Self-Reported Use of Personal Protective Equipment during the SARS-CoV-2 Pandemic in Emergency Medical Service Employees in Germany—A Survey ()
1. Introduction
On 23rd January, 2020, according to the World Health Organization (WHO), the first official SARS-CoV-2 cases were reported in Germany [1]. SARS-CoV-2 or severe acute respiratory syndrome coronavirus type 2, a beta coronavirus, is the cause of the COVID-19 disease [2].
Over the course of the pandemic, an occupational risk for medical staff to contract COVID-19 was reported [3] [4] [5], as well as how transmission between medical personnel had been underestimated at the start of the pandemic [6]. On the 25th of May 2021, the Centers for Disease Control and Prevention reported 491,816 healthcare workers in the United States to have been infected with COVID-19 [7]. No up-to-date figures are available regarding healthcare workers’ infections worldwide, with estimates from the WHO dating back to 2020 [8]. There have been other efforts to collect data on healthcare workers’ infections worldwide, however, these mostly focus on the year 2020 and do not include data from all countries [9] [10].
The main focus regarding COVID-19 occupational risks has been on hospital staff [5] [11] despite Emergency Medical Services (EMS) staff also having a high risk of exposure and infection with the virus [12] [13]. Some studies state that EMS staff have an increased risk of being infected with SARS-CoV-2 compared to the general population [14].
EMS personnel are often the first to attend to patients in situations that can be disordered and characterized by lack of information and time pressure [15] [16] [17]. These factors can negatively impact the adherence of EMS staff to PPE recommendations [18].
Availability and correct use of PPE is one important factor in protecting healthcare staff from infectious diseases, not just during the current pandemic. Particularly during the initial stages of an outbreak, when treatment options or vaccines are not available yet or only available in a limited number, PPE plays a vital role in safeguarding the health of medical and paramedical staff [19] [20].
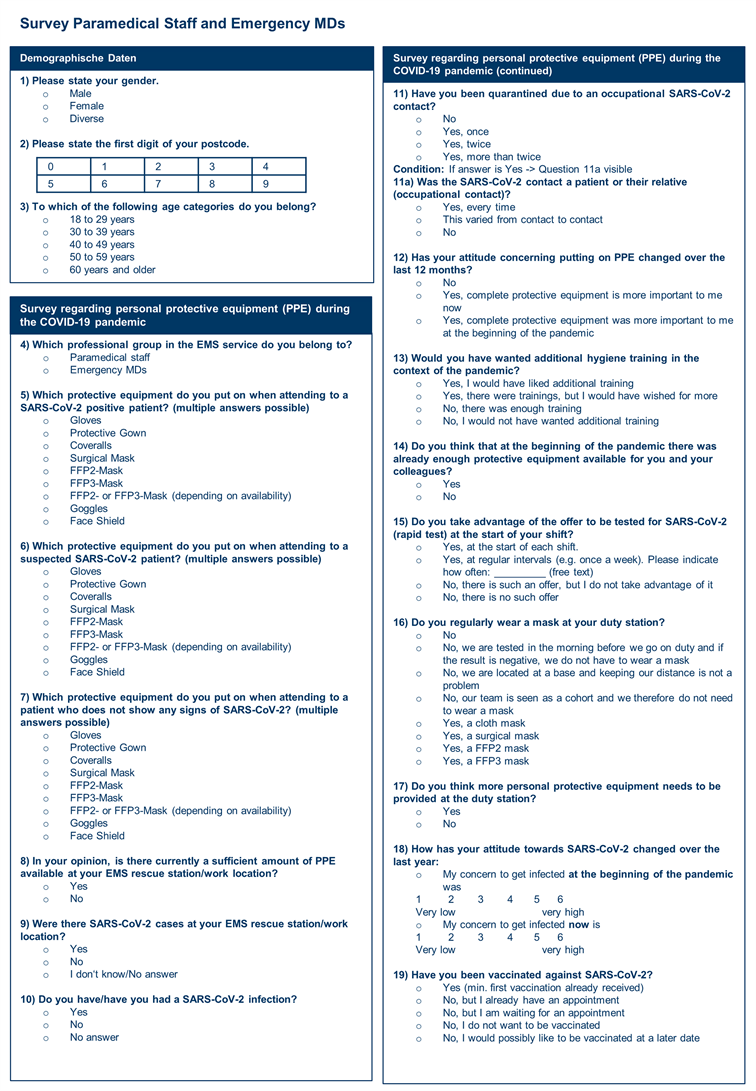
Since current scientific data and reporting on SARS-CoV-2 occupational risk for German EMS workers is very limited, a survey was conducted in March 2021 by the University Hospital Schleswig-Holstein, Institute for Emergency Medicine (IRuN) in Kiel. To our knowledge, this is the first study of this kind conducted in Germany.
The primary objective of the survey was to take stock of the use and availability of PPE in German EMS personnel during the SARS-CoV-2 pandemic. The secondary objective was to generate additional data on individual perceptions of risk of infection and occurrence of infections at the respective places of service.
2. Methods
2.1. Study Design and Setting
The survey, a multicentric prospective cohort investigation, was conducted between 1st of March and 1st of April, 2021 via the online survey tool Lime Survey (Version 4.5.2 + 210426). The survey questions were developed by the IRuN in collaboration with the Robert Koch-Institute (RKI), Berlin. Questions focused on availability and use of PPE, quarantining and COVID-19 infections among EMS staff.
Ahead of the distribution of the survey, a test version was shared with a small group of peers who had not been involved in the survey design. Their remarks were taken into consideration when finalizing the survey.
The survey was conducted at two levels—EMS managers and medical and paramedical EMS employees—with questions adapted slightly to fit the respective study population. This design was chosen to be able to compare whether assessments and experiences at the managerial level corresponded to those of the employees.
The questionnaire aimed at the EMS managers contained 15 questions, whereas the one for EMS employees contained 19 questions.
Responses were collected anonymously except for the first digit of the postal code. This data helped identify whether responses were received from across the nation.
Specifically for EMS managers, the size of the EMS area of operation (in size categories) was queried. Specifically for EMS employees, age (in age categories) and gender were asked.
This data was collected to potentially be able to design more specific and appropriate recommendations at a later stage.
2.2. Study Population
The survey was designed for German EMS managers and EMS employees. Participation in the survey was voluntary. To reach the desired study population, the survey was distributed via specific channels, which are detailed in the following paragraphs for both groups.
To recruit participants from the group of EMS managers, the contact databases of the IRuN were used, which contain details of medical directors of EMS services (Ärztlicher Leiter Rettungsdienst) for each region in Germany. A total of 150 personalized invitations were sent out. Participation in this group was only possible by entering a personalized code received via e-mail.
To recruit participants from the group of EMS employees, a different approach was used to get maximum participation in the survey. The questionnaire was made available openly and shared via social media channels focusing specifically on emergency medicine, existing EMS contacts from the Institute’s database, and personal contacts in various EMS.
A minimum sample size of 325 participants in the group of EMS employees was needed to conduct the goodness of fit test (effect size 0.2; α = 0.05; df = 1; power = 0.95) and to show the differences in mask use between paramedical and medical staff.
2.3. Data Protection
Data was collected via the online survey tool Lime Survey (Version 4.5.2 + 210426) hosted on a server in Germany. Answers for both groups were anonymized automatically through the survey tool. This was done to ensure that no correlation between the personalized invitations and the respective responses could be made. No personal data of study participants which could be used to draw conclusions about their identity was collected. After completion of the survey, the collected data was imported into Microsoft® Excel® (V.1808; 2019 MSO), as well as IBM SPSS Statistics V.26 and evaluated. The data evaluation took place in Germany.
2.4. Ethical Considerations
The survey was approved by the University of Kiel ethics committee (D422/21). Information about the purpose of the survey and the use of participants’ anonymized answers was given on the welcome page of the survey. Participants were advised that by proceeding, they would consent to their answers being used for further analysis and publications.
2.5. Analysis
Descriptive analysis on absolute and relative frequencies was performed for the data on PPE availability and use, both when attending to patients and at the EMS station, as well as the estimates of infected or quarantined staff. PPE use was further divided into encounters with patients with confirmed, suspected or no indication of a SARS-CoV-2 infection. The χ2 goodness-of-fit-test was used to evaluate whether mask use changed according to the SARS-CoV-2 infection category and depending on the type of EMSstaff—paramedical or medical. The test was completed with df = 1 and α = 0.05.
3. Results
3.1. Respondents and Respondent Rates
A total of 34 responses were received in the managerial group, whereas a total of 2389 responses were received in the group of employees. Of these, 28 and 2078 answers were considered complete, respectively.
150 invitations were sent out in the managerial group. With 28 complete answers received, 18.7% of the targeted persons responded. Judging from the first digits of the postal codes submitted, answers were received from all federal states of Germany. Half of the respondents (50.0%, n = 14) in this group stated their EMS area of operation employed 300 or more staff. 25.0% (n = 7) were responsible for 100 to 199 employees, followed by 14.3% from areas of operation with 200 to 299 (n = 4), and 10.7% with less than 100 (n = 3) employees.
In the survey for EMS employees, of the 2078 persons that responded to the question on profession, 80.8% (n = 1678) stated they belonged to the group of paramedical staff, whereas 19.2% (n = 400) stated they were Medical Doctors. Regarding overall gender distribution, 22.0% (n = 454) of respondents were female, 0.1% (n = 2) diverse and 77.9% (n = 1612) male.
Due to the nature of the study, representativeness of this group can only be approximated by comparing the results to similar historical studies that focused on the same study population and had a similar size.
A study conducted in 2017 [21] among 714 German EMS personnel stated a gender distribution of 17.7% female and 82.3% male whereas a more recent study conducted in 2021 [22] stated a distribution of 21.8% female and 78.2% male. Two other studies examined just Emergency Medical Doctors [23] (22.2% female, 77.7% male) and paramedical staff [24] (13.8% female, 86.2% male). The results of these studies were similar to the present survey with 27.8% (n = 110) female and 72.2% (n = 285) male emergency doctors and 20.6% (n = 344) female, 79.3% (n = 1327) male, and 0.1% (n = 2) diverse paramedical staff.
Regarding age distribution the most recent comparable study [22] found a very similar age distribution to the present survey with 30% being 18 - 29 years (present study: 34.2%, n = 708), 33.8% 30 -39 years (present study: 30.6%, n = 634), 21.7% being 40 - 49 years (present study: 21.1%, n = 437), 12% being 50 - 59 years (present study: 11.4%, n = 236) and 1.5% being 60-69 years (present study: answers on age 60 or above: 2.3%, n = 57). Another study focusing only on paramedical staff [24] also stated very similar age demographics to the present study.
Answers were received from all federal states of Germany judging from the first digits of the postal codes submitted.
Overall, the demographic data distribution of EMS employee respondents compares to those of previous studies focusing on the same study population.
See Figure 1 for the overview on general respondent data for both EMS managers and employees.
3.2. Mandatory PPE
Of the 28 EMS managers that responded to the survey, all (100.0%) stated that gloves, protective gown or coveralls, and FFP21 or FFP32 masks had to be worn
in their area of operation when attending to SARS-CoV-2 positive patients. Goggles were stated as mandatory in 96.4% (n = 27) of cases, whereas 35.7% (n = 10) replied that face shields had to be worn. None (0.0%) stated that simple surgical masks were mandatory (Table 1).
In terms of mandatory PPE for suspected SARS-CoV-2 positive patients, answers changed slightly. Recommendations to use surgical masks (0.0%) and face shields (35.7%, n = 10) remained the same. Mandatory use of gloves, as well as FFP2 or FFP3 masks dropped to 96.4% (n = 27) and use of protective gown or coveralls to 92.8% (n = 26). Answers on the use of goggles dropped even further to 82.1% (n = 23) (Table 1).
Regarding mandatory PPE when attending to patients with no signs of a SARS-CoV-2 infection, figures changed more significantly with 92.9% (n = 26) stating mandatory use of gloves and 89.3% (n = 25) FFP2 or FPP3 masks. Only 3.6% (n = 1) respectively stated that gowns or coveralls, surgical masks and face shields had to be used. Finally, 32.1% (n = 9) stated that goggles were mandatory when attending to these types of patients (Table 1).
3.3. Use and availability of PPE
For the EMS employees, among the 2078 staff that responded, the majority stated that when attending to SARS-CoV-2 positive patients, they wear gloves
![]()
Table 1. Mandatory PPE according to EMS managers.
(99.8%, n = 2073), FFP2 or FFP3 mask (total: 99.8%, n = 2073), protective gown or coveralls (total: 99.1%, n = 2060) and goggles (89.7%, n = 1863). Face shields (24.0%, n = 498) and surgical masks (0.0%) were the equipment least cited when attending to a SARS-CoV-2 positive patient (Table 2).
The figures changed slightly when respondents were faced with the question on PPE use for suspected SARS-CoV-2 positive patients. The stated use of gloves (98.8%, n = 2053), FFP2 or FFP3 masks (total: 99.4%, n = 2065) and surgical masks (0.2%, n = 4) remained on a similar level. However, use of gowns or coveralls (total: 95.9%, n = 1993), goggles (85.6%, n = 1778) and face shields (19.2%, n = 400) decreased slightly (Table 2).
When attending to patients without signs of SARS-CoV-2, answers changed more significantly in several categories. Use of gloves (95.7%, n = 1988), FFP2 or FFP3 masks (total: 97.5%, n = 2026) and surgical masks (1.5%, n = 31) remained on a similar level to the previous questions. However, use of protective gowns or coveralls (total: 5.9%, n = 122), goggles (36.9%, n = 766) and face shields (2.6%, n = 53) all dropped to much lower levels (Table 2).
See Figure 2 for an overview of the answers of EMS managers and employees on PPE use.
The total use of both FFP2 and FFP3 masks was further analyzed to determine whether there were differences in mask use between paramedical and medical staff. For PPE use in a SARS-CoV-2 positive patient (Table 3), the χ2 result showed an asymptotic significance of 0.231. For PPE use in a SARS-CoV-2 negative patient (Table 3), the χ2 result showed an asymptotic significance of 0.155.
In terms of the availability of PPE, the majority of respondents (75.3%, n = 1524) stated that at the beginning of the pandemic there was not enough PPE available at their workplace (n = 2024). In comparison, at the time of answering the survey, the majority of EMS employees (87.6%, n = 1783) stated that they were of the opinion that there was now enough PPE available at their workplace (n = 2035).
EMS managers were only asked whether they were of the impression that there was now enough PPE available in their EMS area of operation. 26 respondents (92.8%) confirmed that – according to them – this was the case. Two EMS managers skipped this question.
3.4. Mask use at the EMS Station
Concerning the mask used at the EMS station, 43.4% (n = 903) of the 2,053 EMS employee respondents stated that they regularly wear a FFP2 mask at their station, whereas 42.2% (n = 877) responded that they wear a surgical mask. 5.1% (n = 105) stated they do not wear any mask, 5.0% (n = 103) replied that they are stationed at a base and keeping their distance is not an issue, and 2.0% (n = 42) said staff teams are seen as a cohort and therefore do not need to wear a mask. 0.5% (n = 11) do not wear a mask since they are being tested at the start of their shifts, 0.5% (n = 10) stated that they wear a cloth mask, whilst 0.1% (n = 2) wear a FFP3 mask 0.25 (1.2%) EMS employees did not answer the question.
![]()
Table 2. Use of PPE according to EMS employees.
![]()
Table 3. Use of FFP2 or FFP3 masks.
3.5. SARS-CoV-2 Infections and Quarantine
27 respondents (96.4%) in the EMS managers group stated that there had been SARS-CoV-2 cases at their EMS area of operation. One person did not answer the question.
Regarding quarantine, 53.6% (n = 15) stated less than 5% of their employees had been quarantined due to an occupational SARS-CoV-2 contact. 21.4% (n = 6) estimated the number of quarantined staff at 5% to 10%, whereas 3.7% (n = 1) estimated this figure at 30% to 40%. 3.6% (n = 1) responded that none of their employees had to quarantine due to an occupational contact and 14.3% (n = 4) did not know. One person did not answer the question.
In contrast, 62.1% (n = 1291) of EMS employees stated that there had been SARS-CoV-2 cases at their EMS station. The number of staff who stated that they had been infected themselves was 122 (5.9%). 12 EMS employees skipped this question.
Of 2060 EMS employees that answered the question on whether they had been in quarantine at least once themselves due to an occupational contact, only 448 (21.6%) answered “Yes”. 18 EMS employees decided to not answer this question.
Finally, out of the 21.6% stating that they had been quarantined, 46.9% (n = 210) answered that this was due to contact with a patient or relative of the patient, 17.5% (n = 76) stated that it varied and 34.4% (n = 154) responded that their quarantine was not due to contact with a patient or relative.
4. Discussion
The above results show high self-reported adherence to PPE of German EMS employees during the SARS-CoV-2 pandemic. However, there is a general lack of studies analyzing PPE use in German EMS employees before the onset of the SARS-CoV-2 pandemic. International studies conducted before the SARS-CoV-2 pandemic often observed a general lack of adherence to PPE protocols in EMS workers [16] [18].
Behavior was self-reported in the survey and despite it being anonymous, it might not be coherent with day-to-day practices. This was reported previously in other studies where self-reported behavior and actual behavior were not congruent [25].
The RKI has released general recommendations concerning PPE for healthcare workers, which state that the following should be worn when attending to a suspect or confirmed SARS-CoV-2 positive patient: protective gown, gloves, mask (minimum FFP2 when directly caring for suspected or confirmed positive cases, simple surgical masks are not seen as providing enough protection) and goggles [26]. However, these are recommendations only. There are no PPE guidelines for EMS workers that are applicable nationwide.
Looking at the responses from EMS managers regarding mandatory PPE for SARS-CoV-2 positive and suspected SARS-CoV-2 positive patients, all of them agreed with the above recommendation that gloves, protective gowns or coveralls and FPP2 or FFP3 masks had to be worn when attending to SARS-CoV-2 positive patients. Only the stated use of goggles was not in line with the recommendations.
When attending to suspected SARS-CoV-2 positive patients, the EMS managers however did not fully agree with the above, with all stated use of recommended PPE dropping to below 100%.
As for the EMS employees, self-reported adherence to the RKI recommendations and guidance from EMS managers when attending to confirmed SARS-CoV-2 patients is good. Over 99% of staff state to be using gloves, FFP2 or FFP3 masks as well as protective gowns or coveralls when attending to this patient group. Only the use of goggles is reported at a lower level.
When attending to suspected SARS-CoV-2 positive patients, adherence to the recommendations drops slightly. Whereas the use of gloves and FFP2 or FFP3 masks remains at over 98%, the reported use of gowns or coveralls and the use of goggles is reduced further.
Previous studies have found that the use of gloves has generally been good in EMS staff [16], whereas the use of protective masks left room for improvement [20]. This does not seem to be coherent with the findings of this study, indicating that since the beginning of the SARS-CoV-2 pandemic mask use of EMS staff has been improved.
One thing that stands out from the survey is that the use of goggles in both confirmed and suspected SARS-CoV-2 patients is neither recommended by all EMS managers nor stated as being used by EMS employees. This is something that should be looked at and recommendations and behaviour ideally adjusted, since transmission of the virus does occur via infected secretions, such as droplets, which can be absorbed via the mucosal skin of the eyes [27].
A possible explanation for the stated low percentage of use of goggles could also be that guidelines of certain EMS providers are not in line with the recommendations of the RKI and in certain cases, face shields are used instead of goggles.
An additional important point for EMS managers and employees to note is that the recommendation on PPE use for suspected SARS-CoV-2 patients by the RKI is the same as for confirmed patients. Adherence to these recommendations was found to be less than 100.0% in the findings of the survey. Again, this should be monitored and if possible guidelines and behaviour adjusted, in order to ensure the best possible protection of EMS staff.
Another aspect analyzed was difference in mask use between medical and paramedical staff. According to the participant’s answers, there is no significant difference between mask use in paramedical or medical staff—whether the patient attended to is SARS-CoV-2 positive or not.
On 30th of April, 2021, according to the German RKI, a total of 3,381,597 people were infected with the SARS-CoV-2 virus in Germany [28]. This equates to approximately 4.0% of the German population.
EMS staff have a high likelihood of getting infected with SARS-CoV-2 due to their occupational exposure risk. Nonetheless, the low number of staff (5.9%) stating that they had been infected with SARS-CoV-2 themselves, which is only slightly higher than the overall infection rates within the German population, could support the assumption that the adherence to PPE use recommendations is good within the EMS workforce.
Since the date of infection was not requested in the survey, no conclusions can be drawn from the reported lack of PPE at the beginning of the pandemic in 2020 and the number of infections that might have resulted from this. In addition, no data was collected on whether staff who had been infected with SARS-CoV-2 contracted the disease at their place of work.
Another result that could potentially support the indicated good use of PPE when attending to patients is regarding quarantine. Over a third of EMS staff who had to quarantine due to an occupational contact responded that this was not due to contact with a patient or a patient’s relative. A possible explanation for this could be that during contact with patients or their relatives, proper PPE was worn and that therefore, the above staff were not in proper PPE when in contact with the person due to which they had to quarantine.
When in contact with colleagues at the EMS station, most staff stated they were either wearing a surgical or FFP2 mask. The use of surgical masks at places of work in Germany was legally deemed necessary on the 21st of January, 2021 [29]. A total of 13.1% of EMS employees stated that they wear cloth masks or no masks at all at the EMS station.
The survey however does not show a correlation between lacks of PPE or mask use at the EMS station and staff quarantine. This is something that should be investigated further.
5. Limitations
Recruitment of EMS employees was done via an open invitation on social media, existing contacts from the institute’s database, and through personal contacts in various rescue services. Participation in the survey was voluntary and selection effects cannot be ruled out. However, the demographic data of respondents is comparable to previous studies focusing on the same study population. Therefore, we assume that selection effects have not distorted the results.
6. Conclusion
Overall, the survey points to German EMS staff using proper PPE and protecting themselves well during the current SARS-CoV-2 pandemic. More research needs to be done on this topic, also conducting observational studies to confirm the self-declared statements of staff. If confirmed, another interesting aspect to focus on would be the reasons for improved use of PPE compared to previous studies. This information could inform how education, training and health promotion on PPE use for EMS workers could be communicated in the future in order to better protect EMS staff.
Declarations
Ethics Approval and Consent to Participate
The survey was approved by the University of Kiel ethics committee (D422/21). Information about the purpose of the survey and the use of participants’ anonymized answers was given on the welcome page of the survey.
Consent for Publication
Information about the purpose of the survey and the use of participants’ anonymized answers was given on the welcome page of the survey. Participants were advised that by proceeding, they would consent to their answers being used for further analysis and publications.
Availability of Data and Materials
All data relevant to the study are included in this published article.
Authors’ Contributions
JTG and JW conceived of the study. TB drafted the protocol, which was reviewed by JTG, JW, MZ and JK. JK drafted the survey questions, which were reviewed by JTG, JW, MZ, LH and TB. MZ implemented the survey online. TB prepared and analyzed the data, which was reviewed by JTG, JW, MZ, JK and BA. The final manuscript was drafted by TB and reviewed and approved by all contributors.
Acknowledgements
We thank Univ.-Prof. Dr. Lefering for his guidance and support on data and statistics for this article. We also thank Hanna-Joy Renner for carefully reviewing the manuscript.
List of Abbreviations
COVRIIN COVID-19 Expert Working Group Intensive Care, Infectiology and Emergency Medicine
EMS Emergency Medical Services
IRuN Institute for Emergency Medicine, Kiel
PPE Personal Protective Equipment
RKI Robert Koch-Institute
WHO World Health Organization
Appendices

NOTES
*These authors contributed equally to this work.
#Corresponding author.
1At least 94% filtration capacity, similar to N95 mask.
2At least 99% filtration capacity, similar to N99 mask.