Clinical, Psycho-Social and Metabolic Profile of Women with Hirsutism in Yaounde ()
1. Introduction
Hirsutism is defined as the excessive development of hair in areas where it is normally absent in women. These are androgen-dependent areas where male sexual maturity usually occurs, namely: the face, thorax, white line, lumbar region, gluteal and intergenitocrural regions [1].
It is a common clinical problem affecting approximately 5% to 10% of women of childbearing age according to epidemiological studies in Spain, the United States and Iran [1] [2] [3]. The prevalence of the different etiologies found varies according to the ethno-geographic area. This is most often the result of the action of androgens on the pilosebaceous unit. Hirsutism is also defined by a Ferriman and Gallwey score ≥ 6 - 8 [4]. This symptom is very often trivialized because it is considered more of a cosmetic problem than a medical one. This is probably due to the idiopathic and multi-organic concept of this symptom which makes etiological research difficult [5]. Beyond the genetic nature, hirsutism may be the cutaneous reflection of hyperandrogenism, the most common cause of which is polycystic ovary syndrome (PCOS) which is responsible for more than 70% of cases of hirsutism [6]. Hirsutism can have a significant psychosocial impact due to possible associated infertility and signs of virilization that can affect female identity [7]. Metabolic disorders have been described particularly in women with hirsutism in the context of PCOS due to insulin resistance [8]. While hirsutism is present in our population, no studies have been done. The aim of our study was to describe the clinical, psychosocial and metabolic profiles of women with hirsutism in Yaoundé.
2. Methodology
2.1. Type of Study
We conducted a descriptive cross-sectional study. It took place at the Yaoundé Central Hospital in the department of endocrinology and metabolic diseases over a period of 08 months, from May 2013 to December 2013. The women were recruited by announcement through social media.
Inclusion criteria: We included non-lactating and non-pregnant women aged at least 18 years with hirsutism regardless of the degree of severity who agreed to participate in the study.
Exclusion criteria: We excluded post-menopausal women with hirsutism.
Sampling was consecutive, exhaustive and non-probabilistic.
2.2. Procedure
We used a questionnaire that was pre-designed by the authors; its validity and reliability were tested with volunteers. It contained ten items including identification of participants, obstetrical and gynecological history, personal and family medical history, lifestyle and weight history, information on hirsutism, psycho-social impact related to hirsutism, clinical and biological data. The modified Ferriman and Gallwey (FG) score was used. We classified participants as follows: FG score less than 15 is mild hirsutism, between 16 and 24 is moderate hirsutism and greater than 24 is severe hirsutism. We measured fasting capillary blood glucose, and a blood sample was taken for the determination of total cholesterol, high density lipoprotein (HDL) and triglycerides by enzymatic endpoint colorimetric method. The concentration of low density lipoprotein (LDL) was calculated according to Friedewald’s formula. Psycho-social assessment was carried out using a pre-designed sheet focusing on the daily perception and experience of hirsutism. The metabolic profile of the participants was established according to the criteria of the International Diabetes Federation of 2005 (IDF-2005) and the National Cholesterol Education Program—third adult treatment panel of 2001 (NCEP-ATP III-2001).
2.3. Statistical Analysis
Data were processed into Epidata version 3.0 software and extracted into Stata version 10 software for analysis. The association between qualitative variables was measured by the chi-square test or by Fisher’s exact test when necessary. Comparisons between groups were made by the nonparametric tests of Man Whitney. The association between quantitative variables was measured by Spearman’s nonparametric correlation. The significance threshold was set at 5%.
2.4. Ethical Considerations
All participants gave their written informed consent. We received authorization N˚ 159L/MINSANTE/SG/DHCY/Stages from the ethics committee of the Yaoundé Central Hospital.
3. Results
3.1. Epidemiological Data
We recruited 60 women whose average age was 27.6 ± 7.0 years and 62% of participants were students. In the study, 41.7% of the women originated from the western region of Cameroon, followed by 33.3% and 10%from the center and littoral regions, respectively.
3.2. Clinical Aspects
The average age of onset of hirsutism was 17 years ± 4.2 years.
The Ferriman and Gallwey’s median score was 12 with 70% of women presenting mild hirsutism, 28.3% moderate hirsutism and 1.7% severe hirsutism. The most affected areas were the abdomen and chin, and the mean duration of progression of hirsutism was 9 years. A family history of hirsutism, especially in the mother, was found in 88.8% of participants. Associated signs found were seborrhea (83.3%), hypertrichosis (53.3%), acne (50%), acanthosis nigricans (20%) and signs of virilization (3.3%) (Table 1). Menstrual cycle abnormalities such as spaniomenorrhea were found in 16.7% of women and an association was found between menstrual cycle abnormalities and the severity of hirsutism (p = 0.023). (Figure 1).
Regarding obstetrical aspects, 55% of participants had never been pregnant compared to 45% of women who had been pregnant at least once. Among 33 participants who had never been pregnant, 31 did not have a desire for pregnancy and two women suffered from primary infertility.
With regards to hirsutism treatment 47 women or 78.3% used various treatments versus 13 women or 21.7% who did not use any treatment. The most common treatments used were hair removal and shaving at 66% and 51%, respectively. None of the participants had used electrolysis or laser. Two participants were put on medical treatment.
![]()
Table 1. Signs associated with hirsutism.
![]()
Figure 1. Association between severity of hirsutism and menstrual cycle abnormality.
3.2. Psychosocial Considerations
On the psychosocial level, 58.8% of women found hirsutism normal and 73.3% live with it fairly well. The participants’ perception of hirsutism was as follows: a “missed male” at 26%; beauty or seductive at 21%; witchcraft at 20%; wickedness at 14% and infertility at 18% (Table 2). There was no significant association between the perception of hirsutism, educational level and age.
3.3. Metabolic Aspects
Based on body mass index (BMI), obesity was found in 26.7% of participants The average abdominal circumference was 81.6 cm ± 11.5 cm. The metabolic syndrome was found in 21.7% and 18.3% of participants according to IDF-2005 and NCEPIII-2001, respectively (Table 3). Using Spearman’s non-parametric correlation, no significant correlation was found between the Ferriman and Gallway score, the anthropometric parameters and the metabolic syndrome.
4. Discussion
Hirsutism is present in the Cameroonian. However, not poorly elucidated due to lack of data. Our study provides information on the clinical, psychosocial and metabolic aspects. Our study population was young with an average age of 27.6 ± 7.3 years. Most had a university level of education. This is likely because this segment of the population could easily understand the value of carrying out a scientific study that was without personal profit and also required constraints such as blood draw. The majority of our participants came from the West, Center and Littoral regions probably because these are the regions with the highest population densities according to the third census of the Cameroonian population of 2010 [9]. Most women had mild hirsutism and only one woman
![]()
Table 2. Psychosocial considerations of participants.
![]()
Table 3. Metabolic profile of participants.
had severe hirsutism. This can be explained by our small sample size and the refusal of several women to participate in the study for various reasons (no personal interest, fear of blood tests, cultural context); however, the same observation was made in several studies including Sharma and al. in India [10] and Ansarin and al. in Iran [11] who each found mainly women with mild hirsutism. The mean score of FG was 12. The same figure was found in Sharma and al. in India and lower than that of Zargar and al. in Kashmir which found 13.5 [12]. On the other hand, Zhao and al. in China report a threshold value of 5 [13], likely because of ethno-geographic differences [8]. Regarding the most affected areas in our cohort, the lower abdomen, the chin and the upper abdomen with respective average scores of 2.6/4, 2/4 and 1.8/4. On the other hand, Sharma and al. in India [10] reported the chin, upper lip and lower abdomen as the most frequently affected areas. These findings are probably due to ethnic differences as pointed out by Carmina and al. [14]. However, the chin and lower abdomen remain the most affected areas in the literature [10] [15] such that Knochenhauer and al. concluded in their study that an FG score ≥ 2 in these regions was predictive of hirsutism with a sensitivity of 100% but especially in regions with a high prevalence of hirsutism [16]. The mean age of onset of hirsutism was 17 ± 4.2 years, which is the peri-pubertal age at which all the disorders linked to hyperandrogenism, such as acne and seborrhea are noted [17]. Regarding the associated signs, seborrhea and acne were the most common with 83.3% and 50%, respectively. Acne was found by Noorbala in Iran at 42.7% [3], by Sharma and al. in India at 73.7% [10], and by Zhao and al. in China at 44.4% [13]. Hypertrichosis represented 53.3% of our cohort compared to 42% in Noorbala in Iran [3]. We noted that two participants (3.3%) presented signs of virilization which would justify an etiological investigation. Acanthosis nigricans is commonly found in hyperandrogenic patients with insulin resistance in the context of HAIR-AN syndrome [17] [18]. Since we found 26.7% obese patients in our cohort, it would be wise to perform a hormonal profile of our participants to look for this syndrome. With regards to the obstetrical/gynecological aspects: we noticed that 16.7% of participants had menstrual irregularities. This is lower than that found by Sharma in India [10], Zhao in China [13] and Azziz in the USA [19], who found 22.8%, 23.2% and 28%, respectively. However, our percentage is higher than that of Noorbala in Iran, which was 14.6% [3]. Nevertheless, this non-negligible number would justify performing a pelvic ultrasound and even hormonal assessment for PCOS research, which is the most common etiology of hirsutism in Saudi Arabia [20], Mexico [21], the United Arab Emirates [8] and Iran [3]. Regarding the management of hirsutism: the most of participants had recourse to esthetic treatments, especially, hair removal, because it was practical and financially feasible. No woman had used electrolysis or laser due to the absence of these modalities in Cameroon, although it is recognized that these produce better results in terms of tolerance and effectiveness on hair regrowth, since we note that 34% of the participants were not satisfied with their treatment [22] [23].
In our study, being hirsute seemed normal to most participants. This is probably because of the family history found in most of them, which suggests a genetic component. This acceptance of hirsutism can also be due to the relatively long duration for its establishment (9 years), during which the participants would have adapted to the changes, and also the fact that 21% of consider being hirsute a seductive tool.
Metabolic syndrome was found in 21.7% and 18.3% according to the IDF-2005 NCEPIII-2001, respectively. In our study, the metabolic syndrome may be due to either the presence of Polycystic Ovarian Syndrome (PCOS), since this duo has been found by many authors [8] [24] or lifestyle changes in our urban populations as demonstrated by Fezeu and al [25].
Limitations of the Study
· Sample size.
· Lack of ultrasound and hormonal data.
5. Conclusion
At the end of this study, we observed that hirsutism is present in Cameroon and seems normal for most participants. However, we note that it is associated with menstrual cycle disorders, signs of virilization and metabolic syndrome, which suggests that it might not be as harmless as one might think.
Acknowledgements
We acknowledge all the women who took part in this study.
Authors’ Contributions
Francine Mendane and Martine Etoa conducted the study and wrote the manuscript. Laurence Ngo Yon, Mesmin Dehayem, Sandrine Ongnesseck, Eliane Ngassam, and Vanessa Balla helped with data collection, analysis and interpretation of data. Eugène Sobngwi and Jean Claude Mbanya designed and supervised the study. All authors have read and agreed to the final version of this manuscript.
Abbreviations
BMI Body Mass Index
FG Ferriman and Gallwey
HAIR-AN HyperAndrogenism, Insulin Resistance, Acanthosis Nigricans
HDL Hight Density Lipoprotein
IDF International Diabetes Federation
LDL Low Density Lipoprotein
NCEP-ATP III National Cholesterol Education Program-third adult treatment panel
PCOS: Polycystic Ovary Syndrome
Appendix
QUESTIONNAIRE
1. Identification
2. Gynecological history
3. Obstetric history
4. Personal medical history
5. Family past medical history
6. Habits and lifestyle and weight history
7. Information on hirsutism
8. Pshycosocial impact of hirsutism
9. Clinical informations
10. Biological assessment
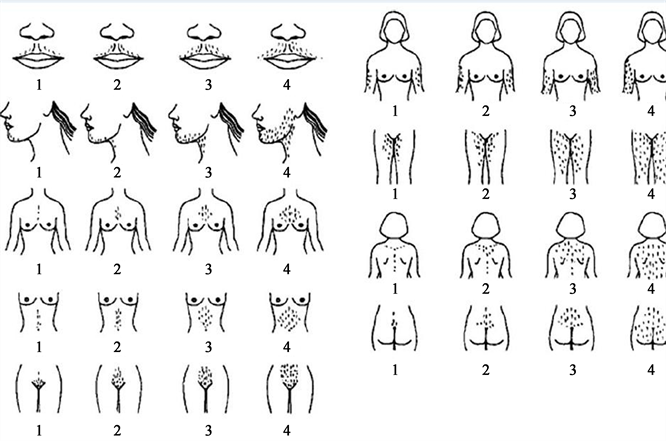
Modified Ferriman Gallwey Score