S. N. ABDULLAH ET AL.
Copyright © 2011 SciRes. OJU
88
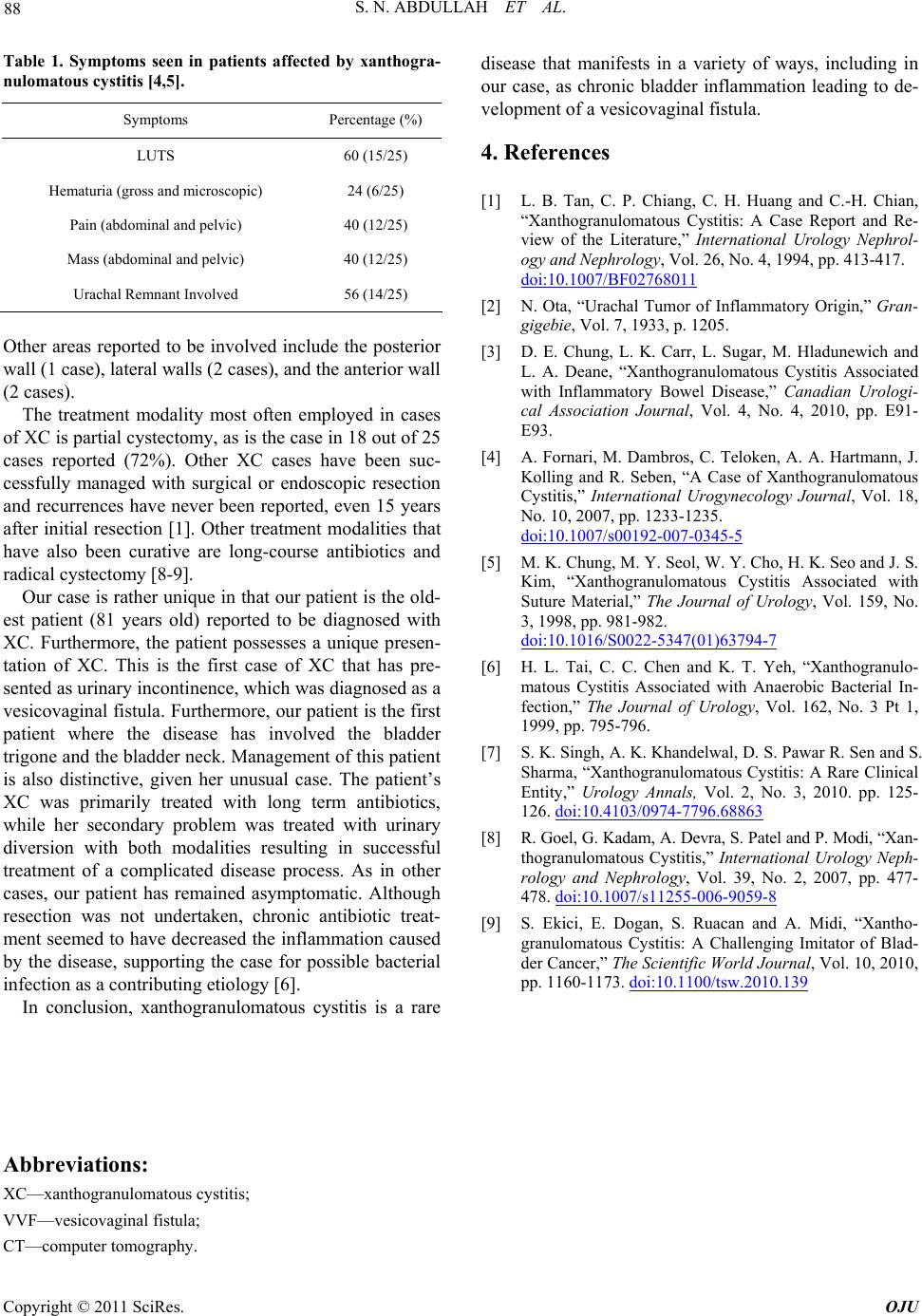
Table 1. Symptoms seen in patients affected by xanthogra-
nulomatous cystitis [4,5].
Symptoms Percentage (%)
LUTS 60 (15/25)
Hematuria (gr oss a nd microscopic) 24 (6/25)
Pain (abdominal and pelvic) 40 (12/25)
Mass (abdominal and pelvic) 40 (12/25)
Urachal Remnant Involved 56 (14/25)
Other areas reported to be involved include the posterior
wall (1 case), lateral walls (2 cases), and the anterior wall
(2 cases).
The treatment modality most often employed in cases
of XC is partial cystectomy, as is the case in 18 out of 25
cases reported (72%). Other XC cases have been suc-
cessfully managed with surgical or endoscopic resection
and recurrences have never been reported, even 15 years
after initial resection [1]. Other treatment modalities that
have also been curative are long-course antibiotics and
radical cystectomy [8-9].
Our case is rather unique in that our patient is the old-
est patient (81 years old) reported to be diagnosed with
XC. Furthermore, the patient possesses a unique presen-
tation of XC. This is the first case of XC that has pre-
sented as urinary incontinence, which was diagnosed as a
vesicovaginal fistula. Furthermore, our patient is the first
patient where the disease has involved the bladder
trigone and the bladder neck. Management of this patient
is also distinctive, given her unusual case. The patient’s
XC was primarily treated with long term antibiotics,
while her secondary problem was treated with urinary
diversion with both modalities resulting in successful
treatment of a complicated disease process. As in other
cases, our patient has remained asymptomatic. Although
resection was not undertaken, chronic antibiotic treat-
ment seemed to have decreased the inflammation caused
by the disease, supporting the case for possible bacterial
infection as a contributing etiology [6].
In conclusion, xanthogranulomatous cystitis is a rare
disease that manifests in a variety of ways, including in
our case, as chronic bladder inflammation leading to de-
velopment of a vesicovaginal fistula.
4. References
[1] L. B. Tan, C. P. Chiang, C. H. Huang and C.-H. Chian,
“Xanthogranulomatous Cystitis: A Case Report and Re-
view of the Literature,” International Urology Nephrol-
ogy and Nephrology, Vol. 26, No. 4, 1994, pp. 413-417.
doi:10.1007/BF02768011
[2] N. Ota, “Urachal Tumor of Inflammatory Origin,” Gran-
gigebie, Vol. 7, 1933, p. 1205.
[3] D. E. Chung, L. K. Carr, L. Sugar, M. Hladunewich and
L. A. Deane, “Xanthogranulomatous Cystitis Associated
with Inflammatory Bowel Disease,” Canadian Urologi-
cal Association Journal, Vol. 4, No. 4, 2010, pp. E91-
E93.
[4] A. Fornari, M. Dambros, C. Teloken, A. A. Hartmann, J.
Kolling and R. Seben, “A Case of Xanthogranulomatous
Cystitis,” International Urogynecology Journal, Vol. 18,
No. 10, 2007, pp. 1233-1235.
doi:10.1007/s00192-007-0345-5
[5] M. K. Chung, M. Y. Seol, W. Y. Cho, H. K. Seo and J. S.
Kim, “Xanthogranulomatous Cystitis Associated with
Suture Material,” The Journal of Urology, Vol. 159, No.
3, 1998, pp. 981-982.
doi:10.1016/S0022-5347(01)63794-7
[6] H. L. Tai, C. C. Chen and K. T. Yeh, “Xanthogranulo-
matous Cystitis Associated with Anaerobic Bacterial In-
fection,” The Journal of Urology, Vol. 162, No. 3 Pt 1,
1999, pp. 795-796.
[7] S. K. Singh, A. K. Khandelwal, D. S. Pawar R. Sen and S.
Sharma, “Xanthogranulomatous Cystitis: A Rare Clinical
Entity,” Urology Annals, Vol. 2, No. 3, 2010. pp. 125-
126. doi:10.4103/0974-7796.68863
[8] R. Goel, G. Kadam, A. Devra, S. Patel and P. Modi, “Xan-
thogranulomatous Cystitis,” International Urology Neph-
rology and Nephrology, Vol. 39, No. 2, 2007, pp. 477-
478. doi:10.1007/s11255-006-9059-8
[9] S. Ekici, E. Dogan, S. Ruacan and A. Midi, “Xantho-
granulomatous Cystitis: A Challenging Imitator of Blad-
der Cancer,” The Scientific World Journal, Vol. 10, 2010,
pp. 1160-1173. doi:10.1100/tsw.2010.139
Abbreviations:
XC—xanthogranulomatous cystitis;
VVF—vesicovaginal fistula;
CT—computer tomography.