To Prevent and Handle Positional Deformational Skull Asymmetry in Infants
—A Survey on Child Health Care Nurses and Parents’ Perception of the Given Information ()
1. Introduction
Since the beginning of 1990 parents have been recommended to let their infants sleep in supine, this has successfully decreased sudden infant death [1]. At the same time positional plagiocephaly and brachycephaly in infants have become a common problem [2] [3] [4]. The incidence of plagiocephaly was very low before 1990 and now an incidence of 46.6% is reported for infants aged 7 to 12 weeks. For most of the infants (78.3%) it was a mild form of plagiocephaly [5]. The main contributory factor in developing positional plagiocephaly and brachycephaly is that infants spend a lot of time in a supine position nowadays [6] [7] [8]. Congenital muscular torticollis (CMT) is a common musculoskeletal abnormality in infants [9]. Due to the positional preference there is a high risk that infants with CMT develop positional plagiocephaly [7] [10] [11] [12]. CMT is a result of shortening or excessive contraction of the sternocleidomastoid (SCM) muscle with limited range of motion (ROM) in both rotation and lateral flexion in the neck and an imbalance in muscle function around the neck [13] [14] [15]. Infants with plagiocephaly and brachycephaly with or without CMT are often referred to physical therapy [16]. Some parents express their dissatisfaction with getting too little or unclear information from health care professionals they meet at Health Care centres. All healthy infants in Sweden attend the Health Care Centre, for check-up, advice etc.
The aim of this study was to find out if there is a discrepancy between the parents and the nurses’ perception of what information is given, and if this information is enough.
The ethical board approved the study as long as no infant/family could be identified. This was fulfilled as all answers were left in an enclosed envelope, with no names or other identifications.
2. Method
A survey was constructed with questions about information and knowledge about prevention and treatment of plagiocephaly and brachycephaly. Consentaneous questions were made for parents and nurses. The questions were established from a long experience of parents complaining about the lack of information. The survey consisted of eleven similar questions about prevention, with options to answer totally agree, agree partly, disagree partly or totally disagree. Questions about recommended tummy time, and how often the head shape were checked was given to both parents and nurses. Questions were given to the parents about their infants head shape, head control, turning, tummy time, age when starting with tummy time. The parents also got nine questions about information given at maternity hospital. For parents with an infant with plagiocephaly or brachycephaly there were also five extra questions to answer with the alternatives totally agree, agree partly, disagree partly, or totally disagree. They were also asked about referral to paediatrician or physiotherapist and if the infant had or had had torticollis. The nurses had eight questions to answer about how to advice/treat plagiocephaly and brachycephaly to be answered with totally agree, agree partly, disagree partly, or totally disagree. Also descriptive data as age of infants, parents and nurses, how long the nurses had worked at the health care centres, parents education level etc. The survey was tested in a pilot study at another location and after that it was distributed to three regions in west Sweden. Parents and nurses were given written information about the study and were asked to participate. An assistant therapist contacted the Health Care Centres and distributed and collected the survey. All Health Care Centres in reasonable distance in Vastra Gotaland and Halland were contacted. The nurses that chosen to participate, administrated the survey to the parents
Statistics
For demographic data descriptive statistics were used, as median and range. For analysis of this and also the distribution of the different alternatives in each question, MS Excel was used.
To compare the independent samples (parents and nurses) Chi-2 test/analysis for categorical variables. P values of less than 0.05 were considered statistically significant (two-tailed test). The analysis of the data was performed with R version 3.2.2 (The R Foundation for Statistical Computing).
3. Result
The participants included 416 families and 118 nurses from three different regions in west Sweden. The infant’s median age at time of the survey was 5 months (0.3 to 60 months), 169 were female, 203 male and parents to 43 infants chose not to answer the question about gender, one family answered female and male, this is interpreted as twins. If the 43 who did not answer about gender had twins is unknown.
The nurses median age was 47 years (32 - 68 years), 16 of them had a masters degree, one was a midwife, 48 were children’s nurses, 61 district nurses, four were both district and children’s nurses, five did not answer this question. The nurses had worked at Health Care Centres for 0.25 to 40 years and been practicing from 1 to 46 years. There was no difference in the answers from the children’s nurses compared with the district nurses.
For some questions the parent’s answer differed significantly from the nurse’s answers; this is about got-given information to prevent flat head (P < 0.0001) (Figure 1), got-given information at an optimal time (P < 0.0001) (Figure 2) and information about how to handle the infant with a flat head (P < 0.0001) (Figure 3). Easiness to give and achieve information also had a discrepancy of the parents 16% disagreed and only 4% of the nurses disagreed.
The recommendations about tummy time varied from 0 to >21 minutes/day, only 55% of the parents perceived that they had got information about specific times; other recommendations were “as often as possible” or “several occasions each day” or no information. Only 5.3% got specific recommendation about more than 21 minutes (Figure 4). About tummy time occasions each day 67.1% had got recommendations ranging from 1 to >5 occasions each day, 21.6% got the recommendation >5 times a day (Figure 5). Of the parents 29% stated that they were recommended to start tummy time when the infant was newborn,
![]()
Figure 1. Distribution of the answers, nurses and parents, about got-given information, question A.
![]()
Figure 2. Distribution of the answers, nurses and parents, about the time when got-given information, question C.
![]()
Figure 3. Distribution of the answers, nurses and parents about got-given information when the child has a flat head, question M.
![]()
Figure 4. Parents perceived recommendations about minutes of daily tummy time.
42% at the age of one to two months, 29% stated later or not given specific advice (Figure 6). Parents had started with tummy time when their infant was at mean one month of age, the range was newborn to 4.5 months of age. About half (56%) stated that they had tummy time five times a day.
For 142 (34%) of the infants the parents stated that the head shape had been flat or skewed. At the time of the survey 19.6% did not have a good head shape according to the parents. The infant’s age ranged from 0.3 to 60 months. Both parents and nurses think that it is important to prevent developmental plagiocephaly and brachycephaly; totally agree 91% resp. 94%, only 2% of the parents partly disagreed and no nurses disagreed. Of the infants that were younger than six months of age 92% always slept in supine, 6% partly slept in supine, and 2% slept less often in supine. 99% of the nurses totally agreed that they recommended infants to sleep in supine, only one partly agreed. 22% of the parents stated that their infant’s head shape had been evaluated by the nurse only once or not at all.
Parents to 27 infants (6.5%) noted that their infant had or have had torticollis.
Information about preventing flat head at maternity hospital was according to 25% of the parents good enough, 19% disagreed partly and 45% totally disagreed with this question.
![]()
Figure 5. Parents perceived advice about the number of tummy time occasions each day.
![]()
Figure 6. Distribution of the answers, nurses and parents, about when they got-given advice about starting tummy time.
4. Discussion
Both parents and nurses thought that it is important to minimize the risk of developmental plagiocephaly/brachycephaly. Well-educated and motivated nurses together with clear routines are probably the best “weapon” against developmental plagiocephaly/brachycephaly. At the Health Care Centres the nurses met the infants and parents regularly, and with good routines it should improve i.e. prevent and decrease developmental plagiocephaly/brachycephaly. Research supports early information, preferably when the infant is newborn or during the first weeks of life [17]. A combination of spoken and written information is considered to be best [18]. The recommendation for how often and how long tummy time should be performed is often indefinite and can be interpreted different by different parents. “Many times a day”, “often”, “several times a day” is not clear to the parents. This is supported by the study of Koren 2010 [19]. In the current study only 5.3% got specific recommendation about more than 21 minutes. There are recommendations of about 30 - 60 minutes during a day. At the meeting with the physiotherapist parents often ask, “What is often?”, “What is much?” They want to know more concrete information, they feel a little lost; and they also need concrete tips how to make their infant accept tummy time, especially if they are older and have only had brief tummy time before. In this study 21.6% got the recommendation to have tummy time > 5 times a day, this ought to be higher.
In an attempt to give parents information about importance to prevent risk for plagiocephaly and stimulate motor development by giving tummy time, a Swedish booklet “Lek på mage” (“play time-tummy time”) was put together in 2007. (http://torticollis.dinstudio.se/files/lekpamage.pdf) in English at http://torticollis.dinstudio.se/files/tummy_time._Anna_Ohman_2014.pdf) also a shorter version at https://www.1177.se/Vastra-Gotaland/Fakta-och-rad/Mer-om/Lek-pa-mage-och-sov-pa-rygg/). In USA a booklet ”Back to sleep, tummy to play” came 2008, like “Lek på mage” it contain advice about avoiding babysitter and long time in car-seats (Back to Sleep, Tummy to Play Copyright © 2008 American Academy of Pediatrics, Updated 08/2016). “Lek på mage” was updated in 2014 as the Swedish board of welfare updated the advice for prevention of sudden infant death, earlier advice to use a pillow was taken away and was not included when the updated advice was presented at the Medical National Conference, December 2013 [1]. There is no risk from the use of a pillow for a supine sleeping infant, however if the infant turns to prone there can be a risk when using a pillow [20] [21].
One possible reason for the discrepancy between the parents and nurse’s opinion on when and which information is given may be due to that there are a lot of other worries and problems for parents of new-borns. Eating, sleeping and other health issues take a lot of the time when parents met the nurse at the Health Care Centre. And also, parents may not understand the importance of all information, they may believe that there only is a small or marginal risk for developmental plagiocephaly/brachycephaly. It is important for health care professionals to be aware that we do not reach everybody, but we need to try our best. To reach 100% is probably utopia; however, to understand the communication problem may help us to put together better information, and better routines. Zachry study showed that 75% of parents took in the information about putting infants on the back to sleep and play on tummy, but of these only three quarters understood the reason for it [22]. Hypothetically in the current study it would mean that 233 of 414 probably were able to take in the information and understand it.
At the time of the survey 19.6% answered that their infant had a skewed or flat head. Some infants were still very young at the time of the survey and this cannot be seen as a final outcome of their head shape. The incidence of skewed or flat head in this study was 34%, this is within the range of incidence found in other studies [5].
The result shows that there is a need for clear routines, more information material and higher awareness and knowledge. Parents need to get education, given by health care nurses and physicians for prevention to be effective [18] [23] [24] [25] [26] [27]. The ideal time to inform parents about prevention of developmental plagiocephaly/brachycephaly is when the infant is new-born [18]. To give both spoken and written information has shown to be the most effective [28]. To follow up on the information given is important, this can be done at the meetings at the Child Care Centre and can also be discussed in parents’ groups, led by a nurse. It should be clear why the information is important.
Tummy time is also important for timely motor development, e.g. to turn, crawl [26] [29] [30] [31] [32]. Infants with a late motor development can cause parent worry and also consume unnecessary resources from health care [33]. Discovery of real problems can be delayed if the infant is believed to “only be a little late in development”. Parents need to be aware that infants need opportunity to train themselves, development comes from repetition, not only with age. Some parents need to be shown in practice how to train on tummy, especially when they have waited with tummy time until the infant is a little older.
There were 43 families that did not answer the question about gender; it is likely that at least some of them were twins, probably a majority as we see many twins in the clinical settings. One option is also that some parents found the question about gender of non-importance. However, in the survey there ought to have been an alternative to choose twins as twins are more common these days because of fertility treatments [34] [35]. To be a twin is also considered a risk factor for plagiocefali/brachycefali [36].
5. Conclusions from the Survey
Both the nurses and the parents state that it is important to prevent deformational plagiocephaly/brachycephaly. There is disagreement in when and in what magnitude the information is given. Parents experience that the information is unclear and is often given late. The nurses felt less confident in giving advice when the plagiocephaly/brachycephaly already had developed. The answers in the survey indicate that routines, information and advice need to improve.
After the survey a working group was set up to give suggestions about routines (Appendix A), information, advice and guidelines for the nurses (Appendix B).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Appendix A
Appendix B
Guidelines for Examination of Plagiocephaly/Brachycephaly 2017
Does the infant have a favourite side?
Ask the parents if their infant often has the head in the same position when beeing in supine; to the left/right, always in neutral position or often stays turned to one of the parents.
Put the infant on the examination couch and see how the infant acts with her/his head. Notice if it is hard to make the infant look in another direction or if it has difficulties to keep the head in neutral position.
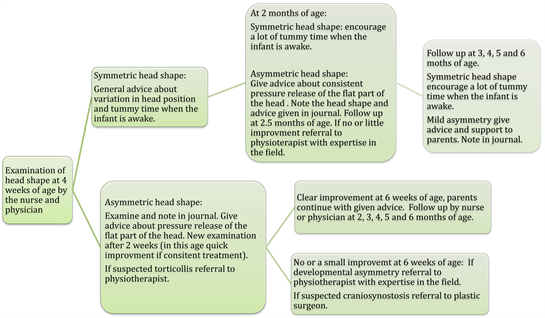
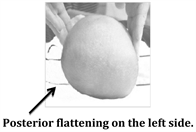
Examination the shape of the head
Put the infant on the parent’s lap with the infant facing the parent or put the infant on the examination couch bench in a supine position, the head directed towards the examiner. Use the infants nose as a marker, put your fingers around the forehead and at the back of the head, look and feel if there is asymmetry.If the infant has a lot of hair it can camouflage asymmetry, cow’s lick can fool the eye.
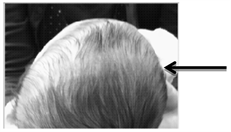
NB! Flat spots occur where the infant has rubbed the hair away. These can be a sign that that side of the head is flatter but is not reliable.
Some infants rub the hair away on the rounder side and stay put on the flat side.
Brachycephaly. Can be everything from minor to severe, a minor brachycephaly can increase to severe fast if the infant at an age of 0 - 3 months.

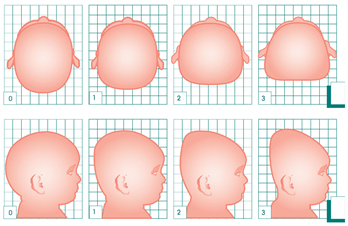
Bulging forehead right side.

Bulging forehead left side.

Asymmetry of the ears. The ear is forward
on the same side as the posterior flattening. If the opposite there is need to exclude Craniosynostosis.
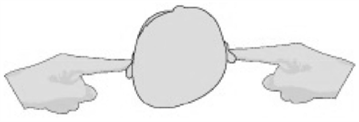
Temporal asymmetry. E.g. when one side is concave
Temporal bulging left side.
Temporal bulging right side.
Cranial Tech scales can be used to estimate plagiocephaly and brachycephaly.
0 = no asymmetry, 1 = mild asymmetry, 2 = moderate asymmetry, 3 = severe asymmetry.
It can be an advantage to also use half scores, one study showed good reliability for this e.g. between 1 - 2 (1.5).
Plagiocefali

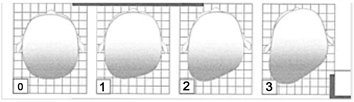
Brachycephaly

The severity assessment Scale is used with permission by Tim Littlefield, Cranial Tech. Tim was asked by Anna Öhman 2016.
Information/Advice to give
More tummy time when the infant is awake, 60 - 90 minutes a day as a goal. Start with a few minutes and gradually increase the time.
Avoid prone position when the infant is awake.
Avoid time by the infant spend on the flat part of the head.
Avoid car safety seat outside the car.
Avoid baby carrier or minimize the time in it.
If/when using baby carrier put it so all interesting things are on the opposite side to the infants favoured side.
Recommend side device, if the infant stays good on the side, this can be the most effective way to get a better head shape. Use it when you can check on your infant, when the infant can turn over to tummy stop using the side device.
If the infant is >6 months of age, healthy and can turn by itself, the infant can sleep in any position it chooses including on the tummy.
Recommend a special pillow (at present the Mimosbreathable pillow February 2017) if the infant stays in neutral position only and it is not possible to make it change sides of the head.
Need for referral
To physiotherapist when suspected torticollis or need for help with plagiocephaly/brachycephaly. In Sweden parents can make their own referral to the physiotherapist. Referral to Craniofacial department in Gothenburg if suspected craniosynostosis. Families living in VG-region (the South West region of Sweden) can send own referrals.
It is also possible for Health Care staff in Sweden to send photos to the Craniofacial department for assessment. Be sure that the photo shows what you see, the angle of the photo can give different results.
Follow up
It is important to know that infant head shape can change the first year of life. It can be harder and take longer time for an older infant, but it is not impossible.
When the infant has achieved a symmetrical head shape it is important to vary the position to maintain the symmetry. Otherwise there is a risk of developing plagiocephaly/brachycephaly again.
For the young infants (0 - 3 months) the head shape can change very quickly. It is important to vary and observe to maintain the symmetric shape.
TORTICOLLIS
Does the infant side bend (tilt) the head to one side.
No remace Infant holds head straight
Infant side bend (tilt) the head to the right. Infant tilt the head with the right ear towards the right shoulder.
Infant side bend (tilt) the head to the left. Infant tilt the head with the left ear towards the left shoulder.
Suspected limitation of head rotation. Infant seem to have a problem to rotate the head to left or right
Suspected asymmetry muscle function/strength of the neck. Hold the infant in a horizontal position with both left and right side up, if there is an obvious difference you can see it.
Referral to physiotherapist when suspected torticollis.
There is evidence that early start of treatment gives shorter treatment time.