J. F. BLANCO ET AL.
Copyright © 2011 SciRes. SS
129
4. Conclusions
We report a rare case of spinal osteoblastoma after sur-
gery in adjacent vertebral level. The osteoblastoma
mimic a syndrome of failed back surgery which can warn
people that a new disease (such as a tumor in this case),
irrelevant to the original one, may happen simultane-
ously even if the original one has been successfully
treated and should be differentiated from the previous
disease or surgical failure and complications.
5. References
[1] D. R. Lucas, K. K. Unni, R. A. McLeod, M. I. O’Connor
and F. H. Sim, “Osteoblastoma: Clinicopathologic Study
of 306 Cases,” Human Pathology, Vol. 25, No. 2, 1994,
pp. 117-134. doi:10.1016/0046-8177(94)90267-4
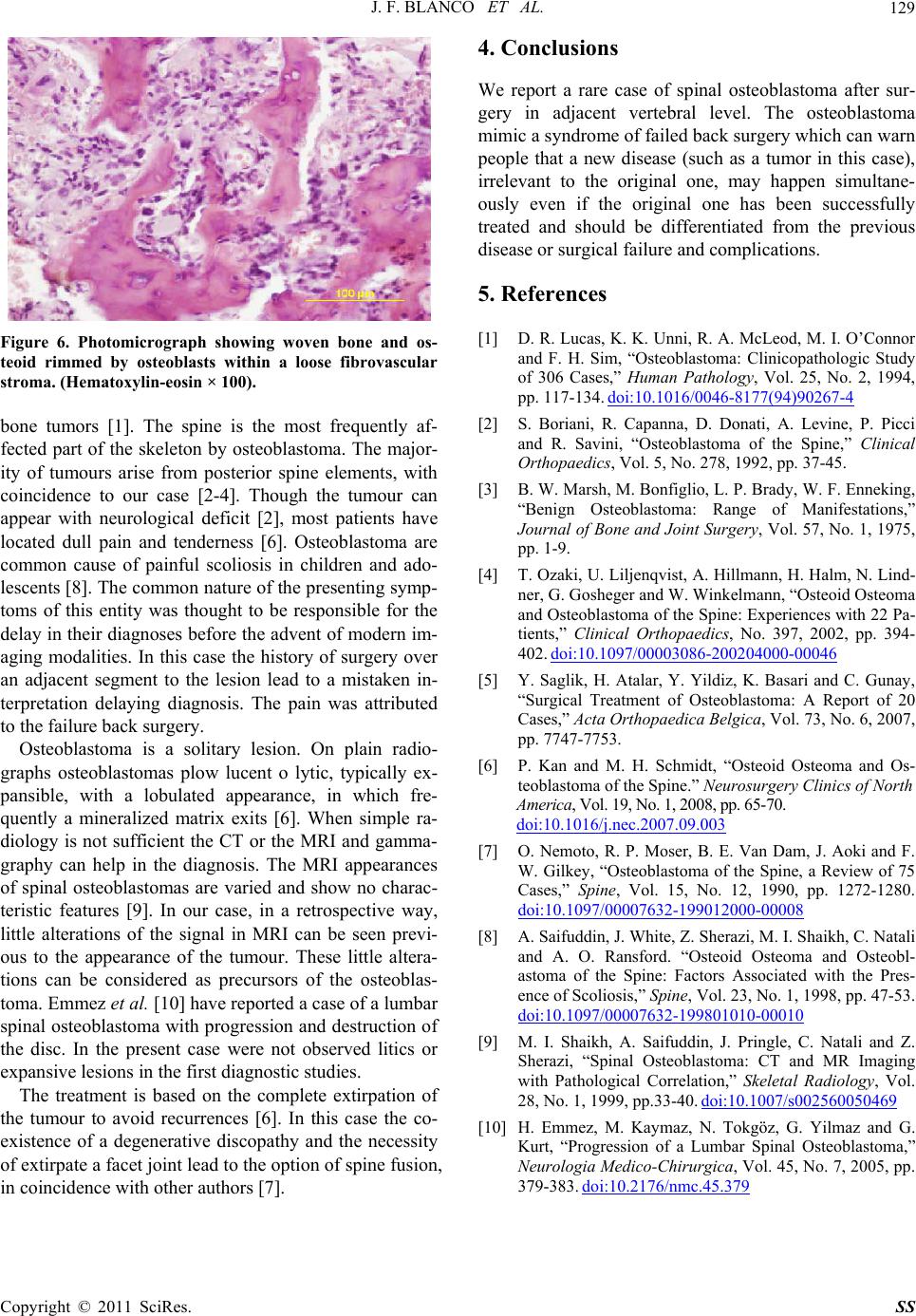
Figure 6. Photomicrograph showing woven bone and os-
teoid rimmed by osteoblasts within a loose fibrovascular
stroma. (Hematoxylin-eosin × 100).
[2] S. Boriani, R. Capanna, D. Donati, A. Levine, P. Picci
and R. Savini, “Osteoblastoma of the Spine,” Clinical
Orthopaedics, Vol. 5, No. 278, 1992, pp. 37-45.
bone tumors [1]. The spine is the most frequently af-
fected part of the skeleton by osteoblastoma. The major-
ity of tumours arise from posterior spine elements, with
coincidence to our case [2-4]. Though the tumour can
appear with neurological deficit [2], most patients have
located dull pain and tenderness [6]. Osteoblastoma are
common cause of painful scoliosis in children and ado-
lescents [8]. The common nature of the presenting symp-
toms of this entity was thought to be responsible for the
delay in their diagnoses before the advent of modern im-
aging modalities. In this case the history of surgery over
an adjacent segment to the lesion lead to a mistaken in-
terpretation delaying diagnosis. The pain was attributed
to the failure back surgery.
[3] B. W. Marsh, M. Bonfiglio, L. P. Brady, W. F. Enneking,
“Benign Osteoblastoma: Range of Manifestations,”
Journal of Bone and Joint Surgery, Vol. 57, No. 1, 1975,
pp. 1-9.
[4] T. Ozaki, U. Liljenqvist, A. Hillmann, H. Halm, N. Lind-
ner, G. Gosheger and W. Winkelmann, “Osteoid Osteoma
and Osteoblastoma of the Spine: Experiences with 22 Pa-
tients,” Clinical Orthopaedics, No. 397, 2002, pp. 394-
402. doi:10.1097/00003086-200204000-00046
[5] Y. Saglik, H. Atalar, Y. Yildiz, K. Basari and C. Gunay,
“Surgical Treatment of Osteoblastoma: A Report of 20
Cases,” Acta Orthopaedica Belgica, Vol. 73, No. 6, 2007,
pp. 7747-7753.
Osteoblastoma is a solitary lesion. On plain radio-
graphs osteoblastomas plow lucent o lytic, typically ex-
pansible, with a lobulated appearance, in which fre-
quently a mineralized matrix exits [6]. When simple ra-
diology is not sufficient the CT or the MRI and gamma-
graphy can help in the diagnosis. The MRI appearances
of spinal osteoblastomas are varied and show no charac-
teristic features [9]. In our case, in a retrospective way,
little alterations of the signal in MRI can be seen previ-
ous to the appearance of the tumour. These little altera-
tions can be considered as precursors of the osteoblas-
toma. Emmez et al. [10] have reported a case of a lumbar
spinal osteoblastoma with progression and destruction of
the disc. In the present case were not observed litics or
expansive lesions in the first diagnostic studies.
[6] P. Kan and M. H. Schmidt, “Osteoid Osteoma and Os-
teoblastoma of the Spine.” Neurosurgery Clinics of North
America, Vol. 19, No. 1, 2008, pp. 65-7 0.
doi:10.1016/j.nec.2007.09.003
[7] O. Nemoto, R. P. Moser, B. E. Van Dam, J. Aoki and F.
W. Gilkey, “Osteoblastoma of the Spine, a Review of 75
Cases,” Spine, Vol. 15, No. 12, 1990, pp. 1272-1280.
doi:10.1097/00007632-199012000-00008
[8] A. Saifuddin, J. White, Z. Sherazi, M. I. Shaikh, C. Natali
and A. O. Ransford. “Osteoid Osteoma and Osteobl-
astoma of the Spine: Factors Associated with the Pres-
ence of Scoliosis,” Spine, Vol. 23, No. 1, 1998, pp. 47-53.
doi:10.1097/00007632-199801010-00010
[9] M. I. Shaikh, A. Saifuddin, J. Pringle, C. Natali and Z.
Sherazi, “Spinal Osteoblastoma: CT and MR Imaging
with Pathological Correlation,” Skeletal Radiology, Vol.
28, No. 1, 1999, pp.33-40. doi:10.1007/s002560050469
The treatment is based on the complete extirpation of
the tumour to avoid recurrences [6]. In this case the co-
existence of a degenerative discopathy and the necessity
of extirpate a facet joint lead to the option of spine fusion,
in coincidence with other authors [7].
[10] H. Emmez, M. Kaymaz, N. Tokgöz, G. Yilmaz and G.
Kurt, “Progression of a Lumbar Spinal Osteoblastoma,”
Neurologia Medico-Chirurgica, Vol. 45, No. 7, 2005, pp.
379-383. doi:10.2176/nmc.45.379