplied by 4 in the newborns of hypertensive patients. Itoua C. [15] reported a low Apgar score in more than a third of newborns in 33% of hypertensive mothers.
Our study on the association of impairment of adaptation to extra-uterine life in newborns of patients with hypertension during pregnancy as a function of maternal serum calcium showed no influence of maternal serum calcium on the occurrence of neonatal asphyxia at the 5% significance level and the odds ratio showed all values less than 1. This shows that there is 0.79 times the risk of neonatal asphyxia occurring in the event of maternal hypocalcaemia at the first minute, 1.15 times the risk of neonatal asphyxia occurring in the event of maternal hypocalcaemia, which shows that this risk is less negligible.
5. Conclusion
Maternal hypocalcemia being one of the factors that can influence maternal-fetal complications during hypertensive diseases of pregnancy, several risk factors have been associated with maternal hypocalcemia, notably advanced maternal age with a mean of 30.33 ± 7.020 years, primiparity was associated with 33.3%, maternal complications were significantly associated with maternal hypocalcemia (p = 0.043), with an OR = 3.255, i.e. three times the risk that a patient with complications of HTA would be hypocalcemic, with average gestational age at Frantcats France, delivery was 34.43 ± 4.327 Aw with an OR = 0.52, and no significant association was found between perinatal asphyxia and maternal calcemia.