Religion and “Zero-Dose” Vaccination Status in Children Aged 12 to 23 Months in Benin and Togo: “Evidence of Demographic and Health Survey and Multiple Indicator Cluster Surveys” ()
1. Introduction
Vaccination is a simple, safe and effective means of protecting an individual against a disease by stimulating their immune system [1] . Today, available vaccines can prevent more than 20 life-threatening diseases, helping people of all ages live longer, healthier lives [2] . Each year, 3.5 - 5.0 million deaths are prevented through vaccination [2] . However, many children still do not receive the basic vaccines they need for their health and well-being. In 2019, 23 million children under the age of one had not received basic vaccines, the highest figure since 2009 [2] . In this group of insufficiently vaccinated children, nearly 75%, called “zero-dose” children, had not even received the first dose of the Diphtheria-Tetanus-Pertussis (DTP) vaccine, i.e. 17.1 million [3] . In the African region of the World Health Organization (WHO), it is estimated that the “zero-dose” vaccination status affects about one in five children [4] . Despite the efforts made and the progress made, Benin and Togo, two neighbouring countries in West Africa, are still facing problems related to insufficient vaccination coverage of children. In 2017, national surveys estimated that respectively 16% - 34% and 12% - 28% of children aged 12 to 23 months have a “zero-dose” vaccination status [5] [6] .
The Immunization 2030 Agenda (IA2030) is a global strategy initiated by the World Health Assembly and endorsed by several countries, including Benin and Togo, aimed at reducing morbidity and mortality from preventable diseases by vaccination [7] . The objective pursued is to reduce by 50% the frequency of “zero-dose” children at national, regional and global levels by 2030 [7] . Guided by the principle of leaving no one behind, it then appeared necessary to better understand the epidemiological profile of “zero-dose” children in order to better target the most vulnerable groups [7] . In this context, there is a growing number of studies in the literature on the predictors of “zero-dose” children, particularly in low- and middle-income countries. Zero-dose children are reported to be more concentrated in disadvantaged groups, isolated communities and conflict zones [8] . In addition, a study in 2022 found significant heterogeneity in the prevalence of zero-dose children between ethnic groups [9] .
In addition to the factors mentioned above, hypotheses have been formulated on the influence of the religious context in which children live on their “zero-dose” vaccination status. Religion designates a set of beliefs and dogmas defining the relationship between man and the sacred [10] . Many authors have underlined the strong significance of religion in contemporary African societies [11] [12] . Sub-Saharan Africa is reported to be home to approximately 24% of all Christians and 16% of all Muslims in the world [13] . The Beninese and Togolese populations are overwhelmingly “believers” with respectively less than 6% and 8% who declare no religious affiliation [5] [14] . Affiliation to religion may affect the adoption of health-promoting behaviours due to theological objections to certain health care or services [15] . The negative influence of religion on attitudes and practices regarding family planning is well documented [16] - [21] . With regard to the specific relationship between religious affiliation and vaccination coverage in children, a review of the literature does not reveal a meta-analysis, combining the conclusions of individual studies on the question. Considering the individual studies, discordant results are observed on the question of the relationship between religion and the occurrence of “zero-dose” or more broadly between religion and complete vaccination coverage in children [22] - [27] . A review of the literature does not identify individual studies in Benin and Togo on the influence of religion on the “zero-dose” vaccination status of children. This work aims to study the relationship between religious affiliation and the “zero-dose” vaccination status of children aged 12 - 23 months in Benin and Togo.
2. Methods
2.1. Study Setting
Benin and Togo are two West African states of 114,763 km2 and 56,785 km2, respectively, with a population of 12,535,929 (2021) and 8.6 million (2021) inhabitants [28] [29] . Administratively, Benin has 12 departments which are divided into 77 communes [30] . Togo is divided into five regions: maritime region, plateau region, central region, Kara region and savannah region [14] . The regions are themselves divided into 39 prefectures, subdivided into 117 communes [31] . Both countries have a demographic context characterized by high population growth (2.8% and 2.4% per year, respectively) [32] , a high total fertility rate (5.7 and 4.6, respectively) [5.6] and a high infant mortality rate (86 and 64 per 1000, respectively) [33] . The epidemiological profile of Benin and Togo is characterized by the predominance of communicable diseases which represent approximately 64% of DALYs [34] . In both countries, the vaccination schedule includes one dose of BCG vaccine and poliomyelitis vaccine (OPV) at birth, three doses of Pentavalent vaccine containing DTP, Hepatitis B and Haemophilus influenzae type b (Hib) antigens, three doses of poliomyelitis vaccine (oral), three doses of pneumococcal vaccine (conjugate), one dose of injectable poliomyelitis vaccine (IPV) at 6, 10 and 14 weeks of age of the child and one dose of vaccine against measles and rubella, one dose of vaccine against yellow fever and a second dose of injectable poliomyelitis vaccine at the age of 9 months and finally a dose of vaccine against meningitis belonging to type A serogroup and a second dose against measles and rubella at from 15 months [35] [36] [37] . In addition, in Benin, the vaccination schedule recommends three doses of the rotavirus vaccine at 6, 10 and 14 weeks compared to two in Togo at 6 and 10 weeks [35] [36] [37] .
2.2. Type of Study and Data Sources
This was a cross-sectional study that consisted of carrying out secondary analyses using the databases of the most recent editions of the Demographic and Health Surveys in Benin and the Multiple Indicator Cluster Surveys (MICS) in Togo. The DHS are series of national surveys carried out since 1984 within the framework of the DHS program, created by the American Agency for International Development (USAID) in 1984 [38] . The MICS surveys are a global program of national surveys developed by the United Nations Children’s Fund (UNICEF) in the 1990s [39] . Both aim to support countries in collecting internationally comparable data on indicators relating, among other things, to the situation of children under five and women of childbearing age [38] [39] . Benin has carried out five DHS, the last of which in 2017-2018 was selected for this study [5] . Five MICS have been conducted in Togo, the most recent of which was in 2017, which we considered for this study [6] . After registering on the respective websites of the DHS and MICS survey programs, a request made it possible to obtain the databases for DHS-V for Benin and MICS-6 for Togo.
2.3. Study Population
Included in the study, were living children aged 12 - 23 months successfully surveyed during the DHS-V (2017-2018) and MICS6 (2017) in Benin and Togo. For children born of multiple pregnancies, only the “first” twin was included. Deceased children, those not usually residing in the surveyed households were not retained for the study.
2.4. Sampling
Details on the sampling procedure of the different targets of the DHS-V (2017-2018) and MICS6 (2017), including children under five are available in the full reports [5] [6] . In summary, they are based on a probability method and a two-stage stratified sampling technique.
To do this, the national territory of Togo has been divided into seven areas of study, namely: Maritime, Plateaux, Central, Kara, Savanes, Lome Commune and Golfe Urban. Each of these study areas was stratified into urban and rural except the last two (Lome Commune and Golfe Urban) which constituted entirely urban strata. Thus, 12 strata were considered. The sample size was set at 8400 households, with 1200 households per field of study [6] . In each area of study, 20 households should be surveyed per Primary Survey Unit (UPS) for a total of 60 UPS, or 420 UPS at the national level [6] . At the first stage, a given number of PSUs was selected in each of the seven domains of study, independently in each stratum (urban and rural) from a sampling frame of 1600 enumeration areas (EAs), which was built in 2015 from the General Population and Housing Census of 2010 (GPHC4) [6] . A total of 420 UPS were drawn. The second degree concerned the selection of households, at the rate of 20 per UPS. The number of households to be selected initially planned to be 8,400 increased to 8,404 because in the Central region, four households initially sampled were split (each in two) because certain members formed their own household. Among the 8,404 households selected for the sample, 8,065 were found, of which 7,916 were successfully integrated (response rate = 98.2%) [6] . In the households surveyed, 4,942 children under five were successfully surveyed for a total of 5,030 who were eligible (response rate = 98.3%) [6] .
For Benin, the national territory has been divided into 12 fields of study corresponding to the 12 administrative departments and, in each field of study (except the Littoral department which has no rural areas). Two strata 2 strata were created (rural and urban) in each department except in the coastal department. The selection of the EDSB-V sample was done, stratum by stratum, through a stratified area survey and at 2 degrees. At the first level, 555 Primary Survey Units (UPS) or clusters were drawn from the list of enumeration areas (ZD) established during the fourth General Population and Housing Census carried out in Benin in 2013 (GPHC4), by carrying out a systematic draw with probability proportional to the size of the UPS (the size of the UPS is the number of households). Then, a count of households in each of these clusters made it possible to obtain a list of households from which was drawn, at the second stage, a sample of 26 households per cluster in both urban and rural areas, with a systematic draw with equal probability [5] .
2.5. Variables
2.5.1. Dependent Variable
The dependent variable was the “vaccination status” of the child. This is a binary qualitative variable that takes the value “1” when it is a “zero-dose” child and “0” otherwise. The 2030 Agenda for Immunization defines “zero-dose” children as those who have not received the first dose of Pentavalent vaccine containing the diphtheria-tetanus-pertussis (DTP), Hepatitis B and Haemophilus influenzaetype b (Hib) vaccine [40] [41] . In the present study, the data relating to the vaccination status are based on the vaccination card.
2.5.2. Main Exhibition
This was the religious affiliation of the household head or mother which was categorized as follows: Christianity, Islam, Traditional and other, no religion. Data on religion for Togo in MICS6 comes from the head of household, while that for Benin in the DHS-V comes from the mother.
2.5.3. Other Independent Variables
We distinguished:
· Variables related to the child: age of the child in months (12 - 17, 18 - 23), sex of the child (Male, Female), type of pregnancy (Twins, Single) and birth order of the child (1, 2 - 3, 4 - 6, 7 and up);
· The variables related to the mother: age of the mother (<20, 20 - 29, 30 - 39, and 40 - 49), level of education of the mother (Non-educated, Primary, Secondary and more), marital status of the mother (Alone, In couple), ethnicity of the mother (Adja, Bariba, Dendi, Fon, Yoa/Lokpa, Betamaribe, Peulh, Yoruba, other Beninese, other nationalities) for Benin;
· Household variables: age of the head of household in years (18 - 29, 30 - 39, 40 - 49, 50 - 59, 60 and over), sex of the head of household (male, female), level of education of the head of household (Educated, Primary, Secondary and more), size of the household (≤5, >5), ethnicity of the head of the household (Adja-Ewe, Kabye, Paragourma, Ana-Ife, Akposso/Akebou, other ethnic groups and other nationalities) for Togo, level of household wealth (Very poor, Poor, Intermediate, Rich and very rich);
· Variables related to the environment: environment (Urban, Rural), region for Togo (Maritime, Plateaux, Centrale, Kara, Savanes, Lome commune-Golfe Urban) and department for Benin (Alibori, Atacora, Atlantique, Borgou, Hills, Couffo, Donga, Littoral, Mono, Oueme, Plateau and Zou).
2.6. Data Analysis
The analyzes took the survey plan into account. The numbers and the weighted percentages of the modalities of the independent variables including the religious affiliation of the head of the household or of the mother were presented. The prevalence of children’s “zero-dose” vaccination status was calculated for Benin and Togo, along with the 95% confidence interval (95% CI). The influence of the religious affiliation of the head of household or mother on zero-dose vaccination status was determined after multiple logistic regression. In this context, the dependent variable was crossed with each of the independent variables including the religious affiliation of the head of household or the mother by a simple logistic regression. Variables significant for p < 0.20 were then entered into a multiple logistic regression. By a top-down step-by-step strategy, the least significant variables were gradually removed so as to have only variables with p < 0.05. The religious affiliation of the head of household or of the mother was kept at each stage regardless of its level of significance. The results were presented in the form of Odds Ratio (OR) accompanied by the 95% CI. All analyses were done using Stata 15 software. The fit of the final models was checked using the Hosmer-Lemeshow test.
2.7. Ethics
The launch of the EDS-V data collection was conditional on obtaining the authorization of the National Ethics Committee for Health Research and the ICF Ethics Committee [5] . The MICS6 protocol was approved by the National Bioethics Advisory Committee in July 2017 [6] . For both surveys, the ethical requirements in terms of research, in particular obtaining the free and informed consent of the participants and the anonymity of the information provided were respected. Additional details on ethical aspects are presented in the full reports of the investigations [5] [6] .
3. Results
3.1. Sample Description
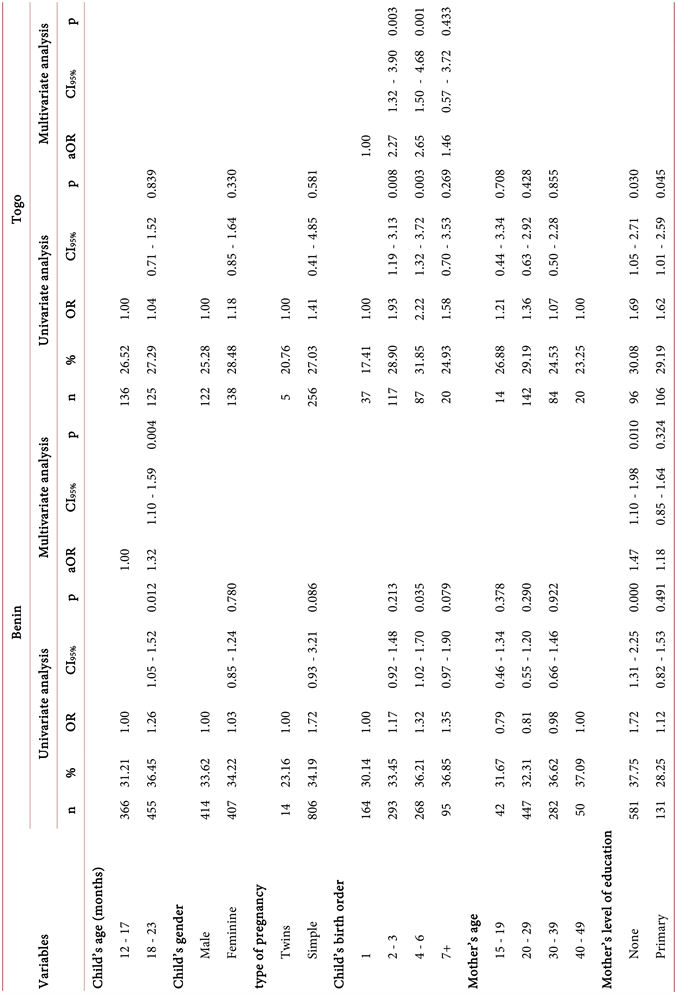
Table 1 presents the basic characteristics of the children surveyed. A total of 2,430
![]()
Table 1. Basic characteristics of children surveyed, Benin (2017-2018) and Togo (2017).
children were included in the study on behalf of Benin, with just over half (51.58%) aged 18 - 23 months. For Togo, 933 children were retained, of which a little less than half (47.15%) were aged 18 - 23 months. In Benin, male children were slightly more represented than their female counterparts (50.85% vs 49.15%). In Togo, there were almost as many girls as boys (485 and 484 respectively). There were 2.51% twins in Benin and 2.31% in Togo. Children of order two or three were the most frequent in both countries (36.42% in Benin and 41.66% in Togo). The majority of children had mothers aged 20 - 29 (57.12% in Benin and 50.17% in Togo) and in a couple (93.91% in Benin and 95.44% in Togo). Nearly 64% of Beninese children had mothers with no formal education. In Togo, this percentage was about half as high (33.13%). In Benin, just over a third of the children had Fon mothers (34.53%). In addition, about eight out of ten children lived in households headed by individuals under the age of 50 (79.60% in Benin and 82.50% in Togo) and males (83.53% in Benin and 83.90% in Togo). In Benin, 56.04% of children lived in households headed by individuals with no formal education compared to more than half as many (25.19%) in Togo. Also, in Togo, 43.16% of children lived in households headed by people with secondary education or more, compared to half as many in Benin (21.52%). In Togo, just over a third (36.27%) of children lived in households headed by Adja-Ewe/Mina. With regard to the place of residence, in the two countries, about six out of ten children (62.19% in Benin and 59.77% in Togo) lived in rural areas. In addition, according to the region of residence, children in the Lomé commune-Gulf urban region (25.65%) were the most represented in Togo, followed by those in the Plateaux region (22.25%). In Benin, it was Borgou (13.85%), Alibori (12.66%) and Atlantique (12.04%).
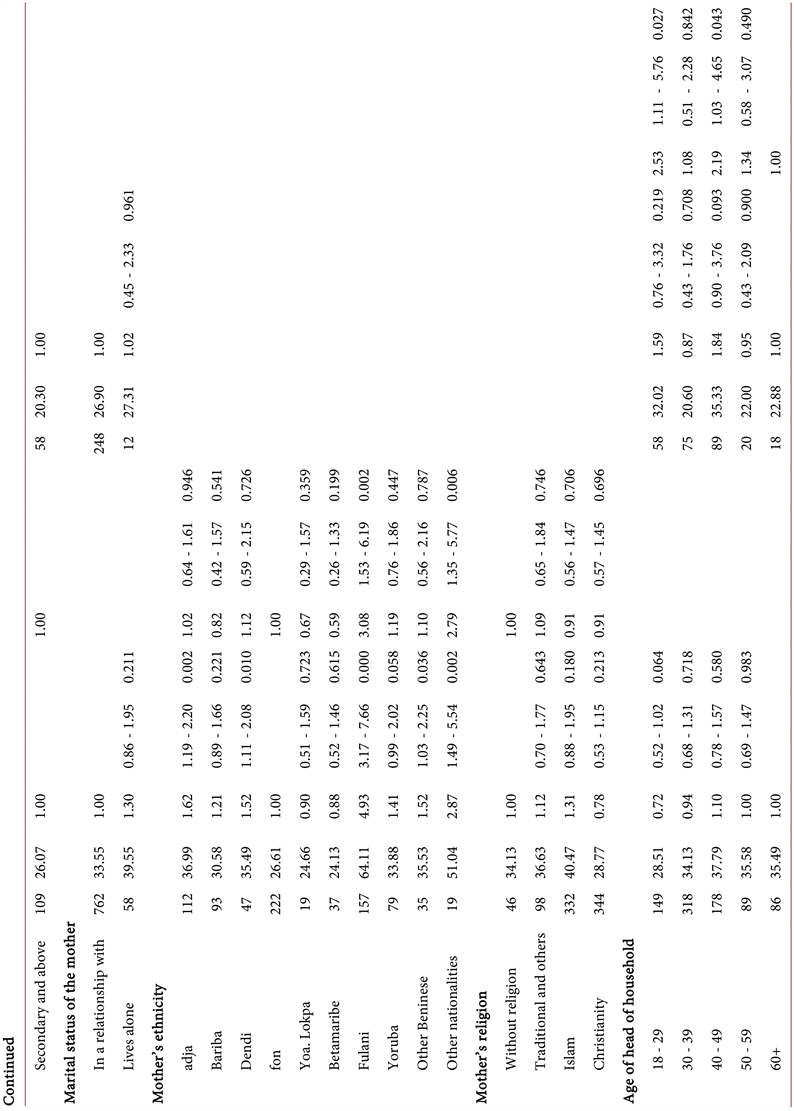
3.2. Religious Affiliation
In Benin, about half (49.41%; 95% CI = 46.35 - 52.47) of children had Christian mothers and 5.61% (95% CI = 4.54 - 6.91) had no maternal religious affiliation. (Table 2). In Togo, nearly half of the children lived in households headed by individuals of the Christian religion (47.97%, 95% CI = 43.35 - 52.63) and 5.95% (95% CI = 4.33 - 8.13) run by individuals with no religious affiliation.
![]()
Table 2. Distribution of children aged 12-23 months in Benin (2017-2018) and Togo (2017) according to the religious affiliation of the mother and the head of household.
![]()
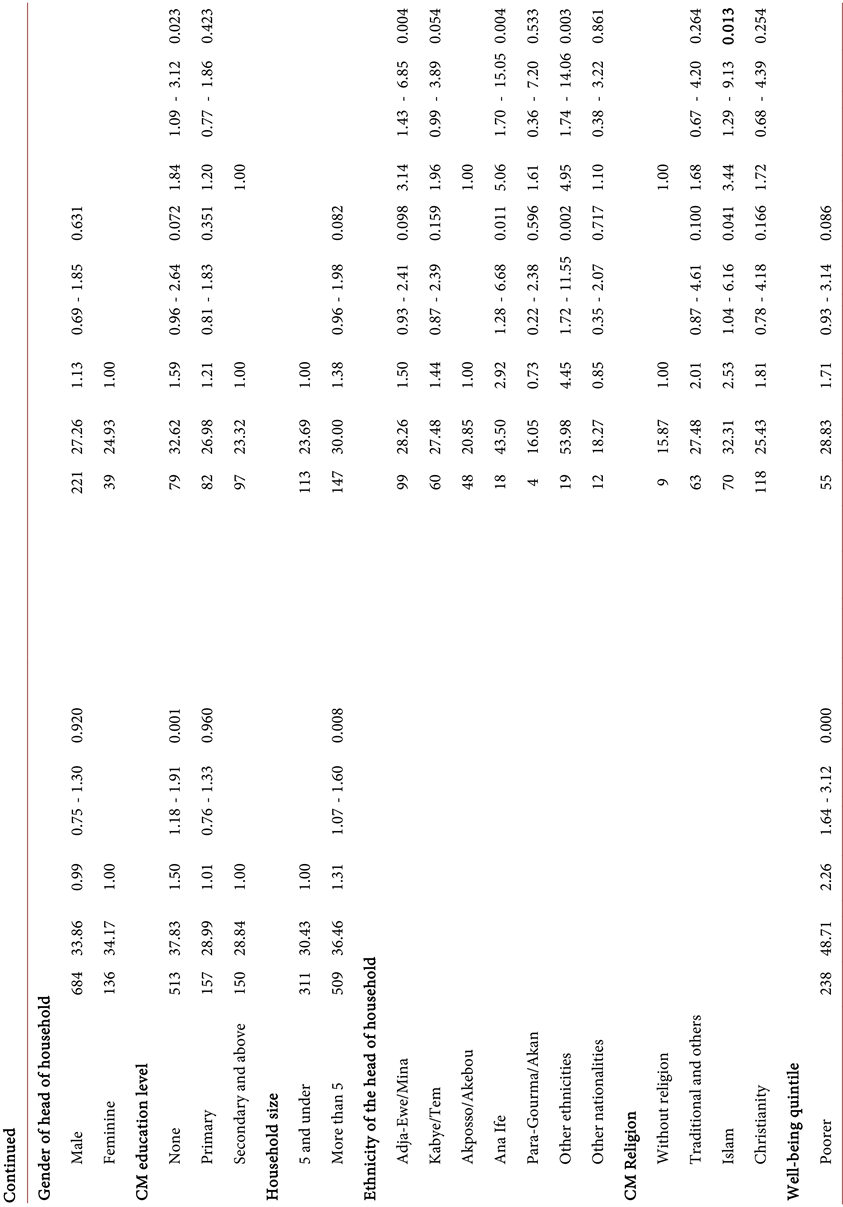
Figure 1. Distribution of children aged 12 - 23 months in Benin (2017-2018) and Togo (2017) according to the religious affiliation of the mother and the head of household
3.3. Prevalence of “zero-dose” Children
The prevalence of “zero-dose” vaccination status in children aged 12 - 23 months was 33.91% (95% CI = 31.67 - 36.23) in Benin. In Togo, this prevalence was 26.88% (95% CI = 23.50 - 30.55).
3.4. Factors Associated with “zero-dose” Vaccination Status
The univariate and multivariate analysis of the factors associated with “zero-doses” are presented in Table 3. We note that the factors associated with “zero-doses” in children aged 12 - 23 months in Togo were: the birth order of the child, the age of the head of household, the level of education of the head of household, the ethnicity of the head of household, the religion of the head of household and the region of residence while those of Benin were: the age of the child, the level of education of the mother, the ethnicity of the mother, and the department of residence.
Concerning Togo, compared to children born in the first position (rank 1), the others were more likely to be “zero-dose”, with a significant difference for ranks 2 - 3 (aOR = 2.27; 95% CI = 1.32 - 3.90) and 4 - 6 (aOR = 2.65; 95% CI = 1.50 - 4.68). Children living in households headed by individuals aged under 60 were more at risk of being “zero-dose”, with a significant difference in the age groups 18 - 29 years (aOR = 2.53; IC95 % = 1.11 - 5.76) and 40 - 49 years (aOR = 2.19; 95% CI = 1.03 - 4.65). Children whose mothers were uneducated (OR = 1.84; 95% CI = 1.09 - 3.12) were more at risk of being “zero-dose” compared to
Table 3. Factors associated with the zero-dose vaccination status of children aged 12 - 23 months, Benin (2017-2018) and Togo (2017).
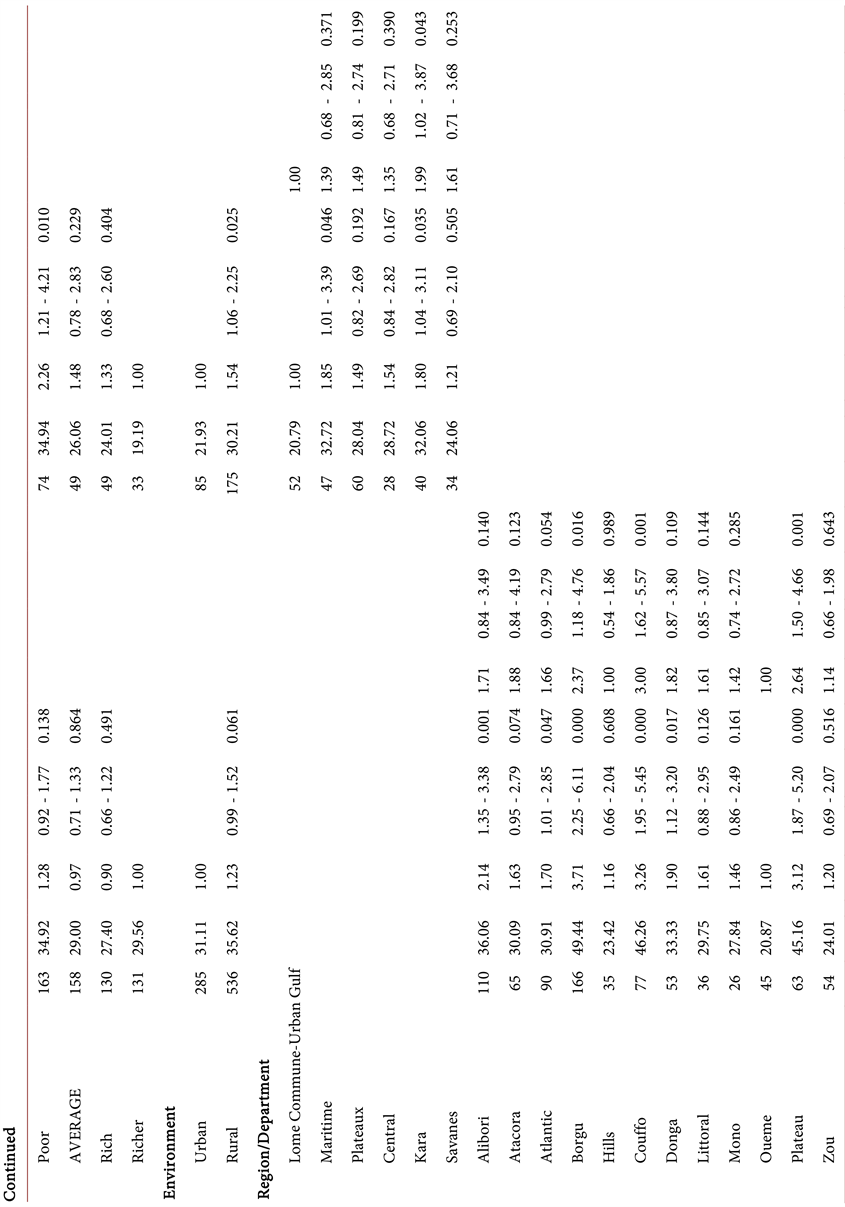
those with mothers with a level of secondary education and more. Adja-Ewe/Mina children (aOR = 3.14; 95% CI = 1.43 - 6.85), Ana-Ife (aOR = 5.06; 95% CI = 1.70 - 15.05) and belonging to other ethnic groups (aOR = 4.95; 95% CI = 1.74 - 14.06) were more at risk of being “zero-dose” compared to those of the Akposso/Akebou ethnic group. Children living in households headed by Muslims (aOR = 3.44; 95% CI = 1.29 - 9.13) were more likely to be “zero-dose” than those from households headed by individuals without religious belief. The risk of being “zero-dose” was multiplied by 1.99 (95% CI = 1.02 - 3.87) in children living in Kara compared to those in Lomé commune-urban Gulf.
For Benin, compared to children aged 12 to 17 months, children aged 18 to 23 months were more likely to be “zero-dose”, with a significant difference for children aged 18 to 23 months (aOR = 1.32; 95% CI = 1.10 - 1.59). Children whose mothers were uneducated (aOR = 1.47; 95% CI = 1.10 - 1.98) were more at risk of being “zero-dose” compared to those with mothers with a level d secondary education and more. Children whose mother’s ethnicity was of other nationalities (aOR = 2.79; 95% CI = 1.35 - 5.77) were more at risk of being “zero-dose” compared to those of the Fon ethnicity. The risk of being “zero-dose” was multiplied by 3 (95% CI = 1.62 - 5.57) in children living in the department of Couffo, multiplied by 2.64 (95% CI = 1.50 - 4, 66) in children living in the Plateau department and multiplied by 2.37 (95% CI = 1.18 - 4.76) compared to those in the Ouémé department.
Moreover, in Benin, by adjusting for the age of the children, the level of education and the ethnicity of the mother as well as the department of residence, there is no evidence in favour of an influence of the religious affiliation of the mother on the “zero-dose” vaccination status of the children. In Togo, after adjusting for the rank of the child, the age, level of education and ethnicity of the head of household, as well as the region of residence, children living in households where the head was a religious woman were three times (aOR = 3.44; 95% CI = 1.29 - 9.13) more likely to be zero-dose than those from households headed by individuals with no religious belief.
4. Discussion
In the present work, the aim was to study the influence of religion on the “zero-dose” vaccination status of children aged 12 - 23 months in Benin and Togo.
We found that the prevalence of “zero-dose” vaccination status in children aged 12 - 23 months in Benin and Togo was 34.61% and 26.88% respectively. These frequencies are higher than what is recorded on average in the WHO African region, with 20% [4] . In the West African sub-region, the following prevalences are observed based on vaccination cards: 3.80% in Senegal (2019) [42] , 7.7% in Gambia (2019 - 2020) [43] , 12.8% in Ghana (2014) [44] , 26.4% in Sierra Leone [45] , 36.3% in Liberia [46] , 45.9% in Mali [47] , 54.3% in Guinea (2018) [48] , 62.1% in Nigeria [49] . Several factors may explain the observed differences: the heterogeneity of vaccination programs between countries, and the financial and logistical resources available to implement these programs; differences in the implementation of different communication strategies for development and for social behaviour change, differences in levels of knowledge as well as attitudes of parents and communities regarding the benefits of vaccination, as well as their adherence recommended vaccination practices. In addition, in Asia, percentages varying from 1.50% in Bangladesh to 27.10 in Laos are observed with in particular: 3.10% in Thailand, 3.80% in Vietnam, 6.10% in Cambodia, 10, 50% in India, 10.50 in Nepal, and 13.30% in Iraq [24] . It should be noted that these prevalences reported in Asia were established on the basis of vaccination records and declarations from mothers; which was not the case in the present study [24] .
In Benin, there is no evidence in favour of a relationship between the religious affiliation of mothers on the “zero-dose” vaccination status of their children. On the other hand, we noted a significant influence of the religious affiliation of the head of household on the “zero-dose” vaccination status of children in Togo. Children living in households headed by Muslims were three times more likely to be zero-dose than those from households headed by individuals with no religious beliefs. Ashwin et al. had made the same observation in India in 2005. It was noted that 83.7% of infants in Hindu households were fully vaccinated while 2.4% were not, against 56.0% fully vaccinated and 16.0% unvaccinated in Muslim households [50] . Similarly, Johri et al. also found in their study in India that Muslim households were 1.72 times more likely to have zero-dose children compared to Hindu households [42] .
The negative influence of affiliation to the Muslim religion on the vaccination status of children has been documented by previous work [22] [23] [24] . A review of the literature in Nigeria in 2022 highlighted lower vaccination coverage among children from Muslim households compared to those from Christian households [22] . In addition, in a multicenter study in 2022, after adjusting for potential confounders, the likelihood of children being “zero-dose” was 76% higher among those living in Muslim households compared to households Christian [24] . According to a study in 2016, the Muslim religion is not always linked to low vaccination coverage, as evidenced by the case of Saudi Arabia where vaccines are widely accepted [51] . In a recent study (2022), the authors pointed out that vaccine hesitancy among Muslim women does not appear to be motivated by a theological basis, but rather by beliefs within specific communities [24] . On the other hand, previous studies in Zimbabwe, Papua New Guinea and India have shown that religion does not have a significant influence on full immunization coverage in children [25] [26] [27] . Further research is needed to understand the basis for the excess risk of “zero-dose” vaccination status in children that appears to be associated with the Muslim religion. Furthermore, from a broader perspective, the influence of religious affiliation on vaccination status highlights the importance of strengthening the involvement of religious leaders in vaccination activities.
In addition to the religious affiliation of the head of household, the other predictors of “zero-dose” vaccination status were the rank of the child, the age, the level of education and the ethnicity of the head of household as well as the area of residence of the household. In Benin, it was the age of the child, the level of education and ethnicity of the mother and the region of residence. Overall, these results support the findings of other work.
We can identify some limitations to this study. The information regarding religion in the DHS-V in Benin concerned mothers of children, whereas in the MICS6 in Togo, the question applied to the head of household; it is not possible to assess to what extent this affected the results obtained. The study took into account the major religious groups without distinguishing between the different currents of thought; for example, Catholicism, Protestantism, Evangelical Churches, etc. for Christianity. Moreover, since the study is based on the use of existing databases, it does not include all the variables that could be evoked as predictors of “zero-dose” vaccination status, for example, knowledge and attitudes of mothers or heads of household towards vaccination.
5. Conclusion
This study is a continuation of recent work on the predictors of the “zero-dose” vaccination status of children. The prevalence of “zero-dose” vaccination status in children was 34.61% in Benin and 26.88% in Togo. In Benin, there is no evidence in favour of a relationship between the religion of mothers and the zero-dose vaccination status of children. On the other hand, in Togo, children living in households whose head was of the Muslim faith were more at risk of being “zero-dose” than those coming from households headed by individuals without religious belief. Additional quantitative studies associated with qualitative work are necessary to clarify the significance or otherwise of the link between the religious context in which children live on their vaccination status and the foundations of this relationship, if any.
Contributors
NTM, AK, JZS, ABS, MTG, YTT, DEL and AEK provided study design and validity. They interpreted the analysis and wrote the first version of the manuscript. NG supported data analysis, proofreading of the project. All authors were responsible for reviewing and editing the manuscript. All authors confirm that they have had full access to all study data and accept responsibility for the decision to submit for publication.
Data Sharing
This study is based on publicly available data from the sixth global round of Multiple Indicator Cluster Surveys (MICS 6) conducted in Togo in 2017 and the fifth global round of Demographic Health Surveys conducted in Benin between 2017 and 2018. The data set that supports the findings of this study can be downloaded through the Demographic and Health Surveys and Multiple Indicator Cluster Surveys Program Data Dissemination System.
Source of Funding
There was no funding source for this study at this time.