Does the incubator control mode influence outcomes of low-birth-weight neonates during the first days of life and at hospital discharge? ()
1. BACKGROUND
Adults are able to maintain a constant core body temperature over a wide range of ambient thermal conditions. In contrast, the newborn infant can only achieve homeothermia over a much narrower range of ambient conditions. The preterm infant has even greater difficulty in maintaining core temperature as their thermal capability is exponentially correlated with gestational age [1]. During the first days of life, management of the thermal environment requires close attention in preterm infants who are particularly prone to both hyperand hypothermia. The range of ambient temperatures, which an immature infant can maintain body temperature, with minimal energy expenditure, is very narrow (36.5˚C - 37.5˚C). As a result, maintaining the core body temperature by controlling the environmental temperature is an essential for survival and optimum body growth as well as for various physiological functions [2]. The optimal ambient temperature at which the infant should be nursed is defined as “the range of environmental temperature within which the metabolic rate is at a minimum and within which temperature regulation is achieved by non-evaporative physical processes alone”.
Neonatal incubators currently use two types of temperature control, air temperature control (ATC) and skin servocontrol modes (SSC). SSC mode is designed to maintain the neonate’s abdominal skin temperature constant, whereas the ATC mode is based on the control of the circulating incubator air temperature (Ta). Abdominal skin temperature is used as an input signal since this parameter is assumed to be closely related to metabolic heat production. These 2 types of control modes produce different patterns of incubator air and infant body temperatures [3]. ATC seems to provide a more stable environment than SSC does [4] for thermal instability is due to repeated changes in infant skin temperature which result in repeated heating demands due to the error signal proportional to skin temperature changes. Heim [5] reported that the metabolic heat production of a 7 dayold-premature neonate (body mass 780 g, gestational age 27 weeks) did not reach a steady state level, but body temperature oscillated following the incubator air temperature. An increase in energy metabolism of 42% over minimal values was found, whereas with a control of air temperature at 34˚C, these fluctuations only reached 18%. Unfortunately, the effect of this difference in metabolism on body growth was not reported by these authors. Taking into account these observations, it is generally reported that the SSC mode should be used when the thermoregulatory system of neonates is fully efficient, but this remains to be proven in low-birth-weight infants.
It is well-known that the temperature management also influences infant outcomes [6], however, only a few studies have aimed to compare the impact of the 2 types of incubator control mode on these outcomes. Sinclair, in a meta-analysis [7] of two trials [8,9] used fatal events as an outcome (death, death by postnatal age period, death by birth weight group) and axillary temperature, as the only physiological parameter, pointed out that there was a very large decrease in death rate of low-birth-weight infants when using an incubator controlled from abdominal skin temperature kept at 36.0˚C while no adverse biologic consequences of thermal stability were found. To the best of our knowledge, no other studies dealing with this problem are available in the literature. Thus, the purpose of the present study was to assess the effects of incubator control mode on clinical outcomes over the first days of life and at hospital discharge for low-birth-weight infants.
2. PATIENTS AND METHODS
Before the investigation, the study was approved by the local ethics committee and all parents provided written informed consent. All the neonates were studied in the neonatal intensive care unit (NICU) at Centre Hospitalier Universitaire Nord in Amiens (France) and nursed for 10 days in a closed incubator Satis + (Médipréma, France). Infants were eligible if they had been born within the past 12 hours, before 33 weeks of gestation and with an Apgar score of at least 5 at 10 min. Infants were excluded if they had a major congenital abnormality and if they had to leave the NICU before the end of the study period. 52 neonates out of 56 recruited fulfilled these criteria. All infants were randomly assigned to one of the 2 incubator control modes: the SSC-group (n = 29) and the ATC-group (n = 23). All the neonates were nursed supine in incubator. The SSC mode was set to reach and maintain an abdominal skin temperature (Tabdo) of 36.8˚C as recommended by the WHO [10]. The thermistor probe was taped between the xiphoïd process and the umbilicus. The incubator air temperature in the ATC-group was determined using PRETHERM® software [11] which is not integrated in the incubator. PRETHERM® allows the calculation of incubator air temperature (Ta) by taking into account the neonate’s characteristics and the thermal insulation of any clothing. It was designed so that the value of incubator air temperature was calculated in order that the metabolic heat production defined by Chessex et al. [12] was minimal. Once calculated each day by the software, Ta was set by the medical staff once daily. Ta, Tabdo and the relative air humidity (RH) inside the incubator were recorded every second during the 10 days using PT 1000 probes for all temperatures (accuracy: ±0.3˚C) and a capacitive humidity sensor for relative air humidity (accuracy: ±10%). The temperature in the room was kept around 25˚C (relative air humidity 35% - 50%; air velocity lower than 0.2 m/s). From the first day of life (noted D0) to the 10th day of life (last day of the study, D9), the neonate’s weight and caregiving (energy intake, respiratory assistance and drug administration) were scored to describe the neonate’s health status. At hospital discharge, we recorded the duration of hospitalization, the prevalence of bronchopulmonary dysplasia, the use of steroids and the occurrence of intra-ventricular hemorrhage. All these clinical outcomes were documented daily in patient medical records.
3. STATISTICAL ANALYSIS
Statview 5.0 software (SAS Institute Inc., USA) was used for the statistical analysis. The anthropomorphic characteristics and the daily outcomes were compared between the two groups using a parametric ANOVA analysis (F-values and the degree of freedom are indicated). When data were expressed as proportions, we used a chi-square test (χ2-values and the degree of freedom are indicated). Data were expressed as mean ± 1 SD. The significance was set at 0.05.
4. RESULTS
4.1. Anthropomorphic Characteristics
In the SSC-group, the neonates were 29.4 ± 1.4 weeks of gestational age, weighted 1217 ± 347 g at birth, their head circumference was 26.4 ± 2.2 cm and their height at birth was 36.7 ± 3.3 cm, their Apgar score at 5 min was 9 ± 2, 79% of them were appropriated-for-gestational age and 66% were male. In the ATC-group, the neonates were 29.9 ± 1.2 weeks of gestational age, weighted 1263 ± 292 g at birth, their head circumference was 27.0 ± 1.6 cm and their height at birth was 37.6 ± 2.7 cm, their Apgar score at 5 min was 9 ± 1, 78% of them were appropriated-for-gestational age and 39% were male. Table 1 shows that none of the anthropomorphic characteristics were statistically different between the two groups of neonates.
4.2. Thermal Environment
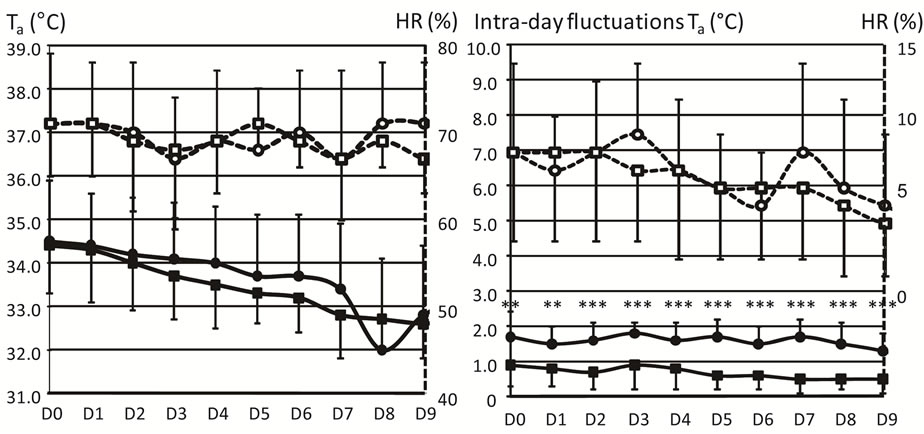
From D0 to D9, Figure 1 shows that the daily mean values of Ta and HR (in the left panel), as well as the intra-day fluctuations of HR (in the right panel), did not differ between the 2 groups of neonates. In contrast, intra-day fluctuations of Ta (in the right panel) were significantly lower in the ATC-group (range between 1.3˚C and 1.7˚C) than in the SSC-group (0.5˚C - 0.9˚C).
4.3. Abdominal Skin Temperature
Figure 2 shows that Tabdo was significantly higher in the ATC-group (37.0˚C) than in the SSC-group (36.7˚C) at D0, D4, D5, D6, D7, D8 and D9. Intra-day fluctua tions of Tabdo were also statistically higher in the ATCgroup (range between 0.4˚C and 0.5˚C) than in the SSCgroup (0.2˚C to 0.3˚C).
4.4. Caregiving
Daily energy intakes were comparable between the SSCand the ATC-groups from D0 to D9. Neonates received 81 ± 12 kcal·kg−1·j−1 on average in the SSC-group and 85 ± 12 kcal·kg−1·j−1 in the ATC-group (F1,46 = 1.081, p = 0.304). However, the daily energy intake increased slightly from D0 (29 ± 8 kcal·kg−1·j−1 in the SSC-group and 29 ± 10 kcal·kg−1·j−1 in the ATC-group, F1,46 = 0.001, p = 0.972) to D9 (109 ± 24 kcal·kg−1·j−1 in the SSCgroup and 113 ± 22 kcal·kg−1·j−1 in the ATC-group, F1,46 = 0.434, p = 0.513).
Daily fluid intake did not differ statistically between the SSCand the ATC-groups from D0 to D7. Neonates received 112 ± 32 ml·kg−1·j−1 on average in the SSCgroup and 111 ± 25 ml·kg−1·j−1 in the ATC-group (F1,46 = 0.004, p = 0.952). However, the daily energy intake was significantly higher at D8 in the SSC-group (190 ± 35 ml·kg−1·j−1) compared to in the ATC-group (168 ± 29 ml·kg−1·j−1, F1,46 = 5.035, p = 0.030) and at D9 (186 ± 21 ml·kg−1·j−1 in the SSC-group and 170 ± 33
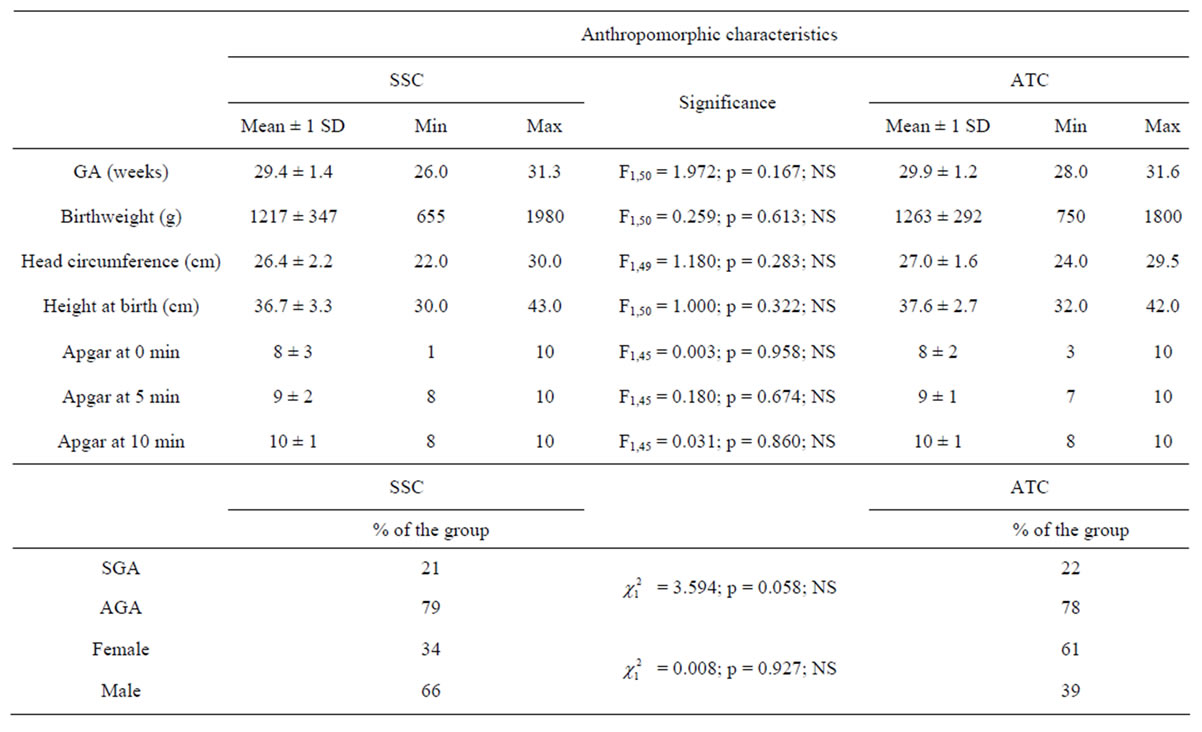
Table 1. Anthropomorphic characteristics of the neonates divided into skin servocontrol-group (SSC) and air temperature control-group (ATC). Gestational age (GA, weeks), birthweight (g), head circumference (cm), height at birth (cm) and the Apgar scores at 0, 5 and 10 min of life are expressed as means (±1 SD), minimal and maximal values. Percentages quantify the number of Small-for-Gestational Age (SGA), Appropriate-for-Gestational Age (AGA), female and male neonates in each group. The middle column shows the statistical tests to compare the 2 groups of infants. NS = Not Significant.
 (a) (b)
(a) (b)
Figure 1. Thermal environment. The preterm infants were divided into the skin servocontrol-group (SSC, circles) and the air temperature control-group (ATC, squares). Daily values (mean ± 1 SD) of incubator air temperatures (Ta, ˚C, solid lines and closed symbols) and relative air humidity (HR, %, dashed lines and open symbols) are represented on the left side of the figure. Intra-day fluctuations of Ta (˚C, full lines and symbols) and relative air humidity (HR, %, hatched lines and empty symbols) are represented on the right side of the figure. All the values are represented from the first day of life (D0) to the last day (D9) of the study. Values are mean ± 1 SD. **p < 0.01, ***p < 0.001.
 (a) (b)
(a) (b)
Figure 2. Abdominal skin temperature. The infants are divided into: skin servocontrol-group (SSC, ) and air temperature control-group (ATC,
) and air temperature control-group (ATC, ). Daily values of abdominal skin temperature (Tabdo, ˚C) are represented in the left panel and intra-day fluctuations are represented on the right side of the figure. All the values are represented from the first day of life (D0) to the last day (D9) of the study. Values are mean ± 1 SD. *p < 0.05, **p < 0.01, ***p < 0.001.
). Daily values of abdominal skin temperature (Tabdo, ˚C) are represented in the left panel and intra-day fluctuations are represented on the right side of the figure. All the values are represented from the first day of life (D0) to the last day (D9) of the study. Values are mean ± 1 SD. *p < 0.05, **p < 0.01, ***p < 0.001.
kcal·kg−1·j−1 in the ATC-group, F1,46 = 4.161, p = 0.047).
Table 2 shows that the number of days with oxygen assistance or artificial ventilation as well as the percentages of neonates under oxygen assistance or artificial ventilation or treated with cardioactive drugs at D6 and D9 were not different between the 2 groups. It should noted that caffeine was administered more frequently in the ATC-group than in the SSC-group at D9 ( = 4.205, p = 0.041).
= 4.205, p = 0.041).