Assessing High-Fidelity Simulation Outcomes in Continuing Medical Education among Tunisian Practitioners ()

1. Introduction
The training of healthcare providers aims to improve care quality by applying for scientific and technical advances in both initial and continuing medical education (CME). In fact, face to the ongoing change in medical knowledge, the CME seems to be a growing and legitimate requirement by which practitioners can stay current in their medical knowledge and practices. Therefore, over the years, CME programs have evolved into many forms, among these forms, we note a decent appearance of the high-fidelity simulation (HFS) as a new method of learning. Indeed, this decent appearance probably returns to the cost and the logistics performance needs [1] [2]. In this context, the study of Blum et al. recommended as well as the World Health Organization that simulation-based courses should be more widely used in medical education [3] [4].
Thus, simulation was defined by Binstadt et al. as “the use of a device or series of devices to emulate a real patient situation for the purposes of education, evaluation, or research” [5].
Moreover, literature proves that clinical simulation is on the point of offering, to the health care providers, a significant educational method across professional boundaries that meet the needs of today’s medical learners at any stage-undergraduate, graduate, or postgraduate medical practitioners, who are the most needed to keep their skills and abilities updated as close as possible to the real world in a safe, non-threatening environment [6].
Furthermore, HFS has been promoted as an innovative teaching strategy that helps users at all levels, from novice to expert, gain confidence and satisfaction [7] [8] [9] which represent the two outcomes that have been examined by several researchers on the use of HFS. Therefore, by referring to the clinical simulation conceptual framework developed by Jeffries, we found that these two outcomes are directly affected by simulation design characteristics used in the simulation session [10]. O’Donnell et al. reported that simulation design characteristics construct to serve as a fundamental guiding foundation for creation, execution, and evaluation of simulation scenarios [11].
Despite the growing body of research evidence documenting the positive outcomes when using HFS technology in educating healthcare professionals as the junior trainee including both undergraduate and graduate medical education, there is no research focusing on the use of HFS in CME [7] [12] [13].
Even in Tunisia, HFS has not been widely endorsed or used in the CME context, and to our knowledge, our study is the first one dealing with this topic, where its originality.
So, this study was conducted to respond to the following research questions; what are the satisfaction and self-confidence levels of Tunisian medical practitioners in a CME using HFS? And what are the satisfaction and self-confidence correlated factors in terms of design characteristics?
Therefore, our purpose of this research was to assess the satisfaction and self-confidence levels of using HFS among Tunisian medical practitioners in a CME and to determine the correlated factors of satisfaction and self-confidence.
2. Methods
2.1. Type of the Survey and Setting
A cross-sectional study was conducted in the medical faculty’s clinical simulation center in Sousse, Tunisia, in February month 2017.
As part of a CME context using HFS, All the participants were included in our study (n = 40).
2.2. Measures
A self-report method involving questionnaire completion was applied. The questionnaire’s structure consisted of two parts:
Part one elicited socio demographic data, including age and sex.
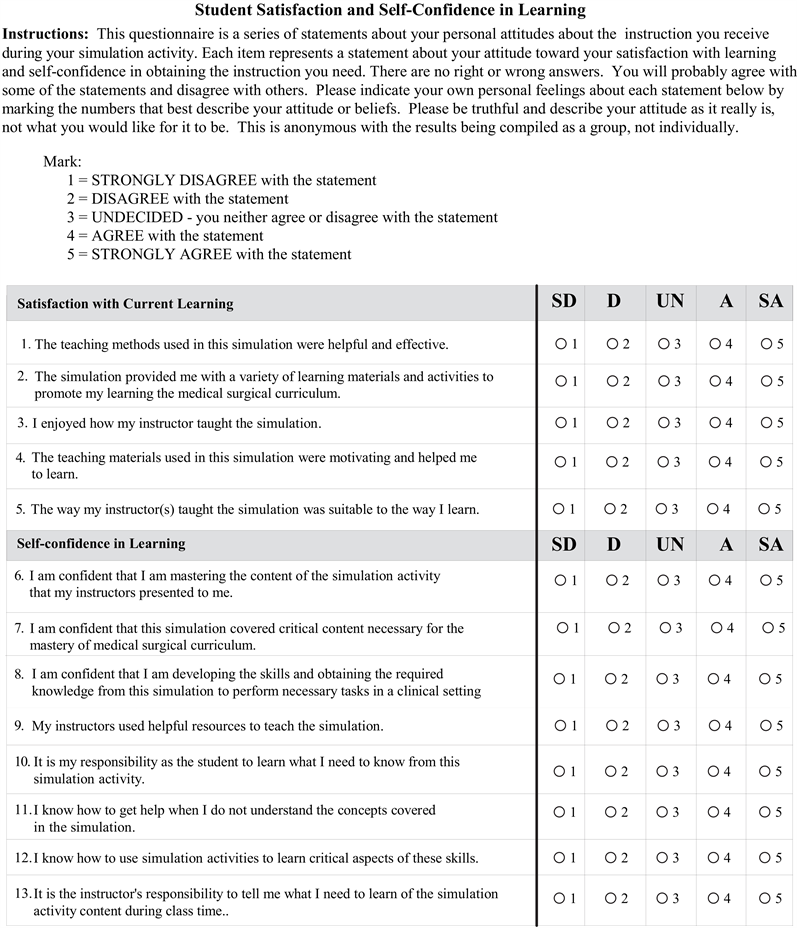
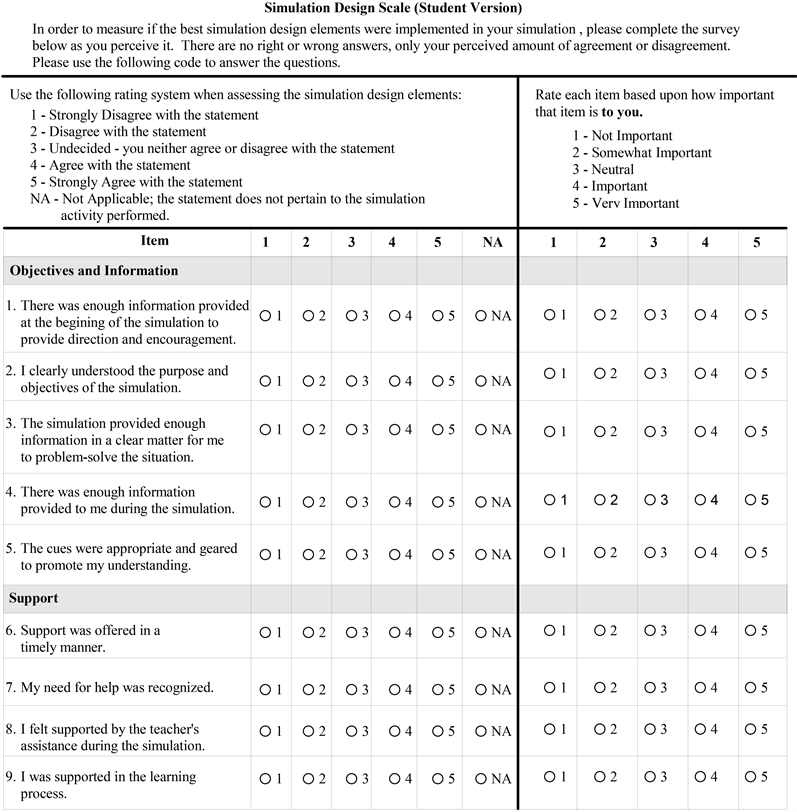
Part two evaluated the simulation design scale and the participant’s satisfaction and self-confidence outcomes. The two used evaluation tools were the Simulation Design Scale (SDS) and the Student Satisfaction and Self-Confidence in Learning Scale which were designed by the National League for Nursing and the Laerdal Multisite Project Group [14]. Participants were invited to complete the tools after the simulation activity as part of a CME. These instruments were used with their original version.
2.2.1. Simulation Design Scale (Annex A)
The SDS is a 20-item tool developed to measure constructs from the Jeffries simulation framework [10]. Content validity was established by 10 experts in simulation development and testing [15]. The instrument’s reliability was tested using Cronbach’s alpha; for presence of characteristics, r ± 0.92, and for importance of characteristics, r ± 0.96 [15]. This instrument uses a Likert-type scale from 1 (strongly disagree) to 5 (strongly agree). The SDS has two parts: 1) the presence of specific characteristics in the simulation and 2) the importance of those characteristics to the learner. The design characteristics rated by the participant include objectives/information (5 items), participant support (4 items), problem solving (5 items), guided reflection and feedback (2 items), and fidelity (2 items) concerning the simulation activity.
2.2.2. Students’ Satisfaction and Self-Confidence in learning (Annex B)
This instrument is a 13-item scale to measure participants’ satisfaction with the simulation activity (5 items) and self-confidence in learning (8 items). Reliability was tested using Cronbach’s alpha; for satisfaction, r ± 0.94, and for self-confidence, r ± 0.87 [16]. A Likert-type scale from1 (strongly disagree) to 5 (strongly agree) was used.
2.3. Data Collection and Analysis
In this study, we distributed a paper-based questionnaire to the participants after obtaining their verbal consent. They could freely and anonymously fill in the questionnaire and return their responses directly to the investigator.
The collected data was analyzed using SPSS version 21. Different methods of data analysis were performed, including descriptive analysis (mean and standard deviation) and bivariate statistics (correlation) using the Spearman’s rho test.
For the simulation design scale, scores are calculated by summing responses where higher scores represent increased recognition of design characteristics in simulation, and the same for the satisfaction and self-confidence scale, scores are calculated by summing responses where higher scores indicate more satisfaction and more self-confidence levels [16].
This study was approved by the ethic committee of medical faculty of Sousse. Administrative authorization has been obtained from the clinical simulation center’s director.
3. Results
3.1. Characteristics of the Participants
All the forty participant physicians were included in the study. The average age of the participants was 30.5 years, with a range of 25 to 50 years. There were 23 women and 17 men.
3.2. Simulation Design Characteristics
All characteristics in the simulation design were rated quite high (all mean scores were higher than 3.5 on the 5-point scale). Problem solving (M = 4.21, SD = 0.48) was the highest rated of the simulation design characteristics. Participant’s support (M = 3.95, SD = 0.8) was the lowest rated of the simulation design characteristics. Table 1 depicts the means for the characteristics on the 5-point SDS (1 = strongly disagree, 5 = strongly agree).
3.3. Students’ Satisfaction and Self-Confidence
The participants were highly satisfied and self-confident satisfied with the simulation experience, which was rating respectively (M = 4.12, SD = 0.52) and (M = 4.25, SD = 0.47) (Table 2).
![]()
Table 1. Results of simulation design scale, N = 40.
3.4. Correlation between Design Characteristics and Satisfaction/Self-Confidence
A statistically significant correlation was noted using the Spearman’s rho. The design characteristics with the highest correlation to both participant’s satisfaction (rs = 0.620) and self-confidence (rs = 0.704) was problem solving, indicating a moderate correlation between this characteristics and the satisfaction and self-confidence’s outcome. The design characteristics with the lowest correlation to both participant’s satisfaction (rs = 0.458) and self-confidence (rs = 0.528) was fidelity (Table 3).
4. Discussion
Nowadays, reforms in CME, returns a crucial need and the major way to update practitioners’ skills, to maintain the best quality of services offered and to promote patient safety [17]. Actually, CME best practices in educational programs are depending on the following statements: mastery learning and deliberate practice. For this reason, simulation-based medical education can be used as a teaching technique allowing these statements achievement [2].
In this respect, Weller, reported that simulation is a popular and effective method of CME for both medical specialists and trainees [18]. As well, the 2008 Academic Emergency Medicine Consensus Conference, “The Science of Simulation in Healthcare: Defining and Developing Clinical Expertise” was organized to help define a national research agenda for maximizing effective use of simulation across undergraduate, graduate, and CME [19].
![]()
Table 2. Results of participant’s satisfaction and self-confidence, N = 40.
![]()
Table 3. Correlation (rs) between design characteristics and satisfaction/self-confidence, N = 40.
**Indicates significance at 0.01.
However, in spite of the growing use of HFS in medical education, there is a shortage of research-based evidence regarding the best simulation practices. Hence, given its increased use, we perceived the need to understand the outcomes derived from this innovative teaching strategy and the factors that contribute to these outcomes.
In our study, we demonstrated that all participants were highly satisfied and self-confident with the simulation experience which were respectively rating (M = 4.11, M = 4.25). As a matter of fact, these findings were concluded by several authors, who proved that HFS enhances the self-confidence and satisfaction scores because it required them to participate, think, and act. Also, it afforded them a safe clinical environment [20] [21]. In general, the literature support is that, in every HFS experience, participants felt positive [7] [22] [23].
In the evaluation of the simulation design characteristics, all parts were highly rated (Table 1). However, problem solving was the highest rated (M = 4.21, SD = 0.48). This result was lower as that was founded in Smith and Roehrs’s study (M = 4.6, SD = 0.4) [21]. In addition, Murphy reported that experiential learning pedagogy such as clinical simulation exercises encourage the integration of clinical concepts; promote problem solving and clinical reasoning as well as critical thinking, teamwork and communication [24].
As for the design characteristic participant’s support has the lowest score. In fact, this result, seems unexpected since the instruction using simulation is participant centered, in which the role of the facilitator is to assist the participant to learn and think. Another design characteristic with a very low score was information and objectives. This result might be due to the reason that participants may have received too much information that they needed to keep in mind in a short amount of time [25]. In this context, it is interesting to note that we have found nearly the same result as other researches [20] [21].
Depending to the Nursing Education Simulation Framework the two mains outcomes of satisfaction and self-confidence are directly influenced by design characteristics [10]. Thus, the correlation analysis of the five simulation design characteristics and the simulation outcomes revealed that all of these characteristics were significantly correlated with practitioners’ satisfaction and self-confidence. This result was found in several studies [21] [25] [26]. In fact, in our study, problem solving was the most strongly correlated design characteristic. This finding supports the notion that participants who learned problem solving through HFS reported a greater sense of being involved and they valued this educational practice more than did participants using other methods [14]. Therefore, problem solving and critical-thinking skills are an essential component of HFS.
Moreover, the design characteristics that included objectives/information and feedback/guided reflection emerged as significant correlated factors with both satisfaction and self-confidence. In this context, research suggests that simulation objectives should be specific, detailed, clear and matching the participant’s knowledge and his HFS experience level [10] [15]. Regarding, guided reflection characteristic, it is a critical component of the simulation experience. However, providing reflection during the scenario may provide additional insight into the patient’s condition and aid in setting goals for the patient’s care [26].
To conclude, the significance correlation of design characteristics with the participant’s satisfaction and self-confidence outcomes imply that medical educators must carefully consider the design of any HFS experience. However, many boundaries may impede taking into account those design characteristics, including increasing the time required to appropriately address them. So, in order to ensure that all of those design characteristics are appropriately addressed, the literature recommended the necessity of implementing a template [27].
This study provides an overall assessment of the HFS effectiveness in a CME in terms of satisfaction and self-confidence outcomes among Tunisian medical practitioners. We recommend the integration of this novice and powerful tool for physicians and other healthcare professionals at all levels, and across all disciplines, as well as in supporting professional practice development and CME [17]. We also recommend setting up, in our hospitals, clinical simulation centers which must be adequately equipped to offer CME training programs.
We also note the need to explore this domain by making other studies deal with varied participants, different medical education programs, larger sample sizes and multiple types of learning experiences. Finally, our key lesson is that CME in any form should be based on scientific best evidence [28]. So, educational technologies such as HFS will be best used to complement, not replace, education grounded in patient safety.
This present study has strengths and limits. As for strengths, we note the originality of this topic since it is up to date and relevant in CME programs, given that, this is the first study assessing HFS outcomes in a CME context among Tunisian practitioners. Actually, in terms of the outcomes, we have noted that participants feel positive about the HFS experience involving critical care without the stress of a real patient, and increase confidence by giving opportunities for critical thinking and decision-making, which could lead to improving practitioners’ self-motivation, best care quality and patient safety. As a final point, simulation-based learning can help develop health professionals’ knowledge, skills, and attitudes while protecting patients from unnecessary risks [29].
As for limits, the assessment of HFS outcomes using a self-administered questionnaire can be associated with a declaration bias; otherwise, this bias is generally present in all studies based on a questionnaire. Moreover, by insisting on the anonymity and on the study’s objectives, we reduced this bias to the maximum.
5. Conclusion
In addition to the fact that simulation has recently emerged in our Tunisian CME programs and gained acceptance by healthcare practitioners, our results showed that it is also a satisfying and effective tool for increasing practitioners’ satisfaction and self-confidence in a CME context. Therefore, in order to update medical information and skills, a call for CME reform seems to be a pressing necessity. Then, Tunisian educators must encourage this valued pedagogy tool and push outside of their comfort zones to introduce HFS in CME increasingly.
Annexes
Annex A: Simulation Design Scale

Annex B: Student Satisfaction and Self-Confidence in Learning