Resistance to Fluoroquinolones and Other Antimicrobials in Culture-Positive Salmonella typhi Isolates in Gulbarga, South India ()
1. Introduction
Typhoid fever etiological agents, Salmonella typhi and Paratyphi A, are causing diverse clinical manifestations worldwide. Estimation of typhoid fever episodes over a decade period (2004-2014) was found to be 13.5 - 21.1 million cases [1]. Various factors influence the incidence of enteric fever. Transmission routes, personal hygiene management, emerging of multidrug resistance strains, prolonged carrier stages are governing factors for the emerging risk of the enteric infections. Though, the enteric fever is now less common in developed countries, many developing countries with limited resources are still facing this menace [2]. Globally, 217,000 deaths are attributable to typhoid fever annually with the highest disease burden in South central and Southeast Asia. Infants, children and adolescents are more likely to get typhoid fever in these regions. Nearly, 80% of the total typhoid fever cases have been reported in eight South Asian countries (Bangladesh, China, India, Indonesia, Laos, Nepal, Pakistan and Vietnam), suggesting typhoid fever to be a major health risk in the region [3] [4].
Untreated enteric fever carries with a mortality rate of 30%, with appropriate antimicrobial treatment reduces the mortality rate to as low as 0.5% [5]. Sometimes it is often necessary to commence treatment with immediate effect to reduce the severity of infections. Fluoroquinolone, ciprofloxacin are choice of drugs for treatment, especially when treatment miscarries with traditional antimicrobial agents comprising chloramphenicol, ampicillin and trimethoprim-sulfamethoxazole (cotrimoxazole) [5]. Multidrug-resistant typhoid fever (MDRTF) is defined as typhoid fever caused by S. typhi strains which are resistant to all the three first-line recommended drugs for treatment, i.e., chloramphenicol, ampicillin and trimethoprim-sulfamethoxazole (cotrimoxazole) [6]. However, this switch to ciprofloxacin has led to a subsequent increase in the occurrence of S. typhi isolates resistant to this antimicrobial agent across the globe, including in India [7] [8].
In Salmonellae, quinolone resistance is usually associated with mutations in the quinolone resistance-determining region (QRDR) of the A subunit of DNA gyrase, though the presence of plasmid-mediated quinolone resistance qnr genes and aac(6’)-Ib-cr has also been described in quinolone-resistant non-Typhoid Salmonella [9]. The association of quinolone resistance with mutations in the genes encoding for DNA gyrase, causes reduced drug accumulation, either by a decreased uptake or by an increased efflux. The exact mechanism of this DNA gyrase-mediated resistance in S. typhi is not fully understood, though various studies have found that single point mutations in this region confer resistance to nalidixic acid and hence reduced susceptibility to Fluoroquinolones [10]. Worldwide there are sporadic reports of high level cephalosporin resistance in typhoidal Salmonellae [11] [12].
A number of cultural, social and environmental factors are associated with the occurrence of typhoid in different endemic settings of which poor quality of life, inadequate provision of safe water and sanitation are found to be the major causes [13]. Gulbarga region, falling under the Hyderabad Karnataka area, is considered to be socio-economically and educationally backward and Typhoid is endemic in this region occurring at regular intervals (Picture 1).
Therefore, this study was undertaken to characterize trends in antimicrobial resistance in clinically relevant S. typhi isolates and environmental isolates originating from Gulbarga, South India, to help clinicians in constituting a more effective treatment regimen.
2. Materials and Methods
Bacterial culture and identification
S. typhi isolates from a total of 1200 clinical samples like Blood, CSF and Urine samples from patients presenting with fever at the outpatient clinics or were admitted in the private and government hospitals of this region and 50 environmental samples from sewage, water and food during the period from August 2006 to September 2009 were included in the study. The patients ranged in age from 2 years to 75 years (median, 40 years). Blood samples were cultured by clot and blood culture methods, while the cerebral spinal fluid (CSF) samples were cultured directly by plating and the urine and stool samples were cultured by using Selenite F broth (Hi-Media Laboratories Ltd, Mumbai). All the biological samples were collected from the same area of the study and the samples were based on the positive Widal test result of the patient, irrespective of the organ affected. Colonies were identified as S. typhi on Wilson and Blair bismuth sulphite agar medium and Xylose-lysine deoxycholate agar (XLD) (Hi-media Laboratories Pvt Ltd, Mumbai, India) using standard biochemical methods [14], and confirmed using Salmonella polyvalent O, O9 and H: d antisera procured from King Institute of Preventive Medicine, Guindy, Chennai, South India.
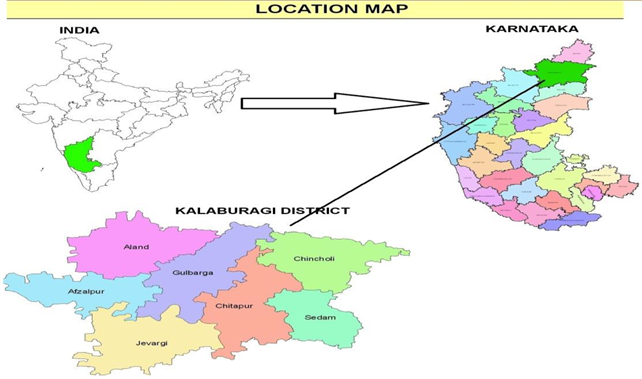
Picture 1. Study area map of Gulbarga district.
Antimicrobial susceptibility testing
Isolates were tested for susceptibility to antibiotics using the Kirby Bauer disk diffusion method. Mueller Hinton agar plates were inoculated with a standardized inoculum of 0.5 McFarland (approximately 108 CFU/ml) over the entire surface. Antibiotic disks were dispensed to the agar surface with the forceps and incubated at 37˚C for 16 to 18 hours in ambient air and diameter of inhibition zones were measured and results were interpreted according to the Clinical and Laboratory Standards Institute (CLSI) guidelines (CLSI, 2013) [15]. Reduced susceptibility to ciprofloxacin was determined as a minimum inhibitory concentration (MIC) of 0.125 - 1.0 μg/ml. The breakpoint for ciprofloxacin is, ≤0.5 μg/ml (susceptible) and >1 μg/ml (resistant) according to the CLSI guidelines (CLSI, 2013) [15]. Escherichia coli ATCC 25922 were used as a standard control. Nalidixic acid susceptibility was used as a screening test for reduced susceptibility to ciprofloxacin [16]. MICs were determined by agar dilution for ampicillin, chloramphenicol, co-trimoxazole, ceftriaxone, ceftazidime, cefotaxime, ceftizoxime, ciprofloxacin and nalidixic acid separately.
Molecular analysis of quinolone resistance
Molecular analysis of quinolone resistance was performed for 20 nalidixic acid resistant (1 ciprofloxacin resistant and 19 ciprofloxacin susceptible) isolates. The molecular mechanism of quinolone resistance was determined by investigating mutations in the QRDRs of DNA gyrase (gyrA and gyrB) genes, according to the previously described protocols [17] [18].
PCR amplification of gyrA gene
Amplification of gyrA gene was performed with primers Forward 5’-ATG AGC GAC CTT GCG AGA GAA ATT ACA CCG-3’ and Reverse 5’- TTC CAT CAG CCC TTC AAT GCT GAT GTC TTC-3’ [17].
The cycling conditions include Preheating at 94˚C for 5 min for 1 cycle, and Denaturation at 94˚C for 30 sec, Primer Annealing at 55˚C for 30 sec and Elongation at 72˚C for 45 sec for 35 cycles. Lastly final elongation was done at 72˚C for 10 min. The size of amplicon was 620 bp by using ABI (Applied Biosystems) PCR.
Electrophoresis
PCR products were loaded on to 1% agarose gel along with 500 bp ladder using 1XTBE Buffer containing Ethidium Bromide for 20 to 30 minutes at 130 volts and observed using UV transilluminator (UV-Tech).
3. Results
Trends in antimicrobial susceptibility of S. typhi isolates
A total of 100 S. typhi strains isolated during the period 2006-2009 from various health care settings. All Salmonella typhi isolates were from blood samples and Environment samples such as contaminated water samples. However, environmental samples are all susceptible for all antibiotics used in this study. 40% (40/100) were fully susceptible to all the antibiotics tested; 9% (9/100) were MDR; 30% (30/100) were nalidixic acid resistant (NAR); and 1% (1/100) was both MDR and NAR (MDR being defined as resistance to all the first line antimicrobials i.e. ampicillin, cotrimoxazole and chloramphenicol). The results are summarized in Table 1. Only two isolates (2%) were resistant to ciprofloxacin (MIC- ≥ 1 µg/ml) (CLSI Guidelines, 2017) (Table 4). There was a steady decline in the number of MDR isolates over the 4 year study period, as well as a parallel increase in NAR (non-MDR) isolates (Table 1 and Table 2).
All 30 nalidixic acid resistant isolates were performed for MIC for Nalidixic acid. 20 NAR isolates were chosen for ciprofloxacin MIC randomly, and a single isolate possessed an MIC of ≥4 μg/ml for ciprofloxacin with the corresponding agar dilution method. Ciprofloxacin MICs for nalidixic acid resistant isolates ranged between 0.125 - 4 μg/ml. A correlation was observed between reduced ciprofloxacin susceptibility and nalidixic acid resistance (19/20 isolates with ciprofloxacin MICs ranging from 0.125 - 1 μg/ml were NAR). The value of R is 0.1602 for Pearson correlation test. Although technically a positive correlation, the relationship between two variables is weak correlation (Figure 1).
All isolates were found to be susceptible to cephalosporins though interestingly there was a gradual increase in MIC values for ceftizoxime and ceftriaxone during the study period from 0.125 - 1 μg/ml (Table 3). All environmental isolates were found to be susceptible to all the antibiotics tested.
Molecular analysis of quinolone resistance
PCR amplification of gyrA gene, nucleotide changes within DNA gyrase (gyrA) gene and their relationship between ciprofloxacin MIC investigated for 20 NAR isolates, with different resistance profiles are shown in Figures 2(a)-(c) and Table 4 respectively. Comparatively, 18 NAR isolates found, with reduced susceptibility to ciprofloxacin (MIC 0.125 - 1 μg/ml) (GenBank accession no. HQ176349-HQ176357 and HQ176359-HQ176366 and HQ176368). Remaining two NAR isolates exhibit exceptional features. One strain (ST-54) with higher MIC ≥ 4 μg/ml for ciprofloxacin has a single gyrA mutation within the QRDR of gyrA, at position Ser83. Sequence of gyrA submitted to NCBI and its GenBank accession no. HQ176358. Another one (ST-77) having reduced ciprofloxacin susceptibility (0.125 µg/ml; GenBank accession no. HQ176367) does not show any mutation at Ser83 in QRDR region of the gyrA.
![]()
Table 1. Distribution of antimicrobial resistance phenotypes among S. typhi isolates.
aSusceptible to all the antibiotics; bSingle resistance—resistance to only one antimicrobial; cPaired resistance—resistance to two antimicrobials; dMultiple resistance—resistance to three and more than three antimicrobial; eMDR—defined as resistance to ampicillin, chloramphenicol and cotrimoxazole.
![]()
Table 2. Trends in resistance to quinolones among S. typhi isolates during the study period.
CIPR—Ciprofloxacin resistance; NARR—Nalidixic acid resistance.
![]()
Table 3. MIC values for Cephalosporins.
![]()
Table 4. Relationship between ciprofloxacin MIC, point mutations within the QRDRs of DNA gyrase gene for 20-seleced serovar Typhi isolates.
![]()
Figure 1. Pearson correlation. The value of R is 0.1602. Although technically a positive correlation, the relationship between the variables is weak. The value of R2, the coefficient of determination, is 0.0257. Where X Value for reduced ciprofloxacin susceptibility, Y Value for Nalidixic acid resistance.
![]() (a)
(a) ![]() (b)
(b) ![]() (c)
(c)
Figure 2. (a) PCR amplification of gyrA gene, M-500 bp DNA Ladder, ST11: (S. typhi Isolate) and C: Control (S. typhi MTTC: 734); (b) PCR amplification of gyrA gene, M-500 bp DNA Ladder, ST12-ST54: S. typhi Isolates; (c) PCR amplification of gyrA gene, M-500 bp DNA Ladder, ST55-ST80: S. typhi Isolates.
4. Discussion
Salmonella typhi accounts for a major proportion of enteric fever in developing countries such as India. In the present study, a gradual decline observed in the number of S. typhi MDR isolates. Similar reports found from other regions of South India [7]. 30% S. typhi isolates were resistant to NAR and showed reduced susceptibility to ciprofloxacin. This finding is most likely due to decreased prescribing of traditional antimicrobial agents, and an increasing reliance on ciprofloxacin as the first line treatment for S. typhi in Gulbarga, which is in accordance with Rudresh et al. [8]. All environment samples are susceptible to all antibiotic used. Environment is a media of transmission for typhoid fever [19].
Indeed, only 2% of S. typhi isolates from positive cultures in Gulbarga were found to be resistant to ciprofloxacin (MIC ≥ 1 and 4 μg/ml), and the emergence of such resistant bacteria is a cause for concern. In recent years, there are some sporadic reports of high-level ciprofloxacin resistance in Salmonella typhi [8]. Capoor et al., in 2007 reported ciprofloxacin resistance rate of 1% in Salmonella typhi isolates [20]. However, isolates with reduced susceptibility to ciprofloxacin (≥0.125; NAR-isolates) have a less favorable response to ciprofloxacin [5].
In our study, one S. typhi isolate ST-54 with a ciprofloxacin MIC ≥ 4 μg/ml, is found to have a single mutation in gyrA (ser 83 to phe) and other strain with lower MICs (0.125 μg/ml - 1.0 μg/ml) also exhibits single point mutations. Our report was contrary to the earlier reports [19] [20] who had found complete resistance to ciprofloxacin (MIC ≥ 4 μg/ml) due to a double mutation in the QRDR region. Menezes et al. (2012), studies focus on NAR isolates with a comparatively reduced susceptibility to ciprofloxacin (MIC 0.125 - 0.5 mg/L), possessed a single gyrA mutation (either at Ser83 or Asp87) only. Resistance mutations of gyrA have been clustered in a region of the gene product between amino acids 67 and 106 termed the QRDR. Gyrase appears to be the primary target for quinolones in gram-negative bacteria since missense mutations in gyrA genes are sufficient to render quinolone resistant in these organisms [21]. gyrA and Par C mutations in QRDR region render quinolone and fluoroquinolones resistance. However, the single mutation in gyrA Ser83 to Phe, Try, Ala, is most common mechanism, for NAR isolates show reduced susceptibility to ciprofloxacin [22]. In the present study there is a single mutation in Ser 83 to Phe, it supports the MIC studies of S. typhi isolate ST54 for Ciprofloxacin resistance.
There was a gradual increase in MICs against ceftriaxone, ceftazidime, cefotaxime and ceftizoxime (a 3rd generation cephalosporin) during the study period, from a MIC value of 0.125 μg/ml in 2006 to 1 μg/ml in 2009, though still well within the susceptible range. This type of resistance to quinolones, and more recently, increase in MIC levels to third and fourth-generation cephalosporins, re-emphasize the importance of continued surveillance in the treatment of enteric fever [23].
5. Conclusions
In our study we found that typhoid fever is endemic in this region. In our experience, nalidixic acid disk diffusion testing is a good indicator of decreased ciprofloxacin susceptibility. A high-level ciprofloxacin resistance (MIC ≥ 4 μg/mL) in single S. typhi isolate is mediated by a single mutation in gyrA. There is a slow emergence of ciprofloxacin resistant typhoidal Salmonellae in this part of south India. A low level of ciprofloxacin resistance was observed, with steadily increasing NAR, but decreasing MDR isolations over the study period. This is most likely due to an increased use of ciprofloxacin as a first line drug of choice for enteric fever. Furthermore all typhoidal Salmonellae were found to be susceptible to third-generation cephalosporin.
Hence in order to better manage and prevent the spread of antimicrobial resistance, both clinicians and governments require accurate epidemiological information. At the present moment, this information tends to be lacking, especially in countries with large populations and unrestricted “over the counter” prescription policies, such as India. The spread of nalidixic acid resistant S. typhi with reduced susceptibility to ciprofloxacin necessitates a change towards “evidence-based” treatment practices for the treatment of typhoid fever, not least in Southern India.