Evaluation of the Neurodevelopmental Outcome of Toddlers with Spinal Dysraphism after Surgical Repair Using ASQ-3™ Scores ()
1. Background
Spina bifida literally means “spine in two parts” or “open spine” [1] . Spinal dysraphism involves a spectrum of congenital anomalies resulting in a defective neural arch through which meninges or neural elements are herniated, leading to a variety of clinical manifestations [1] [2] . They are divided into aperta (a visible lesion) and occulta (with no external lesion) [1] [2] . Meningocele, myelomeningocele, lipomeningomyelocele, myeloschisis, and rachischisis are the usual names associated with them depending on the pathological findings. Meningocele, by definition, involve only the meninges with no neural involvement; others have a variable extent of neural involvement. The spina bifida aperta is usually associated with a skin defect with an impending risk of CSF leak, constituting “open defects,” whereas the occult forms have normal skin cover. Both forms demand different approaches to management. The clinical importance of occult lesions has grown tremendously in recent years.
The large number of children suffering from spina bifida and hydrocephalus, though the detection was sporadic by the pediatricians in the past. With the awareness and growth of neurosurgery referral centers, special clinics were established with the ability to address these problems. Gradually, with the availability of magnetic resonance imaging (MRI), several such anomalies were identified, especially of the occult variety. This also helped to visualize a variety of underlying anomalies and their clinical consequences.
After pediatric neurosurgery became a subspecialty, several neurosurgeons took an interest in this field and contributed to its early detection. Furthermore, there has been a steady decline in these anomalies over the last decade. Folic acid fortification has contributed. Fortification can serve as an effective strategy to prevent neural tube defects (NTDs) in populations where access to folic acid-rich foods or supplements is limited. This review provides an overview of mandatory folic acid (FA) fortification in 71 countries and the research findings on its impact. The programs have shown significant reductions in NTD rates, with reductions of up to 78%. Additionally, blood folate concentrations increased by approximately 1.47 times after fortification. Various health outcomes have also been positively influenced by fortification. As a result, the anomalies that are not compatible with life and the severe anomalies with major defects have decreased, leading to social comfort [3] .
In this study, we aimed to address the Neurodevelopmental outcomes of Sudanese toddler patients with spinal dysraphism after surgical repair with or without a VP shunt using ASQ-3TM Scores.
2. Methodology
This is a cross-sectional retrospective hospital-based study conducted at the National Center for Neurological Sciences (NCNS) in Khartoum, Sudan which serves as the primary tertiary hospital in Sudan. This facility plays a crucial role in providing healthcare services to approximately 40 million people in Sudan. Notably, it handles over 95% of all myelomeningocele surgeries in the country. Additionally, it is the sole institution offering elective public surgery services in Sudan.
The study population included all patients who are defined as toddlers (1 - 3 years old) and diagnosed with any of the spinal dysraphism disorders and admitted for surgical repair either for spinal deformity like myelomeningocele repair alone or with VP shunt insertion, which is operated in the NCNS, in the period from 1/1/2017 to 31/12/2019, and there were 84 cases in total. We included the entire patient population who underwent surgery during the specified period, with the sole exception being those who met the exclusion criteria. In essence, our study encompassed all eligible patients, ensuring a total coverage sample size.
The exclusion criteria for the study encompassed several aspects. Patients were excluded if they declined participation in the study, presented with concurrent congenital conditions such as congenital heart disease or other significant congenital disorders unrelated to the primary research focus, if their contact information was unavailable or died before 1 year. These criteria served as the sole basis for excluding individuals from the study.
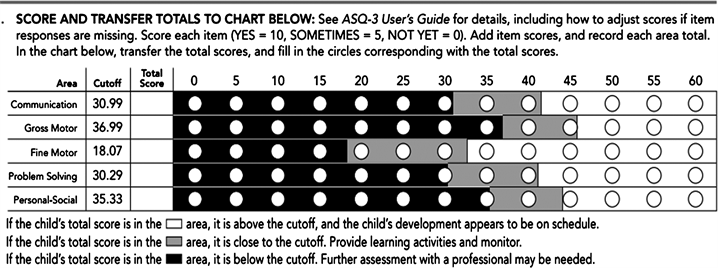
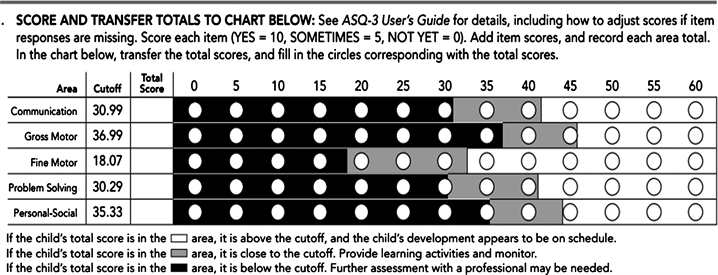
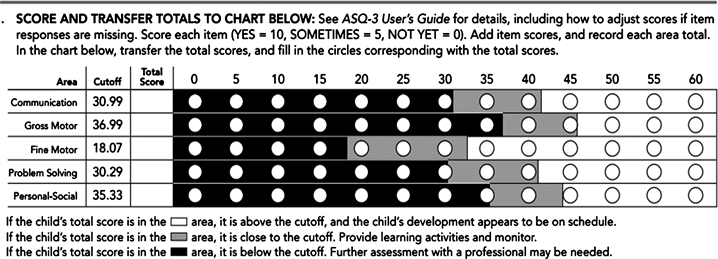
Data is collected by a constructed questionnaire, including ASQ-3TM Scores, which assess gross and fine motor skills, communication, problem solving, and personal and social development. Self-regulation, compliance, social communication, adaptive functioning, autonomy, affect, and interaction with people. Ages & Stages Questionnaires®, Third Edition (ASQ®-3) is a developmental screening tool that pinpoints developmental progress in children between the ages of one month to 5 1/2 years. Its success lies in its parent-centric approach and inherent ease-of-use—a combination that has made it the most widely used developmental screener across the globe. ASQ-3 screens and assesses the developmental performance of children in the areas of communication, gross motor skills, fine motor skills, problem solving, and personal-social skills
Data were processed and analyzed using the Statistical Package for Social Science (SPSS) computer program. Version 25.0. Study aimed to evaluate neurodevelopment outcome of toddler with spinal dysraphism after surgical repair and to evaluate the impact of post-operative complication in neurodevelopment.
3. Ethical Considerations
Informed consent was taken from the participant parents and patients privacy and confidentiality taken into consideration.
4. Results
The gross motor assessment showed the majority of patients (73.8%) need further assessment with professionals, while 7 (8.3%) need to be provided with learning activities and monitored, and only 15 (17.9%) of patients have gross motor development appears to be on schedule (Table 1).
Fine motor assessment showed that nearly half of the patients (46.5%) On the other hand, 15 of the patients (17.9%) necessitate learning activities and checks, and only about a third (35.7%) of patients have fine motor development, which appears to be on schedule (Table 2).
Problem-solving assessment showed that 39 of patients (46.4%) need further assessment with professionals, while 9 (10.7%) need to be provided with learning activities and monitored, and 36 (42.9%)’s problem-solving development appears to be on schedule (Table 3).
![]()
Table 1. Patient’s distribution according to their mother attendance to ANC, and receiving folate supplement after conception.
![]()
Table 2. Patient’s distribution according to type of surgery they underwent.
Nevertheless, personal social assessment revealed that the majority (57, 67.9%) of patients need further assessment with professionals, while 18 (21.4%) need to be provided with learning activities and monitored, and only 9 (10.7%) of their personal social development appears to be on schedule (Table 4).
Our results provide a symptomatology: 6 of the patients (7.1%) had their parents declare that they have hearing difficulty; additionally, 27 (32.1%) had their parents state that they do not talk like other toddlers their age; moreover, a quarter of patients (22.5%) had their parents report that they do not understand what they say; in addition, 57 (67.9%) of children don’t walk, run, or climb like other toddlers as their parents state; only 3 (3.6%) of parents had concern about their child’s vision; half of patients (50%) had medical problems; but only 12 (14.3%) of parents had concern about child behavior (Table 5).
The cross-tabulation results showed that there was a statistically significant association between complications and communication development (P value = 0.017, Table 6), problem-solving development (P value = 0.029), Personal social development (P value = 0.028, Table 7), and Table 8.
![]()
Table 3. Common post-operative complications among patients.
![]()
Table 4. Communication assessment result among patients using ASQ-3™ Scores.
![]()
Table 5. Gross motor assessment result among patients using ASQ-3™ Scores.
![]()
Table 6. Fine motor assessment result among patients using ASQ-3™ Scores.
5. Discussion
84 patients were included in this study; 51 patients, which constituted 60.7%, were 2 years old, and 33 (39.3%) were 3 years old, Figure 1. In this study, there were 45 males (53.6%) and 39 females (46.4%), as shown in Figure 2. Moreover, in this study, 45 of the patients whose mothers attended antenatal care irregularly and 54 (64.3%) of their mothers didn’t receive folate supplements (Table 9).
![]()
![]()
Table 7. Problem solving assessment result among patients using ASQ-3™ Scores.
![]()
![]()
Table 8. Personal social assessment result among patients using ASQ-3™ Scores.
![]()
Figure 1. Patients distribution according to age, n = 84.
![]()
Figure 2. Patients distribution according to gender, n = 84.
![]()
Table 9. Other assessment result among patients using ASQ-3™ Scores.
Furthermore, 44 patients (52.3%) had MMC repair, while 40 (47.7%) had both repair and PV shunt (Table 10), with a mean age of 73.269.0 days.
When we came to postoperative complications, infection was the most common reported complication and was seen in 12 (14.3%) of patients, followed by VP shunt revision in 9 (10.7%) of patients (Table 11). In this context, the mean age at VP shunt revision was 51.7 months (range 3 - 7 months).
Furthermore, communication assessment using ASQ-3TM Scores showed that 30 of the patients (35.7%) need further assessment with professionals, while 15 of the patients (17.9%) need to be provided with learning activities and monitored. The rest of the patient’s communication development appears to be on schedule, as shown in Table 12.
Spinal dysraphism is the most common survivable congenital defect of the central nervous system. We are still lacking the ability to correct the deficits that lead to spinal dysraphism. Our current hope is for novel therapies and optimized
![]()
Table 10. Complications and communication development cross-tabulation.
![]()
Table 11. Complications and Problem-solving development, cross tabulation.
![]()
Table 12. Complications and personal social development, cross tabulation.
medical and surgical management to provide improved outcomes and quality of life for these patients. In this study, we aimed to assess the neurological outcome of patients with spinal dysraphism after surgical repair and VP if it is done with a shunt. Eighty-four patients were included in this study; out of them, 51 (60.7%) were 2 years old, and 33 (39.3%) were 3 years old.
Although there is no evidence that the gender of the child influences the risk of developing spinal dysraphism, Overall, it’s more common in females than in males. This study showed a slight male predominance of 1.1:1, in contrast to previous studies, which revealed that the general population had a slight female predominance [4] [5] . Moreover, Tubbs RS’s study stated that women are three times more likely than men to have spinal dysraphism [6] .
The decreased incidence of NTDs is largely due to the prevention of folate deficiency, a risk factor that was implicated as early as the 1960s but not fully appreciated until the late 1980s and early 1990s. Numerous studies have demonstrated a relationship between lower maternal folate levels and a decreased incidence of spinal dysraphism. In addition, randomized clinical trials helped establish the 4 mg/day recommendation for high-risk mothers, defined as women with a previous pregnancy complicated by an NTD [7] .
The methods available for increasing the consumption of folate were alterations in dietary habits, supplementation, and fortification of food. In 1996, the Food and Drug Administration (FDA) authorized folate fortification and, by 1998, mandated it [8] . As of 2021, over 78 countries have mandated folic acid fortification in their flour [9] . Despite the mounting evidence of a decreased incidence of NTDs with folate supplementation, there are still many countries that forgo fortification and continue to have a significant number of births complicated by NTDs. Our data showed that 53.6% of patients mothers did not attend ANC regularly, and 64.3% of patients their mothers didn’t receive folate supplements. As well published in the literature, spinal dysraphism can be prevented by preconception folic acid [10] . The rostral and caudal neural pores close at 6 weeks of gestation. A delayed folic acid supplementation is bound to miss the vital periods of organogenesis and neural tube closure. It is imperative to supplement our cereal grains with folic acid and vitamin B12 to prevent the social and economic burden of birth defects. This strategy has already benefited developed countries [11] .
On the other hand, Hydrocephalus has until now been considered an almost inevitable sequela of spinal dysraphism in general and especially myelomeningocele. In the neurosurgical literature, reported rates of shunt placement are ~ 80%. It is a neurosurgical aphorism that “the ideal shunt is no shunt.” The shunt placement rate in patients with myelomeningocele has historically been quite high. Studies suggest that patients with myelomeningocele who have had CSF diversion have reduced longevity compared with patients who have not required shunt placement for CSF diversion [12] [13] . The mean IQ has been reported to be higher in children with myelomeningocele who have not required shunt placement than in those who have. Clearly, this observation may simply reflect the severity of the disease; the more severe the malformation, the more likely the need for shunt placement, but it is difficult to deny the long-term adverse effects of shunt-related complications in this group, as evidenced by this and other similar studies. This study showed that according to type of surgery, 52.3% of patients underwent MMC repair only, while 47.7% underwent MMC repair and VP shunt, while a cohort study performed by McDowell MM et al. [14] documented a higher percent. 88% of patients with spina bifida underwent CSF shunting; Waqar Aziz R. et al. [15] reported that 76% had CSF shunting. On the other hand, a study in India reported that VP shunts are seen in only 25% of cases [16] , which is considered the lowest frequency.
Shunt-related complications, including death, have been reported to be greater in patients with myelomeningocele than in those who required shunt placement for the treatment of other conditions. McDowell MM [17] and others have suggested that it is the infective complications of shunt-treated hydrocephalus rather than the hydrocephalus per se that have the greater impact on intelligence in this population. The need for multiple shunt placement procedures also seems to have a negative effect on the long-term outcome [18] . There is also good evidence to suggest that the IQs of patients with myelomeningocele who do not undergo shunt placement are higher than those of their shunt-treated counterparts. In this study, the most Common postoperative complications reported by our patients were infection in 12 (14.3%) of patients, followed by VP shunt revision in 9 (10.7%) of patients, Gursoy K. et al.’s [19] study found that 32.1% of patients had postoperative complications. Demir N. et al. [20] found that following MMC repair, 30 (27.3%) of the patients developed infection, with meningitis/shunt infection in 18 (16.4%) and wound infection in 12 (11%). Our study revealed that Patients who did not experience any post-operative complications showed statistically significant better neurological development (P value = 0.041). This is consistent with Inversetti A. et al.’s [21] study findings that children with spinal dysraphism who did not have complications had scores within the normal range. Also, it has been often mentioned that neurodevelopmental impairment was more likely in shunted children who developed shunt-related complications. [22] . However, when corrected for confounding factors such as central nervous system (CNS) infection or intracranial hemorrhage, test scores for shunted and non-shunted children were similar [23] [24] . Thus, there is little evidence to suggest that mild to moderate ventricular enlargement is detrimental to neurocognitive outcome; by contrast, shunt-related complications, such as infection or repeated blockage, are more likely to negatively impact long-term outcome.
As a result of the neurological and medical symptoms of spinal dysraphism, they are at increased risk of neurobehavioral difficulties. In this study, we found that out of 84 patients, 27 (32.1%) did not talk like other toddlers their age; 21 (25%), their parents did not understand what they said; 57 (67.9%) of children didn’t walk, run, or climb like other toddlers; 3 (3.6%) had concern about vision; 42 (50%) had medical problems; and 12 (14.3%) had concern about child behavior. This is consistent with Nagaraj UD et al.’s [25] study, which recorded that even with adapted living arrangements, only half of the patients have an IQ above 80, and many have major learning impairments. Only half of the patients are able to live freely as adults [26] . This may have been interpreted by Jacobs R. et al.’s [27] study findings, which concluded that children with myelomeningocele often experience neurological deficits, including incontinence and motor difficulties, with specific deficits related to the location of the lesion along the spinal cord. Sensory deficits have also been shown to affect both the formation of synaptic connections between neurons in the perinatal period and myelination throughout childhood. These neurologic deficits may interfere with the development of cognitive skills because the physical disabilities that these children experience may restrict their capacity to efficiently interact with the environment. Further, visual and auditory deficits may impact the child’s ability to process information efficiently for learning and acquiring new skills [28] .
Despite the growing recognition of spinal dysraphism as a potentially life-threatening abnormality in children, up to 15% of patients die by the age of 3 years, and nearly one-third of patients are left with permanent neurological disabilities. We assessed the neurological development of these patients, and unsurprisingly, according to ASQTM Scores 62 (73.8%), gross motor skills needed further assessment with a professional. Fine motor assessment showed that 39 (46.4%) of patients needed further assessment with a professional, Problem-solving assessment showed that 39 (46.4%) of patients need further assessment with professionals, and Personal social assessment showed that 57 (67.9%) of patients need further assessment with professionals. This is in line with Stevenson KL et al.’s findings that among MMC patients at age 2 years, motor function was statistically significantly impaired. A mean of 77.78 is considered to have a high clinical impact on relevant motor disabilities. When dividing motor function at the age of 2 years into fine and gross motor function, only gross motor function was impaired [29] . An explanation for more favorable fine motor function compared to gross motor function is that assessment of motor function at the age of 2 years focuses on gross motor milestones, while fine motor requirements are limited at this age and standardized tests are more thorough at an older age [30] . However, motor function was impaired compared to typically developing children, especially regarding gross motor function, leading to delayed ambulation.
6. Conclusions
The result showed a slight predominance of male to female ratio of 1.3:1, and the majority of patients’ mothers didn’t receive folate supplements. All patients underwent surgical repair, and over half of patients underwent a VP shunt. The most common postoperative complications were infection, followed by VP shunt revision.
Patients communication assessment showed that one third of patients needed Further assessment with professionals. The gross motor assessment showed the majority of patients needed further assessment with a professional, Fine motor assessment showed that nearly half of patients needed further assessment with a professional. Problem-solving assessment showed that nearly half of patients needed further assessment with a professional. Personal social assessment showed that the majority of patients needed further assessment by professionals.
Some patients had apparent problems hearing and talking like other toddlers their age; their parents did not understand what they said; they had other medical problems; they were concerned about child behavior; and the majority of them didn’t walk, run, or climb like other toddlers.
There was a statistically significant association between neurological development and age at repair, complications, and the type of surgery they underwent.
Recommendations
Work toward a prenatal diagnosis of spinal dysraphism and planning for a birth in a hospital that provides a high level of nursery care and a neurosurgical unit, thus improving opportunities for early repair.
One of the main factors that improve neurodevelopment is postsurgical rehab. We recommend including an orthopedist, urologist, and pediatrician who will check for bony and urinary deformities to start early management for those issues.
Parents and other caregivers are a key part of the team. They can learn how to help manage a child’s condition and how to encourage and support the child emotionally and socially.
Abbreviations
CMIIs Chiari Type II Malformations
CSF Cerebrospinal Fluid
CT Computed Tomographic
DQs Developmental Quotients
ETV Endoscopic Third Ventriculostomy
ICU Intensive Care Unit
ICP Intracranial Pressure
MMC Myelomeningocele
MRI Magnetic Resonance Imaging
NCNS National Center for Neurological Sciences
NPH Normal Pressure Hydrocephalus
QP Quiet Phase
RCT Randomized Controlled Trials
SBM Spina Bifida Meningomyelocele
SPSS Statistical Package for Social Science
VA Shunt Ventriculoatrial Shunt
VP Shunt Ventriculoperitoneal Shunt