Subclinical Hypothyroidism and Isolated Hypothyroxinemia during Pregnancy and Their Association with Pregnancy Outcome: A 2-Year Study ()
1. Introduction
Normal pregnancy entails substantial changes in maternal thyroid function. Inadequate adaptation to these changes in thyroid physiology results in thyroid dysfunction [1] [2] . Some of these alterations in thyroid function occur due to increased thyroid hormone-binding globulin (TBG), iodine clearance in the kidneys, and thyrotrophic effect of human chorionic gonadotropin (HCG) [3] [4] . The prevalence of overt hypothyroidism is 1% - 1.5% [5] , of subclinical hypothyroidism 1.5% - 5% [6] and of isolated hypothyroxinemia, 2.5% [7] . The 2011 American Thyroid Association guideline for diagnosis of thyroid disease in pregnancy determined the normal limits of TSH as 0.1 - 2.5 mlU/L in the first, 0.2 - 3 mlU/L in the second and 0.3 - 3.0 mlU/L in the third trimester [8] . Overt hypothyroidism is defined as TSH levels above these limits and fT4 below the 5th percentile. Subclinical hypothyroidism is defined as TSH above these limits and fT4 between the 5th and 95th percentile and isolated hypothyroxinemia as TSH below the above limits and fT4 below the 5th percentile.
Although it is established that overt hypothyroidism in pregnancy is associated with many of adverse outcomes, the effects of subclinical hypothyroidism and isolated hypothyroxinemia on pregnancy outcomes are still controversial [9] - [18] .
Subclinical hypothyroidism might be associated with preterm delivery, low Apgar score, fetal death and miscarriages [19] [20] [21] [22] . According to other studies, it is not associated with any complications. Equally, isolated hypothyroxinemia is associated with preterm labor, high birth weight and neurocognitive deficits in children. In other studies there was no association with complications [23] [24] . According to other studies, subclinical hypothyroidism affects 0.4% - 1% of pregnancies and isolated hypothyroxinemia about 2%, in iodine- sufficient regions and 25% - 30% in iodine deficient regions [24] . The 2011 guidelines for the management of thyroid dysfunction do not recommend universal screening of healthy women for thyroid dysfunction before pregnancy [8] . We carried out the present study in order to know whether the subclinical hypothyroidism or isolated hypothyroxinemia are associated with adverse pregnancy complications in our pregnant population of Western Greece.
2. Materials and Methods
Maternal thyroid hypofunction was defined as 1) subclinical hypothyroidism when TSH was more than 3 mIU/L for the 3rd trimester and free T4 between the 5th and 95th percentiles or 2) isolated hypothyroxinemia when TSH was less than 3 mIU/L for the 3rd trimester and free T4 less than the 5th percentile. Overt hypothyroidism is defined as an elevated TSH (>2.5 mIU/L for the 1st trimester or 3 mIU/L for the 3rd trimester) in conjunction with a decreased FT4 concentration. Women with TSH levels of 10.0 mIU/L or above, irrespective of their FT4 levels, are also considered to have overt hypothyroidism.
This is a retrospective study carried out at Ο&G clinic of the University Hospital, Ioannina. We went through the medical records of 2200 pregnant women followed up in our department throughout the years 2014 and 2015. We searched for evidence of thyroid function testing for these women, as in our hospital thyroid function control is not routinely tested during pregnancy. We identified 469 (21.3%) healthy singleton pregnant women whose third trimester thyroid function was tested during these 2 years. The included women were assigned to 3 different groups: Group 1 (n = 273) were euthyroid, Group 2 (n = 51) had subclinical hypothyroidism and Group 3 (n = 102) had isolated hypothyroxinemia. The rest (n = 43) were excluded from the study as they had Overt Hypothyroidism and other thyroid function issues. We also excluded those with chronic conditions, such as diabetes mellitus, hypertension or other autoimmune diseases. The Socio Demographic characteristics of the study population have been included in Table 1.
Each one of the pregnant women, apart from the thyroid function, was also checked for obstetric outcomes and specifically the week of labor, birth weight
![]()
Table 1. Socio demographic characteristics of participants.
and the history of miscarriages (fetal loss before 24 weeks of gestation). Potential confounding factors including maternal age, parity, smoking, and history of medical problems, gender of the embryo, Rh profile and birth with cesarean section for each one of the pregnant women were also examined and were correlated with thyroid function. In order to investigate a possible correlation between thyroid function and cesarean section labor, we considered only women who had their first CS during this study period.
We used one-way ANOVA to compare the means of numerical data between the 3 groups and chi-square test to assess the relationship between maternal thyroid function and obstetric outcomes. Further regression modeling identified the statistically significant obstetric outcomes in the thyroid hypofunction group.
3. Results
A total of 469 singleton pregnant women enrolled in the study. We tested their thyroid function during the third trimester and a percentage of 5.5% (26 of 469) were found to have overt hypothyroidism, 10.9% were found to have subclinical hypothyroidism (51 of 469), 21.7% isolated hypothyroxinemia (102 of 469) and 58.2% (273 of 469) were found to be euthyroid (Chart 1) and 9.1% (43 of 469) did not fit to any category. Women with overt hypothyroidism or other chronic disease such as diabetes mellitus, hypertension or other autoimmune disease were excluded from the study.
The Socio Demographic Characteristics of the study population are given in Table 1. The mean age of the study population was 31.8 years and the mean gestational age (GA) 38 weeks. In this study we also checked the mean birth
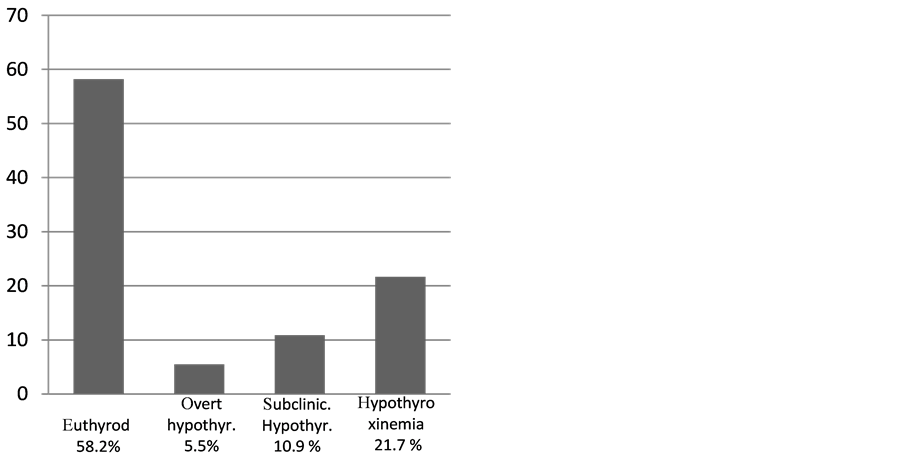
Chart 1. Prevalence of overt hypothyroidism, subclinical hypothyroidism and isolated hypothyroxinemia in the total of 469 pregnant women who were tested at the University Hospital of Ioannina, during the years 2014-2015.
weight (BW), mean number of miscarriages and the mean number of previous cesarean sections (CS). In addition, we also checked the prevalence of the male gender of the embryo, of caesarian section, the percentage of other diseases such as diabetes mellitus and preeclampsia, the percentage of smokers and Rh negative blood profile. All the above characteristics were examined for the total of the participants and for those with subclinical hypothyroidism and isolated hypothyroxinemia separately. Group 1 in Table 1 corresponds to subclinical hypothyroid participants and Group 2 to those with isolated hypothyroxinemia.
Subclinical hypothyroidism and hypothyroxinemia were associated with Gestational age of delivery (GA), birth weight (BW), and history of miscarriage and patients were compared with euthyroid ones (Table 2).
Analysis of the results shows that subclinical hypothyroidism does not affect birth weight or week of labor and does not have any correlation with history of miscarriages (Table 2) and analysis of the results for isolated hypothyroxinemia, show that hypothyroxinemia does not affect the week of labor and is not associated with history of miscarriages. To the contrary, the analysis shows that hypothyroxinemia is associated with higher infants’ birth weight than those of euthyroid women (P < 0.05) (Table 2).
Mean maternal age, parity, smoking, gender of embryo; Rh profile and cesarean section for first time were similar in the three studied groups (Table 3).
4. Discussion
Thyroid disease is the second most common endocrine disorder complicating
![]()
Table 2. Comparison of the obstetric outcomes of patients with thyroid hypofunction compared with euthyroid patients.
![]()
Table 3. Comparison of the demographic characteristics of patients with thyroid hypofunction compared with euthyroid patients.
pregnancy. Attention to thyroid dysfunction during pregnancy has certainly increased in the past decade, particularly in the area of subclinical thyroid dysfunction.
Overt hypothyroidism affects pregnancy and neonatal outcomes in many ways. Many published studies have shown that overt hypothyroidism is associated with preterm labor, low birth weight, miscarriages, intrauterine embryo death and neurodevelopmental complications for the infant [25] [26] [27] [28] [29] .
In our study we found that 5.5% of the tested pregnant women were known hypothyroid and they had started treatment from the first trimester. The probable explanation for this high prevalence may be the deficiency of Iodine in the diet of the pregnant population of Ioannina.
On the other hand the effects of maternal subclinical hypothyroidism and isolated hypothyroxinemia on pregnancy and neonatal outcomes are not definitely confirmed and conflicted results exist among the published studies [19] [22] [24] [25] [26] [27] .
In one study of women screened before midpregnancy, women with subclinical hypothyroidism had higher incidences of preterm birth, placental abruption, and admission of infants to the intensive care nursery when compared with control women [30] . Conversely, in another study of First- and Second-Trimester Evaluation of Risk (FASTER) Trial participants, Cleary-Goldman et al. [22] did not find a link with adverse obstetrical outcomes, such as miscarriage, gestational hypertension, preeclampsia, gestational diabetes, placenta previa, placenta abruption, preterm labor, premature rupture of membranes, low or high birth weight and perinatal mortality.
In a study of 233 pregnant women with isolated hypothyroxinemia, Casey et al. [31] reported that there were no increased adverse perinatal outcomes associated with the condition. Conversely, Cleary-Goldman et al. [22] reported a 2- fold incidence of fetal macrosomia in these women. In another smaller study of 89 women with maternal hypothyroxinemia, there was no evidence of an increased risk for fetal growth restriction or preterm birth [32] .
Because there are still ongoing studies trying to clarify whether or not maternal subclinical hypothyroidism and isolated hypothyroxinemia on pregnancy are associated with adverse outcomes, we decided to carry out the present study to contribute to this still unanswered question. In addition to this, this study is a unique study in the region of Western Greece.
In our study among adverse outcomes, we decided to investigate neonatal birth weight, week of labor and association with miscarriage. We also tried to find if there was an association between thyroid function and maternal age, parity, smoking, Rh, fetus gender and mode of delivery.
Our results indicate that subclinical hypothyroidism was not associated with neonatal birth weight, week of labor or history of miscarriage, a finding which agrees with that of Clearly-Goldman et al. [22] . There was also no association with the other demographic characteristics that were tested.
Unlike subclinical hypothyroidism, isolated hypothyroxinemia in our study was associated with higher birth weight, but not with history of miscarriage or with the week of labor. Clearly-Goldman et al showed also that women with isolated hypothyroxinemia were not at increased risk for the majority of pregnancy complications [22] . However, hypothyroxinemia was associated with birth weight greater than 4000 g, a finding similar to ours, namely that women with hypothyroxinemia give birth to heavier babies than euthyroid ones.
Women with diabetes mellitus, hypertension and autoimmune diseases were excluded from our study, as all those conditions are considered confounding factors.
In summary, we did not find a link between subclinical hypothyroidism and adverse pregnancy outcomes in our population. Similarly, hypothyroxinemia was not associated with the majority of pregnancy complications. However, hypothyroxinemia was associated with higher birth weight. This study can be a useful tool in neonatologist hands, to investigate how maternal subclinical hypothyroidism and isolated hypothyroxinemia, might affect neonate and child development and behavior.
We note the following limitations of this study. The study was conducted retrospectively including results from a single, but large, centre where pregnancies from the wider West area of Greece are treated. Also we have not accounted the BMI of women in this study. Our findings combined with results from other studies will help to clarify the still unanswered question of whether maternal subclinical hypothyroidism and isolated hypothyroxinemia should be treated and whether a test for hypothyroidism should become routine during pregnancy.
Disclosure
We certify that no actual or potential conflicts of interest in relation to this article exist.