Research on the influence of POP surgery on the sexual functioning shows conflicting results. Results range from improvement, [3,7-14] to unchanged, [15-17] and deterioration of sexual functioning postoperatively [3, 18-22].
Surgery is often considered successful when a significant anatomical improvement is reached. Patient satisfaction however, correlates strongly with self-described goals, such as the resumption of daily activities (40.2%) and symptom reduction (38.1%) [23]. So symptom reduction, including sexual dysfunctioning, is an important outcome measure for patients.
Aims
Our study will focus on sexual activity in women with POP and the assessment of different domains of sexual functioning after POP surgery. Secondary outcomes are quality of life and anatomical results. To this end, we carried out a prospective study, with a follow-up time of 2 months.
2. METHODS
A prospective study was carried out between January 2012 and October 2012 in Deventer Hospital, Deventer, The Netherlands. Deventer Hospital is a secondary-level teaching hospital. Oral and written informed consent was obtained from all participants.
Women with POP scheduled for surgical correction, were eligible for participation. Sexual activity was assessed in all women. Concerning the influence of POP surgery, we included women who where sexually active, defined as have had coitus in the month prior to surgery. Women who where not sexually active due to POP were also included. Sexually inactive women, due to other than POP related causes, were excluded. Other exclusion criteria were concomitant incontinence surgery, postoperative use of local estrogens and inadequate composure of the Dutch language. All patients were gynaecologically examined before and 6 weeks after surgery and POP staging was performed using the Baden and Walker classification system.
The primary outcome measure was sexual functioning, divided into different domains. To this end we used the Leiden Questionnaire (LQ), a validated Dutch questionnaire [24]. The LQ comprises ten questions concerning sexual functioning, addressing sexual activity, frequency of sexual contact, sexual desire, lubrication, orgasm during intercourse and masturbation, dyspareunia and sexual satisfaction. Answers are according to a 5-point Likert scale, ranging from never to always. The higher the score, the higher the degree of dysfunction. Patients completed the LQ prior to and 2 months postoperatively.
The secondary outcome quality of life was assessed using the SF-36 questionnaire. Anatomical results were analysed comparing preand postoperative POP grading.
Power analysis was not possible, because the LQ was never used for this research question and because of contradicting results in the existing literature so far. For this pilot study we expected a response rate of 50%.
IBM SPSS Statistics 19.0 (Chicago, Illinois, USA) was used for statistical analysis. The Shapiro-Wilk test was used to assess whether the variables were normally distributed, using a statistics W-value of ≥0.9 as a cut-off point. The LQ was recoded into a uniform five-point Likert scale. Data were analysed using the non-parametric Wilcoxon signed rank test. If no significant difference was found, a post hoc power analysis was performed using G*power 3.1. Given the high percentage of excluded and declining patients, baseline characteristics of these groups were compared with the patients included. We used the Mann-Whitney U-test for data with a skewed distribution and the Fishers exact test and the Chi-square for the categorical, binary variables. A p-value of <0.05 was considered significant.
3. RESULTS
74 patients (average age 61.5 years) were approached. Preoperatively 25 out of 74 patients (33.8%) were sexually inactive due to other reasons than POP. Two patients were not sexually active due to POP. Table 1 shows sexual activity of all patients and the reason for being sexually inactive, when known. 39 patients were found eligible for further analysis. Thereof 16 patients declined participation. 23 patients (average age 56.7 years) were included. Details are shown in Figure 1.
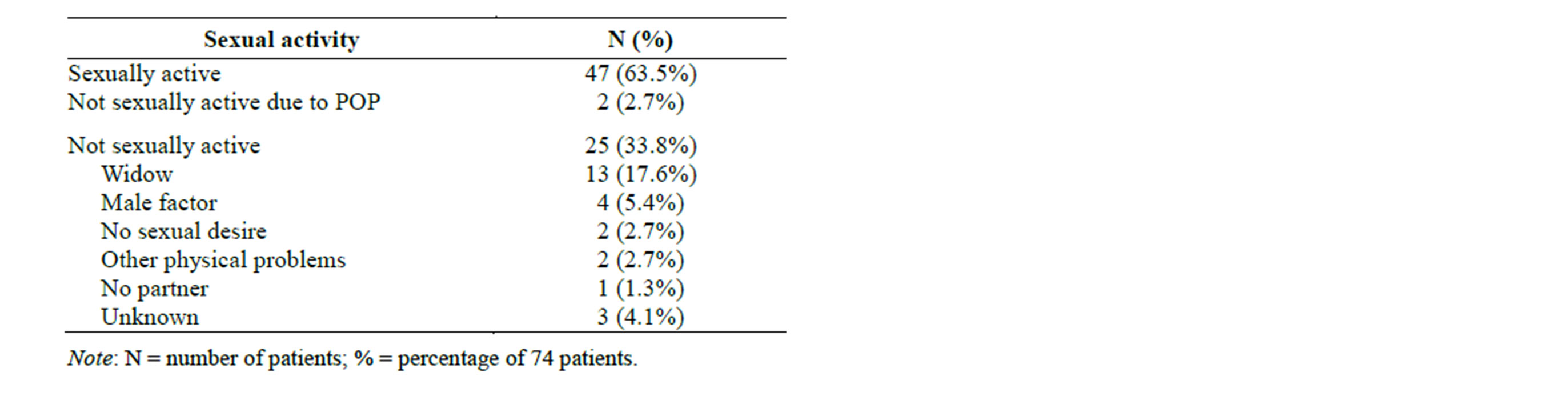
Table 1. Sexual activity preoperative.
The patient characteristics are shown in Table 2. The average age was 56.7 ± 8.4 years. Four patients had already undergone a hysterectomy, one in the context of POP. The latter was also the only patient with a recurrence POP. The average follow-up time was 10.3 ± 1.9 weeks (range 8.0 - 15.1 weeks).
Table 3 shows the different surgical procedures carried out. Most patients underwent a combination of procedures. There were five complications postoperatively: one hematoma on the posterior wall, two urinary tract infections and one postoperative bleeding, for which surgical exploration in theatre. One patient suffered from severe, possibly neuropathic pains at the side of operation.
Postoperatively there was a significant improvement (p = 0.008) of orgasm during intercourse. No significant differences were found for the other domains, as stated in Table 4. Post hoc power analysis showed a power of <0.8. Table 5 shows trends postoperatively. Two preoperative sexually active patients were not sexually active at follow-up. In one patient this was related to severe, possibly neuropathic pains. In the second patient it was related to pain due to the sutures and increased vaginal discharge. The two patients who were not sexually active preoperatively, were both sexually active postoperative. Five patients (21.7%) denoted a deterioration of dyspareunia, of which 3 patients had de novo dyspareunia.
As for quality of life, a significant improvement (p = 0.035) was seen on the domain “changes in health” and a significant deterioration (p = 0.012) was seen on the domain “physical role functioning”. The total score and the other domains didn’t show significant differences. Looking at trends 17 patients (73.9%) showed an improvement in the total score. The Wilcoxon signed rank test showed a significant improvement of cystocele (p ≤ 0.001), rectocele (p = 0.005) and descensus uteri (p ≤ 0.001).
Comparing the excluded and declining patients with the patients included, no significant differences were found in POP grading and surgical procedures carried out. The patients included were significantly more often sexually active (p ≤ 0.001), had a partner more often (p ≤ 0.001) and were younger (p = 0.02). As for post-
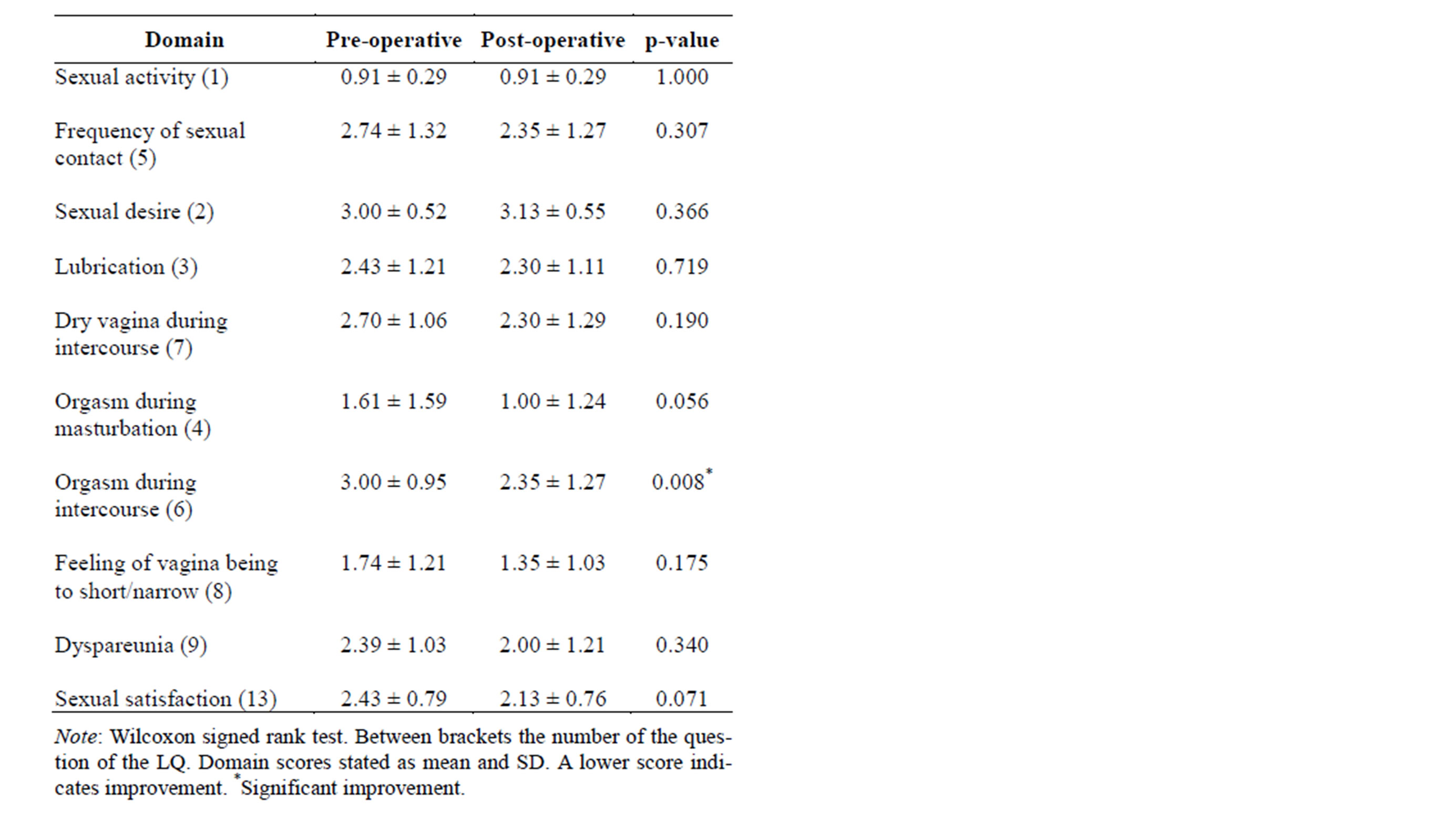
Table 4. LQ scores preoperative and two months postoperative.
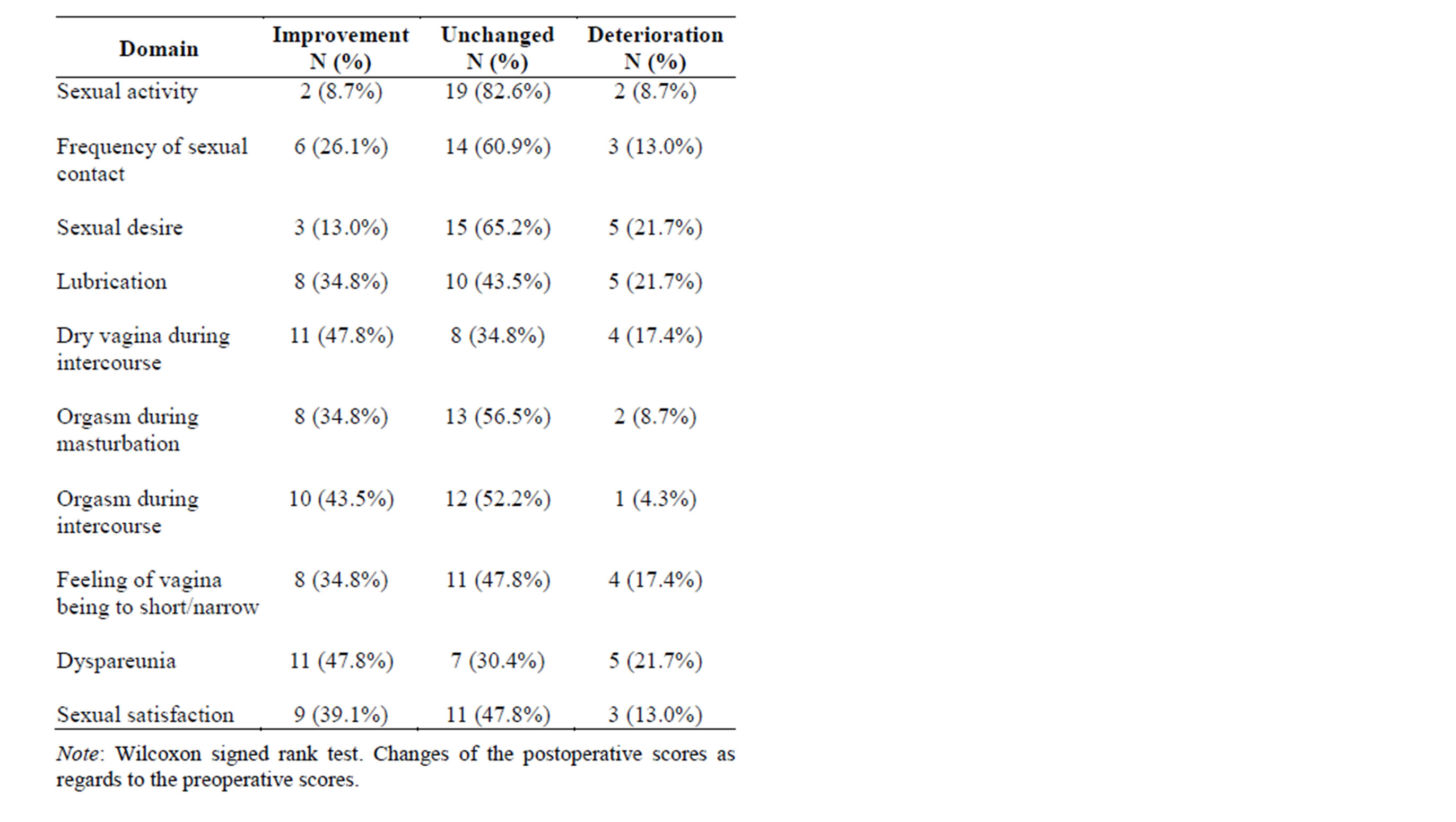
Table 5. Trends. Changes in domains of sexual functioning.
menopausal status, BMI, parity and recurrence POP surgery there were no significant differences.
4. DISCUSSION
4.1. Main Findings
The most important finding of our study is that over a third of the patients presenting with POP are not sexually active due to other reasons than POP. Since similar studies haven’t taken excluded patients into account, little is known about sexual activity in general in this particular group. One study supports our finding; they found that 38.4% of women with pelvic floor disorders were not sexually active [25]. Our finding can partly be explained by the fact that over half of the sexually inactive women were widows. Although part of them had a new partner, they didn’t have coitus. Probably sexual activity in this age group is less focused on coitus and more on other types of sexual activity and intimacy.
As for the effect of POP surgery on sexual functioning, it didn’t affect sexual activity in the majority of patients who were sexually active preoperatively. This is supported by three other studies [3,16,18]. On follow-up two patients were not sexually active. In one patient it was related to pain due to the sutures and increased vaginal discharge, so it is to be expected that she will get sexually active again in the long-term after disappearing of these complaints. For the other patient it was related to severe, possibly neuropathic pains. The two patients who were not sexually active preoperatively, were both sexually active at follow-up. This fact is also underexposed in literature. Only one study showed that 21% of preoperatively sexually inactive patients, resumed sexual activity postoperative. However, the reasons for being sexually inactive are not stated [3]. All other studies excluded women who were sexually inactive, even when this was related to POP.
The significant improvement that we found on the orgasm during intercourse is not endorsed by other studies, that showed no significant difference, [3,7,15-17] or deterioration [9]. There is no clear explanation for this improvement. Looking at trends, the largest improvement was seen in dyspareunia, in nearly half of the patients. Research so far shows miscellaneous results. Six studies support our finding [3,7,10,11,13,14], however, several studies found deterioration [8,19-22]. The latter was particularly associated with implant surgery in the first three months postoperatively. Lubrication, although unchanged in about half of the patients, improved in over a third. This finding is confirmed by a number of studies [3, 7,10,13,14]. However in four studies that showed improvement in both dyspareunia and lubrication, patients were prescribed local estrogens postoperatively, which may have a positive impact on both domains [7,10,13,14]. Three patients had de novo dyspareunia and five patients decreased lubrication. There are several explanations possible. Vaginal nerve innervation and vascularization play an important role in lubrication, by increasing the vaginal blood flow. Theoretically dissection of the vaginal wall may cause damage to the vaginal neurovascularization. There is also a chance of narrowing the supporting tissue surrounding the vagina too much, both proximal and distal [26,27]. Finally vaginal surgery can lead to scarring and loss of elasticity of the vaginal wall. A combination of these factors, individually or together, may play a role in decrease in lubrication and increase dyspareunia.
Preoperatively POP is associated with problems regarding lubrication, dyspareunia and satisfaction [3-5]. Post hoc power analysis revealed that to have enough power (≥0.8), 46 patients are needed to evaluate sexual satisfaction, 181 for dyspareunia and 832 for lubrication.
4.2. Secondary Outcome Measures
Our quality of life analysis showed a significant improvement on the domain health change and a significant deterioration on the domain role functioning physical due to health problems. The latter focuses on limitations in work or daily activities. This deterioration can be explained by the short follow-up. The total score and the other domains didn’t change significantly, although 73.9% of patients had an improvement in the total score. One patient with severe postoperative pain scored very low on all domains (total score 19.61), which is ≥2.5 SD below the group average. In view of the small study population, it was thought that this outlier affected the scores of the entire group. This was confirmed when repeating the Wilcoxon signed rank test, omitting this patient. A significant improvement was found on the total score (p = 0.049), vitality (p = 0.025) and health change (p < 0.01). In all probability we can expect a significant improvement in quality of life with a larger study population, which would be supported by previous research [8,19]. As expected we found a significant improvement in cystocele (p ≤ 0.001), rectocele (p = 0.005) and descensus uteri (p ≤ 0.001).
4.3. Inand Exclusions
As described under main findings, we excluded over a third of the patients because they were not sexually active, due to other reasons than POP. This finding was higher than expected since little is know about sexual activity. Over 20% of patients declined participation, of whom most found the subject of our study to burdened. Possibly there are more sexual problems in this specific group. This and the fact that two-thirds of women were sexually active, underlines the importance of this study.
4.4. Strengths and Limitations
Our study has several strengths. Our study population consisted of patients who solely underwent POP surgery, excluding patients with concomitant urinary-incontinence surgery [3,8,9,11,15,16,18,19,21,22]. We also excluded the possible bias of postoperative local estrogencreme [7,10,13,14]. To our knowledge this is the first study that took excluded patients into account and the specific reasons for being sexually inactive. In addition, we have taken patients who were not sexually active due to POP into analysis. For this group in particular it’s interesting to know the influence of POP surgery on sexual functioning. Finally, our study had a high follow-up percentage (23 of 26 patients, 88.5%), compared to the 50% - 76% in other studies [3,9,11,21,28].
Limitations of our study include the relative small study population, making it difficult to reach enough power to demonstrate significant differences. External factors, other than POP, might influence sexual functioning. Since we used a paired analysis, with every patient forming her own control, the role of external factors is expected to be low. With a short-term follow-up, we may assume the external factors to be equal preand postoperative in the majority of cases. Other limitations were lack of long-term follow-up and inclusion of different types of operations. Although we used a validated Dutch questionnaire, a recent study showed that the PISQ-IR is a validated and specific questionnaire to measure sexual function in women with pelvic floor disorders. [29] At the time of the design of our study, this study was not yet published.
4.5. Interpretation
Since post hoc power analysis showed that there was insufficient power to achieve statistic significance, a larger study is necessary before reliable conclusions can be drawn. However, for the outcome measure lubrication over 800 patients are needed.
5. CONCLUSION
More than a third of patients presenting with POP are not sexually active due to other reasons than POP. Our results show that POP surgery is successful with regard to anatomical correction. Concerning sexual function, surgery appears to improve lubrication, dyspareunia, sexual satisfaction and orgasm during intercourse in a considerable part of patients. Furthermore, there is no negative influence on sexual activity in women who were sexually active preoperatively. It even appears to improve sexual activity in women not sexually active preoperatively due to POP. POP surgery improves quality of life in the majority of patients.
ETHICAL APROVAL
According to the Central Committee Human Bound Research (CCMO), no ethical approval is needed for research involving questionnaires. www.ccmo.nl.
FUNDING
Source of finance: none.