Socio-Demographic Factors, Clinical Characteristics and Maternal Prognosis of Hypertensive Disorders in Pregnancy at Panzi General Referral Hospital ()
1. Introduction
Hypertensive diseases of pregnancy are among the leading causes of severe maternal morbidity and mortality, particularly in developing countries [1] .
An American College of Obstetricians and Gynaecologists (2013) was defined 4 groups of hypertensive diseases of pregnancy: Chronic hypertension, Gestational hypertension, preeclampsia and Chronic hypertension with Superimposed preeclampsia
They are accompanied by various feto-maternal complications, among the maternal complications are eclampsia, HELLP (hemolysis elevated liver enzymes low plaquets) syndrome, retro placental haematoma, stroke, disseminated intravascular coagulation, pulmonary oedema and acute respiratory distress syndrome, acute renal failure, and in extreme cases death [2] , a high frequency of post-partum haemorrhage has also been noted [3] . Fetal complications can include growth retardation in utero, prematurity, hypotrophy and even death in utero. In the long term, women with hypertensive diseases during pregnancy have a higher risk of chronic hypertension, diabetes mellitus, chronic renal failure, stroke, and coronary heart disease, chronic lung disease, retinopathy, Mental retardation, cerebral dysfunction, adult pathologies [4] . The occurrence of maternal complications in women with hypertensive diseases in pregnancy depends essentially on the age of the mother, her race, and the presence of pre-existing pathologies. The overall mortality of hypertensive disease in pregnancy is estimated to be around 7 per 1,000,000 cases and the risk of developing hypertension afterwards is around 20% in the following 7 years. [5] . The occurrence of fetal complications is essentially linked to the gestational age at the time of the onset of the pathology, the earlier the onset, the more severe the complications.
The pathophysiology of these pathologies is only partially elucidated and is thought to be the result of a defect in an invasion of the spiral arteries by the trophoblast, precisely the extra-villous cytotrophoblast, responsible for a defect in placental perfusion. This placental insufficiency leads to the release of cytokines and free radicals which triggers systemic oxidative stress, the maternal response manifesting itself in the second trimester as an inflammatory syndrome and diffuse endothelial dysfunction, responsible for the arterial hypertension and proteinuria characteristic of these conditions. [6]
Placental dysfunction is responsible for the fetal and neonatal morbidity associated with the condition and is often accompanied by prematurity induced by the need for early induction of labour, which is the only ‘treatment’ for the condition.
The problem of hypertensive disease in pregnancy is becoming even more important globally, with the prevalence of pre-eclampsia being significantly higher in Africa, where it averages 4% in the general population, but can be as high as 18% in some ethnic groups [7] . Worldwide, 76,000 women and 500,000 newborns die each year from this hypertensive disorder during pregnancy; moreover, women in low-resource countries are at greater risk of developing pre-eclampsia than those in high-resource countries [8] . In developed countries eclampsia is a rare event, occurring in two to three cases per 10,000 births, but still responsible for significant maternal mortality [9] .
In Africa and Asia, about 10% of maternal deaths are associated with hypertensive disorders of pregnancy, while they are responsible for about 25% of maternal deaths in Latin America. [10] Its prevalence in France is about 2% to 3%, stable between 2010 and 2016, but a third of these cases was a severe form responsible for 58% of hospitalizations in all maternity [11] . In France, the report on maternal mortality between 1999 and 2001 recorded 16 deaths related to hypertensive diseases, which represented the second most common cause of maternal death (11.3%). Eight of these were attributed to eclampsia and more than 40% were considered preventable [12] , thus hypertensive disease in pregnancy is a very important factor in maternal and fetal morbidity.
In the Democratic Republic of Congo, in a descriptive and multicentre study carried out in 3 large maternity hospitals in the city of Kinshasa between 2003 and 2007, a total of 17,592 pregnant women were studied, of whom 1492 (8.5%) presented with pre-eclampsia and 319 (1.8%) with eclampsia.
In our environment, the prevalence of this pathology is increasing, the purpose of our study is to determine the socio-demographic factors and the maternal prognosis of these women with hypertension during pregnancy, hence the purpose of our study.
2. Materials and Method
2.1. Study Setting
This study was carried out at Panzi Hospital, which is a referral health facility in the Ibanda health zone that serves 17 health areas with an estimated population of 515,834 inhabitants. It is also a university training clinic where general practitioners, obstetricians and midwives are trained.
2.2. Study Design
We conducted a cross-sectional study with an analytical focus from 1 January 2021 to 30 June 2022.
2.3. Study Population
Our sample was comprehensive, consisting of 114 pregnant women, parturient with high blood pressure during pregnancy and postpartum women diagnosed with high blood pressure before the sixth week and women transferred to us for high blood pressure in the postpartum period.
2.4. Inclusion Criteria
All pregnant women, parturient and deliveries who were diagnosed with hypertensive disease during pregnancy and who voluntarily consented to the study.
We considered hypertensive disease to be any episode of hypertension characterised by: Persistent arterial hypertension (AH) (diastolic blood pressure ≥ 90 mmHg) and systolic blood pressure ≥ 140 mmHg and significant urine dipstick proteinuria or not.
According to the number of crosses, a proteinuria was qualified as mild if no proteinuria or only one cross, moderate if two crosses and severe if three crosses and more than three crosses on the urine dipstick reading (Figure 1).
2.5. Exclusion Criteria
All pregnant women, parturients and deliveries without a diagnosis of hypertensive disease and patients who did not voluntarily consent to the study.
Data Collection, A survey questionnaire was submitted to each patient and an answer to the interview between the patient and the midwifery or an obstetrician student after verification of data, we completed in the database in Excel software before analysis (Described in the annex).
The data was taken on admission or within 48 hours of delivery or late abortion, and proteinuria was determined by qualitative analysis based on the number of crosses in the urine dipstick.
We analysed the different variables to arrive at the results, two types of variables were analysed.
1) The dependent variable:
Socio-demographic characteristics (Age, Marital status, Type of residence, Occupation Body mass index).
2) The independent variables:
History (Parity, type of pregnancy, prenatal consultation, preventive with low
aspirin, pre-eclampsia, diabetes, high blood pressure and fetal death in utero) clinical variables (reason for consultation, gestational age, blood pressure), and maternal prognosis (type of hypertension in pregnancy, route of delivery, maternal complications).
2.6. Data Entry and Analysis
We did the simple text entry with Microsoft Office Word 2010 and the tables for analysis with Excel 2010. The data analysis was done with SPSS version 20.0 and Stata 14.0 The qualitative variables have been summarised by the Percentage and the quantitative variables will be summarised by Means and Standard Deviation. The associations of the variables were calculated by Pearson's chi-square test with a significance level set at a p-value < 0.05.
2.7. Ethical Considerations
Our research protocol was submitted to the university's ethics and licensing committee to conduct this study. Free and informed consent was obtained from the study participants prior to data collection, and any subject had the right to accept or refuse to participate in the study. Confidentiality and anonymity were guaranteed in this study.
3. Results
3.1. Socio-Demographic Parameters
According to the results presented in Table 1, the average age of the patients was 30.33 years, of which 70.2% were between 18 and 35 years old. Most of them were married (92.1%), 79.8% lived in urban areas and most of them were overweight (43%).
In Table 2, 92.1% of them were carriers of monofetal pregnancies, 36% were multiparous, 94.7% of them underwent prenatal consultation, 13.2% of them received low-dose aspirin for preventive purposes, 34.2% had a previous history of preeclampsia in pregnancy, 1.8% had diabetes, History of Fetal death in utero was previously reported in 7% of the patients and 14% were hypertensive.
3.2. Clinical Parameters
In Table 3, they came to the clinic with one or two complaints, 29.77% were referred by the surrounding health facilities or the prenatal consultation department for pregnancy monitoring with high blood pressure and 27.48% came themselves for low back pain, 44.7% had massive proteinuria on admission.
In Table 4: for systole, the mean was 164.28 mmHg with a minimum of 100 mmHg and maximum of 243 mmHg and for diastolic, the mean was 107.46 mmHg with minimum of 70 mmHg and maximum of 128 mmHg, regarding gestational age the mean was 34.43 ± 4.327 amenorrhea weeks with maximum age at 41 amenorrhea weeks and minimum age at 20 amenorrhea weeks.
![]()
Table 1. Socio-demographics characteristics.
![]()
Table 3. Reason for consultation and proteinuria.
3.3. Maternal Prognosis of Hypertension in Pregnancy
In Table 5, pre-eclampsia was the most frequent form of hypertension in pregnancy with 73.68% of cases and the one associated with a high frequency of severe forms of hypertension in pregnancy, i.e., 84.8% of severe forms (Chat 1).
The route of delivery for patients with high blood pressure during pregnancy was 53.4% vaginal delivery and 46.6% of deliveries were by caesarean section, of which 66.6% of the indications for vaginal delivery were specifically related to high blood pressure during pregnancy (Figure 2).
Regarding the types of maternal complications, eclampsia was the most frequent complication in our patients with 31.7% frequency, followed by help
![]()
Table 4. Blood pressure and gestational age.
![]()
Table 5. Type of hypertension in pregnancy according to severity.
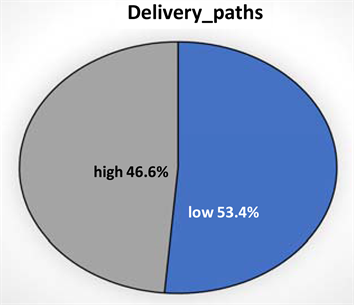
Chat 1. Route of delivery and indication for caesarean sections.
syndrome and acute renal failure with 26.82% and 19.50% respectively.
In Table 7, 28.9% of the patients who presented with maternal complications were between 18 and 35 years of age, age significantly influenced maternal
![]()
Table 7. Maternal age and maternal complications.
complications (p-value = 0.033) and with regard to body mass index, the patients who presented with maternal complications were in obese or overweight states with 40.4% and 43.0% respectively of frequency, body mass index significantly influenced maternal complications (p-value = 0.011).
4. Discussion
Gestational hypertensive disorders are a group of conditions whose cause is often not well defined and are the result of several risk factors that may influence the occurrence of these conditions.
A FIGO study led by Poon LC [8] identified some maternal risk factors for patients with hypertensive disease, including advanced maternal age, nulliparity, obesity, hyperglycaemia during pregnancy and pre-existing chronic hypertension.
Extreme age has been described as a risk factor, especially advanced maternal age and early maternal age, as well as being major risk factors for the occurrence of these conditions, our study found an average age of 30.33 ± 7.020 years, which shows that the maternal age in our study population was advanced, Although the presence of these risk factors is important in the occurrence of these diseases, the causality of the association between calcium and risk factors for hypertensive diseases during pregnancy remains to be investigated because of its multifactorial dimension.
In a meta-analysis of 48 studies in 20 countries involving 3,598,601 women, Mayri Sagady Leslie [13] concluded that pre-eclampsia was associated with a 3-fold increased risk of developing chronic hypertension compared with normotensive women, that women with pre-eclampsia had a double or even higher risk of cardiovascular disease, and that pre-eclampsia was also associated with approximately double the risk of fatal or non-fatal stroke. Laure Lyne Burdet et al. [14] Chronic hypertension may affect the physiological development of the uteroplacental circulation and is associated with an increased risk of placental ischaemic disease.
Pre-existing hypertension in pregnancy is a major risk factor for developing hypertensive disease in pregnancy, and a history of hypertensive disease in pregnancy is also a risk factor; in our study, 65.8% of patients had a history of pre-eclampsia in their previous pregnancy, but still a low rate of prevention with junior aspirin was observed, only 13.2% of our study population.
Obesity is a major risk factor for gestational hypertensive disease, Mayri Sagady Leslie [13] Excessive weight gain during pregnancy or pregnancy against a background of obesity and overweight, which is associated with hyperinsulinism, insulin resistance and maternal systemic inflammation proposed as one of the mechanisms leading to endothelial dysfunction associated with hypertension, proteinuria, thrombotic disease, multi-organ damage and high maternal mortality; The endothelial and vascular dysfunction associated with these disorders is responsible for the vasoconstriction characteristic of hypertensive disorders during pregnancy, taking into account our study 83.4% of our study population was either overweight or obese, but knowing the BMI of our patients before pregnancy could provide additional answers, as pregnancy is associated with weight gain that is often not negligible.
The quality of the antenatal care of patients with hypertension in pregnancy is one of the pillars of the management of this pathology, since good follow-up allows the early detection of fetomaternal complications on which the management depends; prevention with aspirin in antiplatelet doses remains an important means of prevention. In our study, we found a low rate of prophylaxis with aspirin 100 mg, i.e. 13.2% of our study population.
Regarding gestational age, our study showed that the mean age of delivery in hypertensive patients during pregnancy was 34.43amenorheas weeks.
In a study comparing the perinatal prognosis of hypertensive patients during pregnancy with that of normotensive pregnant women, Joëlle M. [15] found that pregnancies of hypertensive patients were more likely to be delivered preterm than those of normotensive women, with a more than 4-fold increased risk of delivery before 37 weeks’ gestation when a pregnant woman had hypertension during pregnancy (OR = 4.58 [1.57 - 13.36]). The authors also found a deficit in the overall biometric parameters. The blood pressure of our patients showed a tendency towards severity, the average systolic blood pressure was 164.28 mmHg and the average diastolic blood pressure was 107.46 mmHg, this tendency towards severity explains the tendency to induce preterm delivery, i.e. our average of 34.43 amenorhea weeks.
With regard to the maternal prognosis of patients with hypertension during pregnancy, we will evaluate the severity, mode of delivery and maternal complications.
Regarding the severity of hypertension during pregnancy, pre-eclampsia is the form of hypertension during pregnancy that represents the majority of severe forms of hypertension, with a frequency of 58.77% of the 69.3% of severe forms. In his study, Cissé C.T. et al. [16] found a frequency of pre-eclampsia of 14.9% of all hypertensive disorders associated with pregnancy.
Regarding the mode of delivery of patients with arterial hypertension, we found that 46.6% of patients delivered via the upper route with an incidence of 31.06% of indications exclusively related to arterial hypertension for either maternal or fetal prognosis. Our study shows that one in three patients with hypertension during pregnancy will deliver by caesarean section for an indication exclusively related to hypertension. Eclampsia is the most common maternal complication in our patients with a frequency of 31.7%.
An association analysis of maternal complications with maternal age in patients with hypertension during pregnancy showed that as maternal age decreased, patients tended to have more hypertension-related complications with (p-value = 0.033) at the 5% significance level. Regarding body mass index and maternal complications, the study found a significant association between increasing body mass index and maternal complications (p-value = 0.011) at the 5% significance level.
Collection Sheet
IDENTITY Bukavu, The............../............../2021
Surname............................
First name....................
Age......................
Type of residence: urban................semi-urban.............rural..................
Occupation 1 = no occupation; 2 = trader; 3 = student;
4 = civil servant (specify.............................................); 5 = other to specify..................................
Civil status .... 1 = married; 2 = single; 3 = divorced .........4= separated ............
- Weight ....... in kilograms
- Height ....... in centimetres
BMI:
HISTORY
Obstetric history
Body type ....... Parity .... Alive .... Abortion ... Died .....
DDR ....../......./....... PAD ....../......./....... Gestational age ...............
Pathology during pregnancy 1 = no; 2 = yes
(Please specify) .............................................................................................................................................
Place of residence during the first 4 months of pregnancy.........................................................
Personal medical history
- Known hypertension ... = yes; 2 = no
If yes, current treatment ...............................................................
...............................................................
- HTA during previous pregnancy ... = yes; 2 = no
If yes, current treatment ...............................................................
...............................................................
-Taking aspirin junior...... 1 = yes; 2 = no
If yes, from which month ...............................................................
- Diabetes ........ 1 = yes; 2 = no
-MFIU ........ 1 = yes; 2 = no
PREGNANCY FOLLOW-UP
- ANC .... 1 = yes; 2 = no
- Number of ANC ........ 1 = none; 2 = 1; 3 = 2; 4 = 3; 5 = 4
- Location ..............................; unknown= 2
Reason for consultation: Please specify ...........................................................................................................
Proteinuria (number of crosses) ....................................................................................................................
CLINICAL EXAMINATION
- State of consciousness ....... 1 = good; 2 = impaired
- BP BD ........... /........... / in mm hg
BLOOD PRESSURE ........... /........... / in mm hg
- Heart rate ........ bpm
- Presence of oedema ....... 1 = yes; 2 = no
- Type of hypertension in pregnancy................................................................
- Mode of delivery: 1. vaginal delivery........................2.vaginal_delivery...............
If vaginal delivery (2)
- Indication for caesarean section: .............................................................................................
Comment: ....................................................................................................................
- Types of complications to be reported: ..............................................................