International Journal of Clinical Medicine
Vol.2 No.4(2011), Article ID:7551,7 pages DOI:10.4236/ijcm.2011.24069
Fluctuation of Corrected Serum Calcium Levels Following Partial and Total Thyroidectomy
![]()
Department of Otolaryngology-Head & Neck Surgery, North Manchester General Hospital, Pennine Acute Hospitals NHS Foundation Trust, Manchester, United Kingdom.
Email: prad.murthy@pat.nhs.uk
Received February 27th, 2011; revised April 11th, 2011; accepted July 20th, 2011.
Keywords: Thyroidectomy, Hypocalcaemia, Parathyroid Glands, Peripheral Receptors
ABSTRACT
Objectives: To identify any fluctuation of corrected serum calcium levels and to determine the presence of sub-clinical hypocalcaemia following partial and total thyroidectomy with preservation of at least two parathyroid glands. Design: A prospective study. Setting: Tertiary Head & Neck referral unit. Patients: Eighty five patients undergoing partial or total thyroidectomy with or without laryngectomy from April 2003 to April 2009 were included in the study. Corrected serum calcium levels (CCSL) were noted preoperatively and postoperatively on day 1, day 7 and 6 months. Results: Forty six patients underwent hemi-thyroidectomy (HT), 29 underwent total thyroidectomy (TT) and 10 underwent total thyroidectomy with laryngectomy (TTL). Nine (19.56%) patients in the HT group, 6 (24.14%) in the TT group and 3 (30.0%) in the TTL group developed hypocalcaemia postoperatively which was most significant on 1st postoperative day. This improved by 7th postoperative day in each group when the change in calcium levels became statistically insignificant. Six patients (3 patients had HT, 2 had TT and 1 had TTL) developed sub-clinical mild hypocalcaemia which was persistent at 6 months follow-up. Conclusion: The most significant changes in corrected serum calcium levels occur within first 24 hours after thyroid surgery. Thereafter most patients return to normocalcaemia within a seven-day period. Despite preservation of parathyroid glands there is a subgroup of patients who develop sub-clinical hypocalcaemia which persists even at six months but does not require treatment.
1. Introduction
Calcium regulation is critical for normal cell function, neural transmission, membrane stability, bone structure, blood coagulation, and intracellular signalling. Unrecognised or poorly treated hypocalcaemia can lead to significant morbidity or death. Approximately 99% of calcium is found in bone, and 1% is found in extra-cellular fluid. Of this extra-cellular calcium, 50% is in the free (active) ionized form (1 mmol/L - 1.15 mmol/L), 40% is bound to protein (predominantly albumin), and 10% is complexed with anions (e.g. citrate). It is this 1% extra-cellular calcium that is essential for normal physiological function.
Early changes in the extra-cellular serum calcium levels after thyroid surgery leading to hypocalcaemia have frequently been reported [1-5]. The exact cause of transient and permanent hypocalcaemia post thyroidectomy is multi-factorial and has been linked to 1) hypoparathyroidism caused by iatrogenic damage to the parathyroid glands or their blood supply, 2) haemodilution, 3) hypoalbuminaemia, and 4) changes in peripheral sensitivity to parathyroid hormone.
Numerous studies have attempted to identify risk factors that will predict those patients who will become severely hypocalcaemic post surgery thereby preventing significant morbidity and mortality [6-11]. In the last two decades few groups have examined the influence of partial and total thyroidectomy on fluctuation of CSCL over a long term period.
The aim of this paper is to identify the fluctuation of CSCL over a six month period after thyroid surgery as well as to highlight the presence of sub-clinical hypocalcaemia despite preservation of parathyroid glands (PTG) and their blood supply.
2. Method
2.1. Patients
This is a prospective study of patients undergoing partial or total thyroidectomy with or without laryngectomy from April 2003 to April 2009. For analysis the patients were divided into three groups: 1) patient who underwent hemi-thyroidectomy, 2) patients who underwent total thyroidectomy, and 3) patients who underwent total thyroidectomy with laryngectomy.
2.2. Surgery
The surgery of all cases included in the study was performed by the senior author to remove operator bias. Methylene blue dye was not infused prior to surgery in any patient. A standard approach was employed with an incision two finger breadths above the clavicle. Subplatysmal flaps were raised, the strap muscles retracted and the thyroid gland exposed. The middle thyroid vein was ligated and the lobes of the thyroid mobilised medially. The superior and inferior thyroid arteries were identified together with recurrent laryngeal nerve (RLN). Meticulous haemostasis was maintained and inferior parathyroid glands visually identified on the posterolateral border of the thyroid above the level where the inferior thyroid artery crosses the RLN. The superior thyroid artery was ligated adjacent to the thyroid capsule. In order to preserve the parathyroid glands, extra-capsular dissection was performed and inferior thyroid artery ligated distal to branches to inferior parathyroid gland. The superior parathyroid glands were identified adjacent to the upper pole of the respective lobes. The parathyroid glands were identified and preserved in a similar manner when thyroid gland was resected in patients undergoing laryngectomy.
2.3. Data Recording and Analysis
Patients who did not have calcium levels done either preoperatively or postoperatively on day 1, day 7 and 6 months were excluded from the study. In addition, patients who were taking pre-operative calcium supplementation and those that required immediate post-operative intravenous or oral calcium supplementation due to symptoms of hypocalcaemia were excluded from the study. All the patients had a CSCL of >1.90 mmol/L preoperatively.
Corrected serum calcium level (CSCL) was noted preoperatively and on day 1, day 7 and 6 months postoperatively. The number of patients in each group that were normocalcaemia (2.65 mmol/L - 2.12 mmol/L), mildly hypocalcaemia (2.11 mmol/L - 2.00 mmol/L), moderately hypocalcaemia (1.99 mmol/L - 1.91 mmol/L) and severely hypocalcaemia (<1.91 mmol/L) was noted.
The mean difference in CSCL between each subgroup was analysed using a paired t-test (Statsdirect® version 2.3.3) in order to demonstrate a significant change (p < 0.05) between the preoperative levels and postoperative levels.
3. Results
A total of 120 patients were enrolled in the study. Of these, 85 patients met the inclusion criteria and had complete recording of data and were hence included in the study. There were 57 females and 28 males. The mean age was 46 years (range 37 - 68 years).
3.1. Hemi-Thyroidectomy Group
There were 46 patients in this group. Nine (19.56%) patients in this group developed hypocalcaemia postoperatively on day 1 (p = 0.001, SD = 0.12) and 1 patient who was mildly hypocalcaemia preoperatively became severely hypocalcaemic postoperatively (Figure 1). All the patients were asymptomatic and did not require calcium supplementation. As per our departmental policy we start postoperative calcium supplementation if a patient develops symptoms of hypocalcaemia or if corrected serum calcium level is <1.8 mmol/L.
Calcium levels improved by day 7 when only 3 (6.52%) patients had hypocalcaemia (p = 0.02, SD = 0.1) including the one patient who developed severe hypocalcaemia. Mild hypocalcaemia persisted in 3 patients at 6 months postoperatively (p = 0.9, SD = 0.14) (Table 1). This included the single patient who had developed severe hypocalcaemia at day 7. These 3 patients were followed up for 6 months postoperatively and continued to be hypocalcaemic but remained asymptomatic and hence were discharged.
3.2. Total Thyroidectomy Group
There were 29 patients in this group. Six (24.14%) patients in this group developed hypocalcaemia postoperatively on day 1 (p < 0.001, SD = 0.1) and 1 patient who was mildly hypocalcaemia in the preoperative period became moderately hypocalcaemic postoperatively (Figure 2). All the patients were asymptomatic and did not require calcium supplementation. By the 7th postoperative day, 5 (17.24%) patients had hypocalcaemia (p = 0.22, SD = 0.15). Mild hypocalcaemia persisted in 2 patients at the 6 months assessment (p = 0.7, SD = 0.07) (Table 2). These patients were followed up for 6 months and continued to be hypocalcaemic but remained asymptomatic and were hence discharged.
3.3. Total Thyroidectomy with Laryngectomy Group
There were 10 patients in this group. Three (30%) patients in this group developed hypocalcaemia postoperatively on day 1 (p < 0.003, SD = 0.1). Of these, 1 patient who had mild hypocalcaemia and another who had moderate hypocalcaemia in the preoperative period became severely hypocalcaemic postoperatively (Figure 3). How-
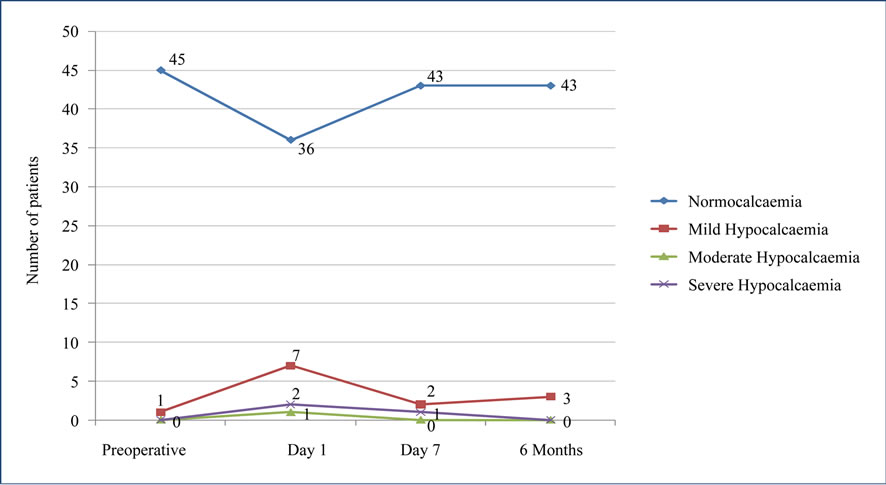
Figure 1. Pre-op and post-op calcium levels in hemi-thyroidectomy group (n = 46).
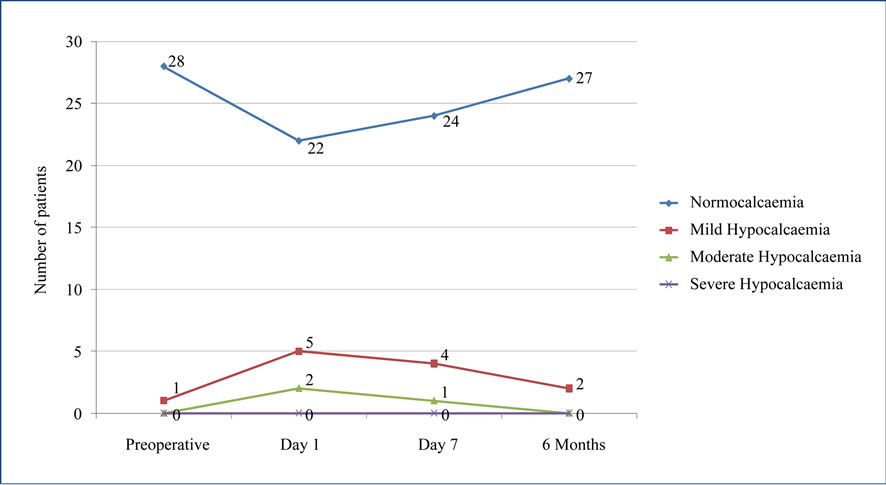
Figure 2. Pre-op and post-op calcium levels in total thyroidectomy group (n = 29).

Table 1. Statistical difference in calcium levels pre/post operative in hemi-thyroidectomy group.
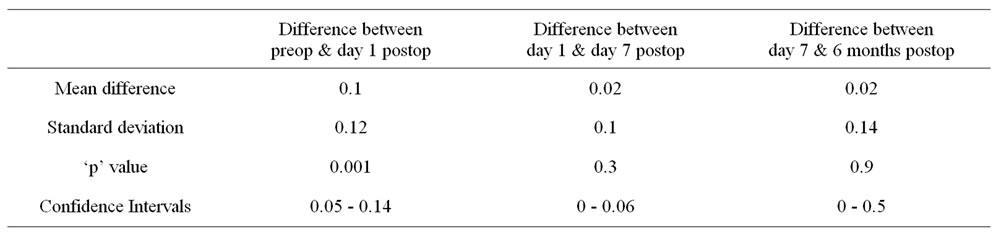
Table 2. Statistical difference in calcium levels pre/post operative in total thyroidectomy group.

Figure 3. Pre-op and post-op calcium levels in total thyroidectomy with laryngectomy group.
ever, all the patients were asymptomatic and did not require calcium supplementation. By the 7th postoperative day, 2 (20%) patients had mild hypocalcaemia (p = 0.1, SD = 0.1). Mild hypocalcaemia persisted in 1 patient at the 6 months assessment (p = 0.3, SD = 0.01) (Table 3). This patient remained asymptomatic and was discharged at this period.
4. Discussion
Hypocalcaemia following thyroid surgery is more commonly associated with total thyroidectomy particularly for malignant lesions, thyroidectomy along with laryngectomy and thyroidectomy in younger patients [12,13]. The patho-physiology has been linked to hypoparathyroidism, haemodilution, hypoalbuminaemia, and changes in peripheral sensitivity to parathyroid hormone. Its association with the removal of the parathyroid glands (PTGs) or disruption of the blood supply to the PTG is still debatable [14-18]. Similarly auto-transplantation of the PTG at the time of surgery also is open to further research but it does seem to serve a role in preventing hypocalcaemia [19].
Permanent hypocalcaemia requiring long-term supplementation has been well reported following thyroid surgery [1-5]. Numerous studies have been performed examining serum calcium, magnesium and phosphorous levels as well as levels of 1.25 dihydroxycholecalciferol, parathyroid hormone & calcitonin in order to determine which factors will predict those individuals who will become severely hypocalcaemic in the post-operative period [1-5,12,13] thus preventing significant morbidity.
To our knowledge there are few studies that determine the mid-term fluctuation of corrected serum calcium levels and exclude the presence of sub-clinical hypocalcaemia following thyroid surgery with preservation of parathyroid glands. In our study we have analysed the CSCL in three different groups of patients; those undergoing hemi-thyroidectomy (HT), total thyroidectomy (TT) and total thyroidectomy with laryngectomy (TTL) over period of 6 months. In order to remove variability all surgery was performed by the senior author and every effort was made to identify and carefully preserve at least two
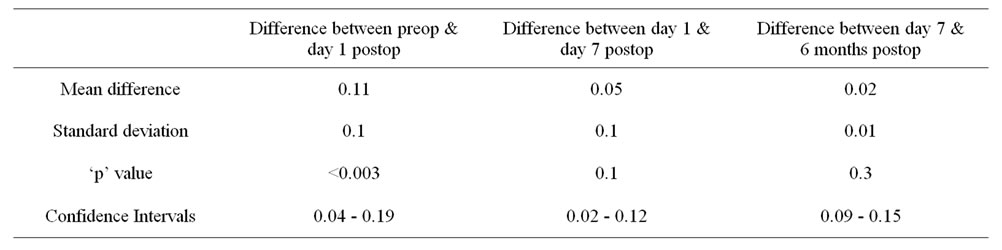
Table 3. Statistical difference in calcium levels pre/post operative in laryngectomy with total thyroidectomy group.
of the PTGs and their vascular supply in all cases including when hemithyroidectomy was carried out. Identification of the PTGs was carried out based on appearance—being tan to brown, pea sized and close to the thyroid capsule—as well as location, the superior PTG usually being located at the border of the middle and upper thirds of the thyroid gland posteriorly, near the cricothyroid joint and the inferior PTG lying near the junction of the recurrent laryngeal nerve and the inferior thyroid artery posteriorly. Meticulous dissection with preservation of the PTGs will minimize the possibility of transient postoperative hypoparathyroidism in situations where the hypocalcaemia can be clearly attributed to this condition. Following excision of the thyroid lobe, the wellbeing of the PTG was confirmed by ensuring that the gland retained it’s tan colour and remained attached to it’s vascular pedicle. If a gland was noted to be devitalized, it was minced into 1 mm pieces and re-implanted into multiple pockets created in the ipsilateral sternomastoid muscle.
From our research, we found that the most significant fluctuation of CSCL occurred within first 24 hours postoperatively. The fluctuation was maximum in patients undergoing total thyroidectomy (fluctuation = 0.18 mmol/L, p < 0.001), followed by patients who had total thyroidectomy along with laryngectomy (fluctuation = 0.11 mmol/L, p < 0.003) and hemi-thyroidectomy (fluctuation = 0.1 mmol/L, p = 0.001). The cause for the transient drop in serum calcium in patients who underwent total thyroidectomy is more readily ascertained on the basis of the preserved parathyroid tissue taking a few days to recover from the trauma of surgical dissection which produces temporary parathyroid insufficiency before resuming normal function. Whilst some surgeons routinely give calcium supplementation after total thyroidectomy to facilitate early discharge from hospital and to eliminate the need for phlebotomy several times in the postoperative period, our practice is to treat this mild hypocalcaemia only if it is symptomatic (positive Trosseau’s or Chvostek’s sign, cardiac arrhythmia, tingling around the lips) and in our experience this usually tends to occur when the corrected serum calcium falls below 1.85 mmol/L. Despite there being no significant difference in CSCL over the medium term in each group, 3 patients (6.52%) who underwent hemi-thyroidectomy, 2 patients (6.89%) who underwent total thyroidectomy and 1 patient (10%) who had total thyroidectomy with laryngectomy had mild sub-clinical hypocalcaemia at 6 months postoperatively. We acknowledge that numbers in each group are too small to be of statistical significance but awareness needs to be drawn to the fact that sub-clinical hypoparathyroidism does occasionally occur after thyroid surgery and may need to be monitored for the few months following surgery in case these patients need to be commenced on replacement therapy particularly if they become symptomatic. Surprisingly, our results have shown that it also occurs in patients who underwent hemi-thyroidectomy whose parathyroid glands and their blood supply were not disturbed on the opposite non-operated side. In these patients, there will be a modest decrease in total serum calcium levels with little or no change to the free or ionized calcium. The nonspecific release of ADH caused by surgical stress also results in the serum albumin becoming haemodiluted which in turn affects the total serum calcium which is bound to albumin. However, as it is the free unbound calcium which brings about physiologic effects, these patients remain asymptomatic. This transient reduction in serum albumin levels seen in patients who have undergone hemithyroidectomy is expected to a greater extent after total thyroidectomy. Unlike patients who undergo unilateral surgery, significant reductions in free or ionized calcium levels are seen in patients after total thyroidectomy. This is likely to be another cause of transient hypoparathyroidism resulting in temporary hypocalcaemia in addition to possible iatrogenic injury to the PTGs and their vascular supply.
It appears that calcium homeostasis following thyroid surgery is a complex problem and is not only related to iatrogenic damage to the parathyroid gland and/or its blood supply leading to hypoparathyroidism but also to possible changes in the calcium sensing receptors. These are G-coupled receptors found not only in parathyroid glands but also in kidneys, bones, intestine and various other organs responsible for calcium homeostasis. Functionally mutations in the receptor have been shown to induce diseases of calcium homeostasis owing to changes in the set point for calcium-regulated parathyroid hormone release as well as alterations in the renal handling of calcium. It has been shown that gain-of-function mutations cause hypocalcaemia [20-22]. We hypothesise a similar mutation following certain thyroid diseases causing sub-clinical hypocalcaemia despite the preservation of parathyroid glands. Further molecular research into the calcium G-receptors after thyroid surgery needs to be considered in the future.
5. Conclusions
The most significant changes in CSCL occur within the first 24 hours after thyroid surgery and thereafter most patients return to normocalcaemia within a seven day period and do not require further monitoring unless clinically indicated. There is however a small group of patients that despite meticulous preservation of the parathyroid glands and its blood supply develop postoperative sub-clinical hypocalcaemia which persists even after six months but do not require treatment. It appears that calcium homeostasis in this sub-group is a complex problem and is not only related to parathyroid gland function but also to possible changes in peripheral calcium receptors.
In future a larger group of patients undergoing hemithyroidectomy will need to be studied in order to determine the true incidence of this problem. In addition to this, the effects of thyroid disease, surgery on parathyroid glands and the role of peripheral calcium receptors also need to be considered.
REFERENCES
- N. Mehta, N. B. Watts, J. A. Welge and D. Steward, “Comparison of Serum Calcium Change Following Thyroid and Non-Thyroid Neck Surgery,” Otolaryngology— Head and Neck Surgery, Vol. 134, No. 6, 2006, pp. 901-906.
- C. Bourell, B. Uzzan, G. Y. Perret, et al., “Transient Hypocalcaemia after Thyroidectomy,” Annals of Otology, Rhinology and Laryngology, Vol. 102, No. 7, 1993, pp. 496-501.
- P. Lindblom, J. Westerdahl and A. Bergenfelz, “Hemithyroidectomy: Long Term Effects on Parathyroid Function a Preliminary Report,” World Journal of Surgery, Vol. 25, No. 9, 2001, pp. 1155-1159. doi:10.1007/BF03215864
- A. Bergenfelz and B. Ahren, “Calcium Metabolism after Hemithyroidectomy,” Hormone Research, Vol. 39, No. 1-2, 1993, pp. 56-60. doi:10.1159/000182696
- E. Eforakopoulou-Gialakidou, D. A. Koutras, S. D. Moulopoulos, et al., “Thyroid and Parathyroid Response to Subtotal Thyroidectomy,” Endocrinologia Experimentalis, Vol. 22, No. 3, 1988, pp. 165-169.
- T. Meyer, S. Merkel, W. Hohenberger, et al., “Dysfunction of Calcium Metabolism Following Resection of the Thyroid Gland. An Analysis of important Risk Factors,” Zentralblatt fur Chirurgie, Vol. 127, No. 5, 2002, pp. 429-434. doi:10.1055/s-2002-31972
- P. Del Rio, M. F. Arcuri, M. Sianesi, et al., “The Utility of Serum PTH Assessment 24 Hours after Total Thyroidectomy,” Otolaryngology—Head & Neck Surgery, Vol. 132, No. 4, 2005, pp. 584-586.
- R. M. Quiros, C. E. Pesce, R. A. Prinz, et al. “Intraoperative Parathyroid Hormone Levels in Thyroid Surgery Are Predictive of Postoperative Hypoparathyroidism and Need for Vitamin D Supplementation,” American Journal of Surgery, Vol. 189, No. 3, 2005, pp. 306-309. doi:10.1016/j.amjsurg.2005.01.006
- A. Lam and P. D. Kerr, “Parathyroid Hormone: An Early Predictor of Post Thyroidectomy Hypocalcaemia,” Laryngoscope, Vol. 113, 2003, pp. 2196-2200.
- C. P. Lombardi, M. Raffaelli, R. Bellantone, et al., “Early Prediction of Post Thyroidectomy Hypocalcaemia by One Single iPTH Measurement,” Surgery, Vol. 136, 2004, pp. 1236-1241.
- A. Vescan, I. Witterick and J. Freeman, “Parathyroid Hormone as a Predictor of Hypocalcaemia after Thyroidectomy,” Laryngoscope, Vol. 115, No. 12, 2005, pp. 2105-2108.
- R. Bellantone, C. P. Lombaedi, P. Princi, et al., “Is Routine Supplementation Therapy (Calcium and Vitamin D) Useful after Total Thyroidectomy?” Surgery, Vol. 132, No. 6, 2002, pp. 1109-1112.
- C. R. McHenry, T. Speroff, R. A. Prinz, et al., “Risk Factors for Post-Thyroidectomy Hypocalcaemia,” Surgery, Vol. 116, No. 10, 1994, pp. 641-648.
- N. Bhattacharyya and M. P. Fried, “Assessment of the Morbidity and Complications of Total Thyroidectomy,” Archives of Otolaryngology and Head & Neck Surgery, Vol. 128, No. 4, 2002, pp. 389-392.
- C. Nies, H. Sitter, M. Rothmund, et al. “Parathyroid Function Following Ligation of the Inferior Thyroid Arteries during Bilateral Subtotal Thyroidectomy,” British Journal of Surgery, 1994, Vol. 81, No. 12, pp. 1757-1759. doi:10.1002/bjs.1800811215
- V. J. Araujo-Filho, G. B. Silva-Filho, A. R. Ferraz, et al., “The Importance of the Ligation of the Inferior Thyroid Artery in Parathyroid Function after Subtotal Thyroidectomy,” Revista do Hospital das Clínicas, Vol. 55, No. 4, 2000, pp. 113-120. doi:10.1590/S0041-87812000000400002
- M. Dolapci, M. Doganay, N. A. Kama, et al., “Truncalligation of the Inferior Thyroid Arteries Does Not Affect the Incidence of Hypocalcaemia after Thyroidectomy,” European Journal of Surgery, Vol. 166, No. 4, 2000, pp. 286-288. doi:10.1080/110241500750009096
- G. Maralcan, Z. Sayin, N. Aybasti, et al., “Does Truncal Ligation of the Inferior Thyroid Arteries during Bilateral Subtotal Thyroidectomy Affect Serum Calcium Levels?” International surgery, Vol. 91, No. 4, 2006, pp. 211-216.
- C.-Y. Lo and K.-Y. Lain, “Parathyroid Auto-Transplantation during Thyroidectomy: Is Frozen Section Necessary?” Archives of Surgery, Vol. 134, No. 3, 1999, pp. 258-260. doi:10.1001/archsurg.134.3.258
- E. M. Brown, “Physiology and Patho-Physiology of the Extra-Cellular Calcium-Sensing Receptor,” American Journal of Medicine, 1999, Vol. 106, No. 2, pp. 238-253. doi:10.1016/S0002-9343(98)00418-5
- D. A. Heath, “Clinical Manifestations of Abnormalities of the Calcium Sensing Receptor,” Clinical Endocrinology Vol. 48, No. 3, 1998, pp. 257-258.
- J. Tfelt-Hansen and E. M. Brown, “The Calcium-Sensing Receptor in Normal Physiology and Patho-Physiology,” Clinical Laboratory Sciences, Vol. 42, No. 1, 2005, pp. 35-70. doi:10.1080/10408360590886606

