Caesarean section at a tertiary institution in Southwestern Nigeria—A 6-year audit ()
1. INTRODUCTION
Caesarean section is one of the commonly performed surgical procedure worldwide [1], its rate across Nigeria ranges 20.8% - 34.5% [2-4] while that of United States is 25% and England, Wales and Northern Ireland is 20% [3]. Despite the high rate of this procedure there is still strong aversion for it in this part of the globe [1,5,6]. Caesarean section is associated with higher morbidity and mortality compared with vaginal delivery [7,8]. There are various reports of rate increase over the years across the world. In developed countries, attributed factors include fear of litigation, liberal use of caesarean section for breech presentation, detection of fetal distress by continuous electronic fetal monitoring among others [8] while reasons are less clear in developing countries which include specialist and referral nature of the hospital, unbooked status of most of the patients, increasing use of fetal rate abnormality alone as a measure of fetal distress, overdiagnosis of cephalo-pelvic disproportion by junior doctors and use of caesarean section for patients with previous caesarean section [8,9]. Safety of caesarean section has improved over the decades due to improved anaesthestic techniques which has accounted for rate increase across the world [6,10]. The objective of this study is to look at the trends over six years and the corresponding perinatal outcome in our health facility.
2. MATERIALS AND METHOD
Ladoke Akintola University of Technology Teaching Hospital, Osogbo commenced operation in 2000. It is a 300 bedded tertiary hospital located in the semi-urban state capital of Osun State, Southwestern Nigeria. It was retrospective study from January 1, 2005 to December 31, 2010. Medical records from both central and labour ward were examined. Socio-demographic and other information were obtained. Data were fed into SPSS version 14. Categorical variables were summarized using number and percentages while mean and standard deviation were for continuous variable. Multivariate analysis was done and level of significance was put at less than 5%. Analytical tests were done using SPSS version 14 software.
Ethical approval was obtained from the institution ethic committee.
3. RESULTS
There were 2798 deliveries, 1004 caesarean sections were recorded and 688 were analyzable. The caesarean rate over six years was 35.9%. Yearly caesarean section rate is shown in Figure 1 and yearly perinatal death rate in Figure 2. Emergency caesarean section was 80.2%, Figure 3. 208 (30.2%) were nulliparous women that had caesarean section. The mean age of the delivered women was 29.8 (±4.9) years (19 - 44 years). The median parity was 1 ranging between 0 - 6. The mean gestational age at delivery was 38.7 (±2.4) weeks. The mean duration of surgery was 50.9 (±19.8) minutes. The median admission period was 6 days ranging between 1 - 120 days. The mean birth weight was 3.04 (±0.61) kg. The mean apgar scores at 1 minutes and 5 minutes respectively were 7.1 (±2.1) and 8.7 (±2.2). Majority of the women were within age 20 - 29 years (50.3%), Nulliparous women were 208 (30.2%), and they were mainly of Yoruba ethnic group 680 (98.8%). Majority of them 358 (52.0%)

Figure 1. Annual caesarean section rate.
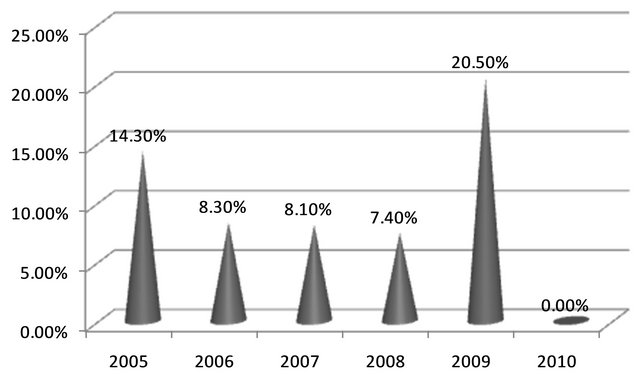
Figure 2. Annual perinatal death rate from caesarean section.
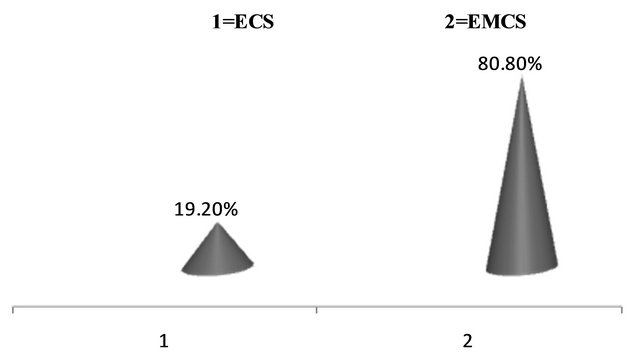
Figure 3. Types of caesarean sections. ECS = Elective caesarean section; EMCS = Emergency caerarean section.
were registered for antenatal care in our health facility while 562 (81.7%) had term caesarean deliveries (Table 1).
The major indication for caesarean section was two previous caesarean sections and above 154 (22.3%), followed by obstructed labour 128 (18.6%), prolonged labour/failure to progress in labour 94 (13.6%) while unclear indications were 6 (0.9%) (Table 2).
Maternal infection 68 (9.9%) ranked highest in complications suffered by the delivered women while maternal death were 20 (2.9%) contributing maternal mortality ratio of 731 per 100,000 live birth. Birth asphyxia 66 (9.6%) was the major perinatal complication while perinatal mortality was 26.7 per 1000 live birth (Table 3).
After adjusting for confounders, women who had a child and above had significant perinatal mortality com-

Table 1. Sociodemographic characteristics.

Table 2. Indications for caesarean section.

Table 3. Feto-maternal complications.
pared with those who were nulliparous, OR = 7.835, (95%CI 2.757 - 22.565, p < 0.001), emergency deliveries had significant perinatal mortality compared to elective deliveries, OR = 5.913, (95%CI 1.393 - 25.111, p < 0.05) and those who had antenatal care outside our health facility had worse perinatal outcome than the women that had antenatal care in our health facility, OR = 7.835, (95%CI 2.757 - 22.265, p < 0.001), Table 4.
4. DISCUSSION
The average caesarean section rate over the six years was 35.9% and reached 40.8% in 2010, the highest so far from all the studies in the country despite strong aversion
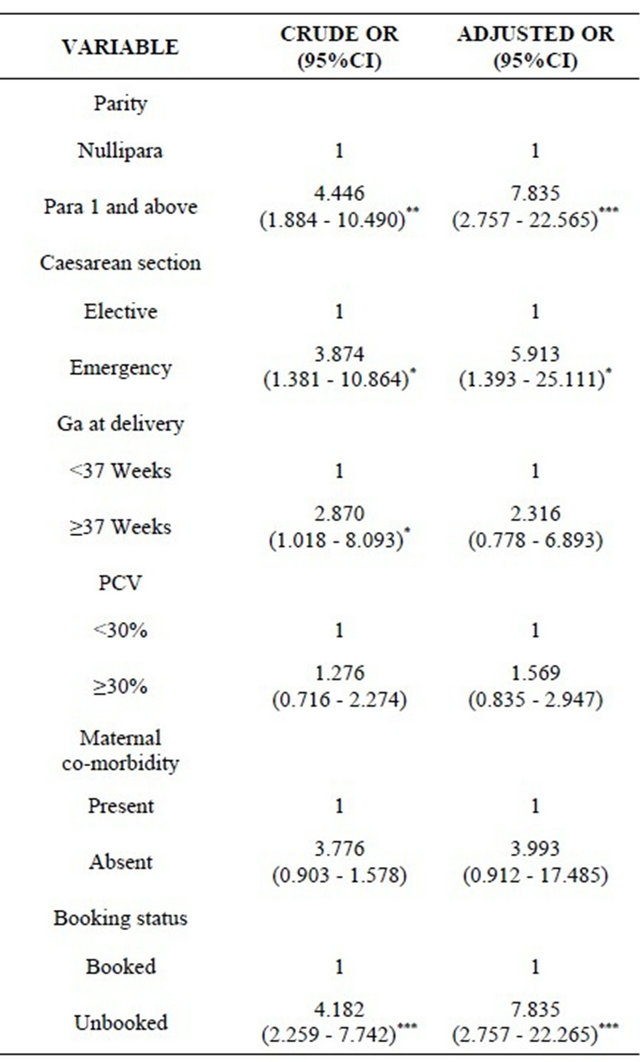
Table 4. Risk factors to perinatal mortality.
*p < 0.005; **p < 0.01; ***p < 0.001.
of Nigerian women to this procedure [1-4,6-8], and much higher than the reports from Tanzania [11], United States and Europe [10,12,13]. The higher rate was associated mainly with repeat caesarean delivery, obstructed labour, failure to progress in labour from poor judgment by the junior doctors, breech presentation due to lack of skill in providing external cephalic version especially to singleton fetuses with no contra-indications to the procedure and fetal distress by relying only on intermittent auscultation with no fetal blood gas analysis to further strengthen the diagnosis of the condition among other indications for caesarean section.
Caesarean section rate of 50.3% reported among age group 20 - 29 years in our study was consistent with findings in the country [8] but lower than 77% from India [14], almost the same rate of 46.7% was reported in United States but in different age group 40 - 54 years in 2009 [15]. The proportion of nullipara that had caesarean section in this study was 30%, similar to reports from the northern region of the country but slightly higher than that reports from same region [8,16]. This proportion is significantly high for this environment where large family size is desired and its implications on perinatal and future reproductive health [17].
The commonest indication for caesarean section was previous caesarean section, which corroborates studies from the eastern part of the country [2,18] and Tanzania [11], this may be due to increase in rates of caesarean section over the years thus reversing the pattern of obstructed labour as commonest indication in previous studies [2,4,19]. Fetal distress also contributed significantly to caesarean section rate, this might be due to over-reliance on intermittent auscultation in the absence of electronic fetal monitoring and fetal scalp sampling.
Surgical wound infection was the commonest cause of maternal morbidity in support of other reports from the country [4,20], probably due to increasing number of those who did not register in our health facility but admitted on account of complicated labour [21]. Caesarean mortality ratio of 731 per 100,000 live births was higher than 480 per 100,000 live births reported from the eastern part of the country but lower than 1180 per 100,000 live birth reported from the South-southern part [4]. This mortality is significantly high compared to vaginal deliveries.
Perinatal mortality rate did not follow any consistent pattern, there was a drop from 14.3% to 7.4% between 2005 to 2008, then peaked in 2009 to 29.5% but fell to zero in 2010. This could be due to variation in standard of practice because there was no significant change in the manpower and infrastructure that might effect this change. This trend is unacceptably high for obvious reasons that maternal morbidity/mortality associated with this procedure coupled with financial burden will further discourage these women from utilizing the facility again, thus patronizing traditional birth attendants and mission homes with hope of attempting vaginal delivery. This practice has resulted in ruptured uterus with attendant adverse maternal and perinatal sequelae [22,23]. Overall, the perinatal death was unacceptable high to justify the increasing trend in caesarean section.
After adjusting for various confounders, multiparity, emergency caesarean section and unbooked women contributed significantly to perinatal deaths. These form the target groups for health education and the need to manage them with utmost caution.
5. CONCLUSION
Caesarean section rate was unacceptably high with no corresponding reduction in perinatal death for its justification. Attempts should be made to reduce the incidence of primary caesarean section by careful management of induction of labour, accurate assessment of fetal distress, patience with management of arrest disorders [24] while efforts must be geared towards acquiring skills in external cephalic version especially in this part of the world where there is strong aversion to abdominal delivery. The risk factors to perinatal death were multiparity, emergency caesarean section and unbooked status of the women, optimizing patient’s condition before surgery will reduce the scourge.
6. ACKNOWLEDGEMENTS
Many thanks to labour ward nurses and medical records for their great assistance in retrieving information. There is neither financial assistance received and nor conflict of interests among the authors.
NOTES