Open Journal of Obstetrics and Gynecology
Vol. 3 No. 1A (2013) , Article ID: 27687 , 5 pages DOI:10.4236/ojog.2013.31A026
Professionalism education of OB/GYN resident physicians: What makes a difference?
![]()
Department of OB/GYN, Thomas Jefferson University Philadelphia, USA
Email: Brett.worly@jefferson.edu
Received 29 October 2012; revised 30 November 2012; accepted 8 December 2012
Keywords: Curriculum Development; Education; Medicine; Narrative; OB/GYN; Physician; Professionalism; Resident
ABSTRACT
Objective: The aim of this study was to evaluate the efficacy of a new Professionalism curriculum in an Obstetrics and Gynecology (OB/GYN) residency after introducing Narrative Medicine and Professional Development/Support Group (PDSG) programs. Methods: 32 OB/GYN residents participated in this IRB approved pilot study. Twenty residents were assessed with the Barry Challenges to Professionalism Questionnaire (Barry), the Jefferson Scale of EmpathyPhysician Version (JSE), and the Jefferson Scale of Attitudes Toward Physician-Nurse Collaboration (JSAT) in August 2010, as controls. Five Narrative Medicine sessions and four PDSG sessions were then used from August 2010-May 2011, for resident physician professionalism education. Seventeen residents then underwent post-testing with the Barry, JSE, and JSAT in May 2011. Results: The pre-test/post-test Barry comparison showed an improvement in scores after introduction of the new Narrative Medicine and PDSG curriculum (7.6 +/− 2.1 versus 8.4 +/− 1.6; p = 0.10) though this was not statistically significant. Pre-test/post-test comparison of JSAT scores showed a statistically significant decline in collaboration (52.3 +/− 4.1 versus 49.7 +/− 3.7; p = 0.028) while JSE scores showed a downward trend in empathy (109.3 +/− 10.0 versus 104.8 +/− 9.2; p = 0.086). Conclusion: Narrative Medicine and PDSG small group sessions could be an effective component of OB/GYN resident physician Professionalism curriculum. This pilot project was underpowered, due to limited resources.
1. INTRODUCTION
Professionalism is an important attribute for physicians, with roots in early medicine from the time of Hippocrates. Many have worked to define “professionalism”, and this definition continues to evolve with changes in medicine. The American Board of Internal Medicine emphasized professionalism formally in 1995, when it published a definition of professionalism and qualities for members to strive for, including altruism, respect for others, accountability, excellence, duty and advocacy, honor, integrity, and ethical and moral standards (Project Professionalism, 2012) [1]. The Accreditation Council for Graduate Medical Education (ACGME) issued a statement in 1999, stating that “Core Competencies” should be taught to every resident, including professionalism (ACGME, 1999) [2]. The impact of suboptimal professional behavior was further demonstrated in 2006, when the Institute of Medicine estimated that medical errors cost as much as $17 - 29 billion per year, with some of these errors potentially reduced or eliminated with improved professionalism (Kohn, 2000; Rogers, 2006) [3, 4].
Professionalism research has increased recently in the fields of General Surgery and Internal Medicine (Reed, 2006; Coverdill, 2010) [5,6]. Obstetrics and Gynecology (OB/GYN) is similar in some ways to General Surgery and Internal Medicine, but our field has its own unique challenges and it is still unclear how best to teach professionalism to Obstetrics and Gynecology resident physicians (Adams, 2006) [7]. Long hours in training, an increasingly female dominated specialty, all female patients, dealing with the joys and tragedies of pregnancy, and working within the framework of each stage of a woman’s reproductive life contribute to the excitement of the specialty, but also contribute to a demanding lifestyle for OB/GYN resident physicians. Empathy is an important component of professionalism that can be affected by burnout, common in OB/GYN.
2. MATERIALS AND METHODS
The study objectives were to design, implement, and assess a new OB/GYN resident Professionalism curriculum using Professionalism Development/Support Groups (PDSG) and Narrative Medicine Group groups. We hypothesized that OB/GYN resident physicians would see improvement in professionalism scores as measured by the Barry Challenges to Professionalism Questionnaire (Barry) questionnaire (Barry, 2000) [8], when controlling for resident burnout through the use of the Jefferson Scale of Empathy-Physician Version (JSE) (Hojat, 2002) [9], and the Jefferson Scale of Attitudes Toward Physician-Nurse Collaboration (JSAT) (Hojat, 1999) [10].
We used a prospective cohort design with a cross-sectional convenience sample, to evaluate OB/GYN resident physician professionalism, empathy, and physician-nurse collaboration. The study was approved by the Institutional Review Board of Thomas Jefferson University. Informed consent was obtained from participants. Inclusion criteria were OB/GYN resident physicians who agreed to participate and signed informed consent. Exclusion criteria were participants from other specialties and other health care professionals. Twenty Thomas Jefferson University OB/GYN resident physicians participated in a baseline assessment consisting of the Barry, JSAT, and the JSE in August 2010. All 32 OB/GYN resident physicians then attended the five Narrative Medicine and four PDSG small group hour-long sessions from August 2010-May 2011, when their schedules allowed for it. Seventeen OB/GYN resident physicians participated in a subsequent post-test exercise in May 2011, in an attempt to evaluate the efficacy of the Professionalism curriculum. Resident physicians were also asked to evaluate the Narrative Medicine and PDSG curriculum with a 5-item Likert rating at the conclusion of the course.
PDSG are resident-focused sessions led by a Psychologist without planned content, and are used to examine issues of humanism in the medical profession, encountered by residents on a daily basis. A second program, Narrative Medicine groups, are comprised of regular meetings where a prompt is given and participants write for a set time about their experiences relating to a given professionalism topic, such as “interpersonal conflict”. Then, members of the group read their narratives and discuss the issues involved relating to professionalism (Pearson, 2008) [11]. They are different in that PDSG groups are participant driven, in that participants chose a theme to be examined, whereas in Narrative Medicine, there is a leader driven discussion of a theme illustrated by the examples set forth by participants. Topics of the Narrative Medicine small group sessions included interpersonal conflict, handling bad outcomes, physician burnout, handling emotion in practice, and dealing with the disruptive physician. Methods of teaching professionalism, as discussed above, have not been extensively researched for efficacy in the OB/GYN literature.
In our study we used the Barry Challenges to Professionalism Questionnaire (Barry) to assess the status of the professionalism of resident physicians, and whether the curriculum was effective. The Barry is an externally validated, self-administered 6-item tool to measure professionalism in resident physicians. In this questionnaire scenarios are presented to the residents with multiple choice answers as to how to respond to an ethically difficult situation. Categories included on the Barry Professionalism questionnaire include receipt of gifts, financial investments, patient confidentiality, physician impairment, harassment, and honesty with patients. “Best” answers on the multiple choice Barry are given a score of two, acceptable answers are given a score of 1, and other answers are given a score of 0. The Barry was selected to assess resident professionalism because it was a short, externally validated, convenient questionnaire (Barry, 2000; Tokuda, 2009) [8,12].
In view of a “burnout rate” reported to be as high as 64% - 76% in OB/GYN physicians (O’Connell, 2009) [13], assessment of physician empathy and collaboration appear to be important components in evaluating resident physician development. The Jefferson Scale of Empathy (JSE), and the Jefferson Scale of Attitudes toward Physician-Nurse Collaboration (JSAT) can be used to assess resident physicians’ insight and strength in these areas (Hojat, 2002; Hojat, 1999) [9,10]. The Jefferson Scale of EmpathyPhysician Version is an externally validated, self-administered, 20-item scale, which uses a 7-item Likert scale to evaluate statements regarding empathy. Phrases such as, “I try to imagine myself in my patients’ shoes when providing care to them,” and “I believe that emotion has no place in the treatment of medical illness,” are rated on a 7-item Likert scale (Strongly Agree = 7, Strongly Disagree = 1, with several of the statements reverse-coded as appropriate) (Hojat, 2002) [14]. The Jefferson Scale of Attitudes toward Physician-Nurse Collaboration is a 15-item scale that is also externally validated, and uses a 4-item Likert scale to evaluate statements of collaboration such as, “Physicians should be educated to establish collaborative relationships with nurses,” and “Doctors should be the dominant authority in all health care matters.” (4 = Strongly Agree, 1 = Strongly Disagree, with several statements reverse-coded as appropriate). These evaluation tools were scored as previously reported (Hojat, 1999) [10].
Participants were characterized with regard to demographic variables such as age, residency year, and length of employment. Continuous variables were summarized by the mean, percentage, and standard deviation. Where variables cannot be reasonably considered normally distributed, transformations were applied to achieve approximate normality where appropriate. Categorical variables, nominal and ordinal, were summarized by frequencies. Analysis of variance (ANOVA) was used for comparing the effects of stimulus class for continuous normally distributed variables (some of which have been transformed for this purpose), with the Kruskal-Wallis test used for the non-normal variables. Discrete variables were compared using either the Chi-square or Fishers exact test. The standard of statistical significant difference was set at p < 0.05.
Demographic Data were described using means, standard deviations, and percentages (Table 1). Continuous variables were compared using matched t tests. All data were analyzed using SAS 9.2.
3. RESULTS
Twenty OB/GYN residents out of a 32 resident OB/GYN residency program attended the introductory lecture for the study and agreed to participate. Attendance ranged from 25% - 75% of residents per resident-year cohort for each individual session. Age (28.7 +/− 1.9) was also found to significantly affect Barry Professionalism scores, with older participants scoring better on the Barry questionnaire (p < 0.05).
The post-test session was attended by 17 resident physicians, and all who attended completed the evaluations. Age was not included by one resident. Three resident physicians did not include their rank year. Residents with missing information were not included in Table 1, but were included in the data analysis.
Barry Professionalism questionnaire results increased from preto post-test, however did not show a statistically significant increase, (7.6 +/− 2.1 versus 8.4 +/− 1.6; p = 0.10). Individual categories within the Barry were also not statistically significantly different (Figure 1). With further evaluation of data, it was discovered that a subset of 2 residents showed signs of extreme burnout on the Collaborative (JSAT) and Empathy (JSE) questionnaires. When these two residents were controlled for by normalizing the Barry professionalism score with a z score and correcting for JSE and JSAT scores, professionalism scores showed a statistically significant improvement following the intervention, (−0.44 +/− 1.5 versus 0.52 +/− 0.9; p = 0.025). A secondary analysis of this project revealed a greater improvement in Barry scores for second, third, and fourth year residents, compared to first year residents during the postand pre-tests (p < 0.05).
Collaboration scores on the JSAT showed a statistically significant worsening over the 10-month time period (52.3 +/− 4.1 versus 49.7 +/− 3.7; p = 0.028). Empathy scores on the JSE also worsened from preto posttest, however were not statistically significant, (109.3 +/− 10.0 versus 104.8 +/− 9.2; p = 0.086). Resident physicians liked the Narrative Medicine small group sessions, with 53% saying it was “Somewhat Helpful”, or better in evaluation on a 5-point Likert scale.
4. DISCUSSION
The primary outcome of the study suggests that OB/ GYN resident physicians had a non-statistically significant improvement in their Barry Professionalism scores after the new Narrative Medicine and PDSG curriculum change. This suggests that we may have improved professionalism in our OB/GYN residents with our new curriculum. Narrative Medicine groups and/or PDSG in isolation have not been previously assessed in OB/GYN resident physicians.
The pre-test/post-test comparison of resident physicians with the JSAT and JSE reveals a statistically significant worsening in collaboration scores, and a downward worsening trend in empathy scores. More likely, these resident physicians are showing signs of burnout from other stressors. It is possible that the new curriculum slowed down the rate of burnout, but this requires further study.
Important considerations in this evaluation include the small sample size, and a convenience sample. The convenience sample could include selection bias, and make this curriculum appear to be overly efficacious. We made every attempt to ensure universal participation of residents throughout this study, however this was not possible given schedule conflicts. Increased OB/GYN resident participation would occur with this curriculum if attendance was required by the resident program director.
The cross-sectional, convenience sample design of this
Table 1. Demographic data. Subjects listed by OB/GYN resident year cohort. Values are given as number (percentage) or mean ± SD unless otherwise indicated.
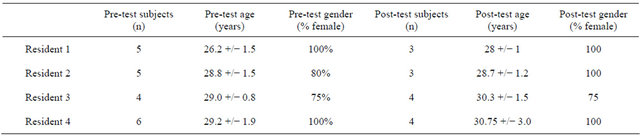

Figure 1. Comparison of preand post-test results for OB/GYN residents on Barry Professionalism questionnaire, by category.
study also may have affected the results, and only associations, not causal relationships, can be drawn from cross-sectional studies. A prospective, randomized controlled trial with frequent, more thorough professionalism evaluations would be the optimal design to identify if Narrative Medicine and PDSG curriculum components are an effective and efficient means for teaching OB/ GYN resident physicians professionalism.
Residents were not matched in preand post-testing, because there was more interest in resident year and age than matching groups, as there was a significant resident concern for anonymity in a small group. Resident physicians were reluctant to give feedback and criticism to a new curriculum from a respected attending physician, even when guaranteed anonymity. Resident physicians purposefully omitted their cohort year in an attempt to avoid any possibility of identification or matching of each questionnaire and individual resident physician comments. Anonymity was more important than matched outcomes, given the small sample size of the study. The results of this study would have been stronger if anonymous identifying links had been used to track residents in preand post-testing, thus allowing for matched controls.
It is also unknown whether the improved Barry Professionalism scores correlate with a difference in how resident physicians perform on a daily basis in relations with patients and healthcare professionals. The Barry Professionalism scores are surrogates for professional behavior, and simply performing better on the questionnaire may or may not translate to actual daily improvement for the OB/GYN resident physicians. The Barry Professionalism scores focus on six limited areas of professionalism, but professionalism includes more than just these attributes. The Barry Professionalism questionnaire has been internally and externally validated (Barry, 2000; Tokuda, 2009) [8,12], but a more thorough evaluation could be performed with more extensive testing, to evaluate the impact of this curriculum on other aspects of professionalism.
5. CONCLUSION
In conclusion, our pilot study identified important associations in a new OB/GYN resident physician Professionalism curriculum. The Narrative Medicine and Professional Development/Support Group Professionalism curriculum may improve OB/GYN resident professionalism, when controlling for resident physician burnout. Collaboration scores showed a statistically significant worsening during our study, while Empathy scores showed a worsening trend. While professionalism training has been undertaken in many resident physician programs, large trials with matched controls, and a more in-depth evaluation of professionalism with clinical correlation still need to be performed to assess efficacy.
6. ACKNOWLEDGEMENTS
Funding for this project was received from the Thomas Jefferson University InterProfessional Education Center.
REFERENCES
- Project Professionalism. The American Board of Internal Medicine. http://www.abimfoundation.org/Resource-Center/Bibliography/~/media/Files/Resource%20Center/Project%20professionalism.ashx.
- Accreditation Council for Graduate Medical Education. ACGME Outcome Project. http://www.acgme.org/outcome/comp/compMin.asp.
- Kohn, L.T., Corrigan, J.M., Donaldson, M.S., Eds. (2000) To err is human: Building a safer health system. National Academy of Press, Washington DC.
- Rogers Jr., S.O., Gawande, A.A., Kwaan, M., Puopolo, A.L., Yoon, C., Brennan, T.A., et al. (2006) Analysis of surgical errors in closed malpractice claims at 4 liability insurers. Surgery, 140, 25-33. doi:0.1016/j.surg.2006.01.008
- Reed, D.A, West, C.P, Mueller, P.S., Ficalora, R.D., Engstler, G.J. and Beckman, T.J. (2008) Behaviors of highly professional resident physicians. Journal of the American Medical Association, 300, 1326-1333. doi:0.1001/jama.300.11.1326
- Coverdill, J.E., Carbonell, A.M., Fryer, J., Fuhrman, G.M., Harold, K.L., Hiatt, J.R., et al. (2010) A new professionalism? Surgical residents, duty hours restrictions, and shift transitions. Academic Medicine, 85, S72-S75. doi:0.1097/ACM.0b013e3181ed455b
- Adams, K.E., O’Reilly, M., Romm, J. and James, K. (2006) Effect of Balint training on resident professionalism. American Journal of Obstetrics & Gynecology, 195, 1431-1437. doi:0.1016/j.ajog.2006.07.042
- Barry, D., Cyran, E. and Anderson, R.J. (2000) Common issues in medical professionalism: Room to grow. American Journal of Medicine, 108, 136-142. doi:0.1016/S0002-9343(99)00405-2
- Hojat, M., Gonnella, J.S., Nasca, T.J., Mangione, S., Vergare, M. and Magee, M. (2002) Physician empathy: Definition, components, measurement and relationship to gender and specialty. American Journal of Psychiatry, 159, 1563-1569. doi:0.1176/appi.ajp.159.9.1563
- Hojat, M., Fields, S.K., Veloski, J.J., Griffiths, M., Cohen, M.J. and Plumb, J.D. (1999) Psychometeric properties of an attitude scale measuring physician-nurse collaboration. Evaluation & the Health Professions, 22, 208-220. doi:0.1177/01632789922034275
- Pearson, A.S., McTigue, M.P. and Tarpley, J.L. (2008) Narrative medicine in surgical education. Journal of Surgical Education, 65, 99-100. doi:0.1016/j.jsurg.2007.11.008
- Tokuda, Y., Barnett, P.B., Norisue, Y., Konishi, R., Kudo, H. and Miyagi, S. (2009) Questionnaire survey for challenging cases of medical professionalism in Japan. Medical Teacher, 31, 502-507. doi:0.1080/01421590802203488
- O’Connell, V.A., Youcha, S. and Pellegrini, V. (2009) Physician burnout: The effect of time allotted for a patient visit on physician burnout among OB/GYN physicians. The Journal of Medical Practice Management, 24, 300-313.
- Hojat, M., Gonnella, J.S., Mangione, S., Nasca, T.J., Veloski, J.J., Erdmann, J.B., et al. (2002) Empathy in medical students as related to academic performance, clinical competence and gender. Medical Education, 36, 522-527. doi:0.1046/j.1365-2923.2002.01234.x

