The Self-Administered International Prostate Symptoms Score (IPSS) Questionnaire of Kosovo Men with Benign Prostatic Hyperplasia ()
1. Introduction
Benign prostatic hyperplasia (BPH) is a common condition as men get older. An enlarged prostate gland can cause uncomfortable urinary symptoms, such as blocking the flow of urine out of the bladder. Lower urinary tract symptoms (LUTS) due to benign prostatic hyperplasia (BPH) are common conditions in middle-age or older men [1]. The International Prostate Symptom Score (IPSS) is a useful and validated questionnaire to evaluate LUTS secondary to BPH [2]. However, BPH is considered for the vast majority of LUTS. BPH causes symptoms in approximately 90% of men over the age of 55 years old and one-third of men will develop urinary tract symptoms once in their life [3] [4] [5] [6].
The primary goal for treating men with BPH-LUTS is usually to relieve symptoms and to prevent them [7].
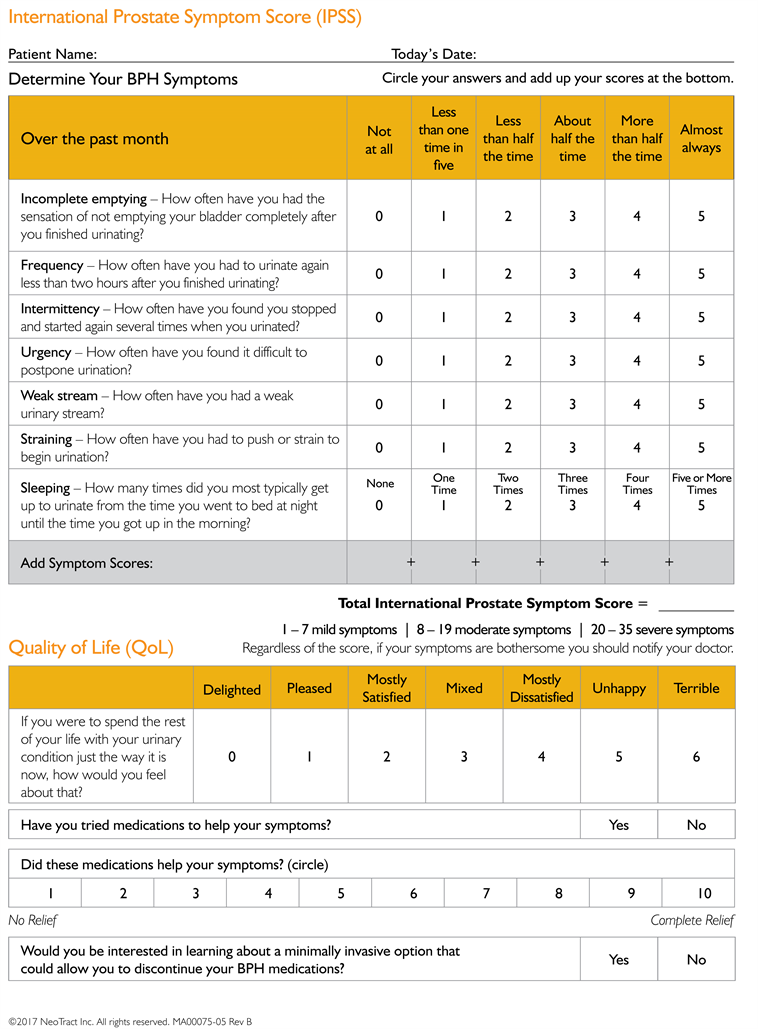
The most important issue is that the IPSS questionnaire should be self-administered as this will eliminate the possible bias that may be associated with physician-assisted or health worker-assisted administration. This instrument measures the severity of voiding and storage symptoms (see Appendix) and consists of 7 items of the International Prostate Symptom Score, referred to in this article as the IPSS (see Appendix) [8]. Therefore, guidelines recommend that the IPSS questionnaire be used as a mandatory test in the evaluation and follow-up of LUTS and BPH [9].
This study was in terms of the initial evaluation of LUTS and BPH, and the assessment of changes in symptom severity before and after medication and the quality of life of patients with benign prostatic hyperplasia.
Much of the research to date has focused to evaluate the relationship between lower urinary tract symptoms (LUTS), different diagnostic indicators of benign prostatic hyperplasia (BPH) [10], and relationship between prostate inflammation and lower urinary tract symptoms (LUTS) due to benign prostate hyperplasia (BPH) has raised the urological interest in the recent years, due to new evidence that supports this potential link [11], and some of the research has focused on surgical or medical management of symptoms, but there is growing interest in identifying preventive measures for reducing the burden of LUTS by identifying risk factors associated with these symptoms, especially those that are potentially modifiable [12]. Other risk factors include comorbidities, such as diabetes, cardiovascular disease, hypertension and the side effects of the pharmacological treatments for these comorbidities [13]. Other postulated but not yet clearly established factors associated with LUTS include higher body mass index (BMI), lower socio-economic status, being married, family history, dietary and lifestyle factors (such as alcohol, caffeine, smoking, physical inactivity), history of sexually transmitted disease, other prostate conditions and ethnicity [11] [12] [13] [14] [15].
2. Materials and Methods
2.1. Patients and Study Design
This was a prospective, observational, study to evaluate change in Qol in patients with moderate-to-severe LUTS/BPH managed in a urological setting. The study was performed in the University Clinical Centre of Kosovo—Urology Clinic—Kosovo from October 2020 to January 2021. A total number of 100 patients who presented themselves to the urology outpatient department with LUTS due to BPH were enrolled in the study.
The study inclusion criteria were as follows: all patients who presented themselves to the urology outpatient clinic with BPH, LUTSs were aged > 40 years.
The exclusion criteria included the following cases: patients with uncontrolled diabetes (prostate-specific antigen > 4 ng/dL); patients with a history of transurethral resection of the prostate and patients who underwent surgery for urethral vesicle calculus in the past.
2.2. Sample Size
The selection of patients included in the study was randomized by analyzing inclusive and exclusion criteria.
2.3. LUTS Assessment
The collected medical histories from the enrolled patients. On their initial visit, respondents were issued IPSS (English version). The sum of IPSS questions 2, 4 and 7 related to irritative symptoms: and the sum of IPSS questions 1, 3, 5 and 6 related to obstructive symptoms.
3. Follow-Up and Outcomes
Patients with symptoms score of 20 - 35 had severe symptoms of IPSS where 52% of them were treated with Alpha Receptor Blockers, 5 alpha-reductase inhibitors and prostatectomy (TUR-P, PTV), while patients with moderate symptoms (41%) were treated with 5 alpha-reductase inhibitors and herbal extracts, and patients with mild symptoms (7%) were treated with careful observation and waiting and herbal extracts.
The questionnaire consists of seven questions on incomplete bladder emptying, frequency of micturition, intermittency, urgency, weak stream, straining and nocturia. There is an 8th question on the quality-of-life assessment in relation to the urinary symptoms.
Statistical Analysis
Values are expressed as Mean ± SD for continuous variables and percentage for dichotomous data. Continuous data was compared with two-tailed Student t-test and discrete data with Chi-square test. Quantitative data was analyzed through the SPSS statistical program.
4. Results
This study was carried out on 100 consecutive patients suffering with HBP and LUTS. The average age of the participants was 69 ± 0.726. From 100 patients surveyed 7% of them had mild symptoms, 41% had moderate symptoms and the largest number of them 52% had severe symptoms. Most of the participants (76%) were married, (90%) were Albanian. Regarding education level most of them (36%) were only educated at primary school level or below. Higher proportions of them (53%) were pensioners. 51% of them were living in a village. The majority of the participants were Muslim (92%) and (55%) of them were smokers. When asked if they use the Anti-hypertensive drugs, the majority of the patients declared yes (68%), whereas (32%) declared no. When questioned about a family history of prostate disease, 67% of them declared that they did not have a history of this in their family (Table 1).
Regarding the symptomatology between patients living in the city and in a village: out of 100 patients, most of them (29%) stated that they had the feeling of not emptying the bladder less than one in five times. Comparing the place of settlement, we did not find a statistically significant relationship between the settlement in the village and in the city: Village Mean-SD (2.63 ± 1.37) and Mean Rank 55.52, while Mean-SD city (2.14 ± 1.36) and Mean Rank 45.2 p < 0.679. In terms of frequency when comparing patients living rurally and in urban areas, we did not gain a statistically significant relationship: Village (2.61 ± 1.41), Mean Rank: 54.85, City (2.14 ± 1.30), Mean Rank 45.97 p < 0.203. Regarding the interval of urination, 30% of the patients had to stop and start the act of urination again. Comparing the place of residence, I did not find a statistical reliability p < 0.338. 24% of patients had emergency urination p < 0.36. Most patients, 32% of them, had low blood pressure during urination p < 0.25. In answer to the question: how often they have had to push or strain to begin urination, most of them (36%) had to do this almost always. We compared this with village residence: (3.25 ± 1.27), Mean Rank 54.79 and patients living in the city (2.9 ± 1.27) Mean Rank 46.03 p < 0.256. 28% of them urinate 2 times per night p < 0.256 (Table 2).
According to the terms of IPSS categorization most patients (52%) were experiencing severe symptoms, 41% had moderate symptoms and only 7% had mild symptoms.
Comparing the three levels of IPSS and the quality of life of patients with HBP and LUTS, when asked how they would feel if they still had problems with urination, 22% of them said that they would feel upset. Analyzing the categorization of patients according to IPSS: mild symptoms were: Mean/SD (1.71 ± 1.113),
![]()
Table 1. Main socio-demographic and health conditions results (n = 100).
![]()
Table 2. Symptomatology between patient’s perception to living in the center and village.
Moderate symptoms (2.9 ± 1.49) and severe symptoms (4.31 ± 1.27) p < 0. 156. Statistical reliability of 64% p < 0.000 was in patients where they were interested in learning about any invasive option that would allow them to discontinue medication for LUTS (Tables 3-5).
5. Discussion
The purpose of this study is to evaluate psychometric properties including validity and quality of life patients with BPH using the IPSS instrument in male patients with BPH under tertiary care.
This study has evaluated changes in symptoms and QoL in a large cohort of patients with LUTS/BPH managed in conditions of real-life practice. We observed significant improvements in interested in learning about a minimally invasive option that could allow you to discontinue your BPH medications.
A relevant contribution of this study is that is assesses the effect on QoL of several medical treatments for LUTS/BPH used in real life practice by means of an internationally recognized, validated questionnaire that is easy to use in regular clinical practice, whereas earlier studies tended to focus almost exclusively on symptoms [16] [17] [18] or on outcomes associated with a single drug [19] [20]. In the present study, treatment regimens were chosen by participating urologists based on their current practice, and the distribution of patients across different pharmacological options is in line with data published in a previous report [18] [21].
![]()
Table 3. Quality of life and IPSS assessment.
![]()
Table 4. Quality of life and IPSS assessment test statisticsa,b.
a. Kruskal Wallis Test; b. Grouping variable.
![]()
Table 5. Quality of life and IPSS assessment.
In item-total correlation testing, the symptom-related item of nocturia and incomplete emptying feeling had a poor correlation. The results suggest that this item is being measured in a related yet slightly different domain than the other items of the IPSS. This result isn’t similar to that of a previous validation study carried in Brazil [19].
Some studies have already demonstrated an association between nocturia and poorer HRQoL in men with BPH. Van Dijk et al. [19] reported that among the symptoms assessed by the IPSS questionnaire, nocturia, urgency and weak stream associated with poorer QoL. Storage symptoms such as urgency, increased frequency, and nocturia reportedly have a greater impact on QoL than voiding symptoms [20]. In our study, nocturia (20% were three times, 24% four times and 17% five or more times), frequency (23% were Less than half the time, 15% about half the time and 25% more than half the time) and incomplete emptying (23% were less than half the time, 22% about half the time and more than half the time were 12%), had a negative impact on the QoL in men with BPH.
In this study the patient’s classification according to IPSS showed that most of them 52% experienced severe symptoms, 41% had moderate symptoms and only 7% had mild symptoms. Comparing the three levels of IPSS and the quality of life of patients with HBP and LUTS, when asked how you would feel if you still had problems with urination, 22% said they would feel upset, analyzing the categorization of patients according to IPSS: Mild symptoms were: Mean/SD (1.71. ± 1.113), moderate symptoms (2.9 ± 1.49) and severe symptoms (4.31 ± 1.27) p < 0.156. The statistical reliability of 64% p < 0.000 was in patients where they were interested in learning about any invasive option that would allow them to discontinue medication for LUTS.
A study was done in Nigeria [22] to determine the value of IPSS in the management of patients with BPH. Using pre-treatment IPSS, patients were divided into 3 groups: mild, moderate, and severe symptoms groups. Patients with mild symptoms were treated with careful observation and waiting as a mode of management. The moderate symptoms group received doxazosin (a-blocker) & antimuscarinics, while the severe symptoms group was treated by prostatectomy. The positive predictive value (PPV) of post treatment symptoms improvement was found out to be 87% for the severe group and 52% for the moderate group as measured by IPSS/QOL [23]. The study concluded that IPSS is a valuable tool in management of patients with BPH.
Limitations
Subjects in the present study were only recruited by a convenience sampling in Urology Clinic. The psychometric performance of these measures should be further tested with Albania speakers of different nationalities as all subjects in this study were knew Albanian speakers.
6. Conclusion
The results demonstrate that IPSS is reliable, shows responsiveness, and has constructive validity. The IPSS is a valid instrument to assess the impact of BPH symptoms on health and quality of life due to urinary symptoms.
This assessment measures the quality of life of living with benign prostatic hyperplasia according to the IPSS scale classification.
Appendix