Intracranial Epidural Plasmacytoma Presenting as a Neurosurgical Emergency: Case Report ()
1. Case Report
A 60-year-old right-handed man presented to our emergencies immediately after a mildly severe head trauma with quick loose of consciousness. His medical history was significant for a light chain multiple myeloma diagnosed one year ago for which he underwent chemotherapy with total remission. On admission, the patient’s neurological examination found a Glasgow Coma Score of 13 out of 15 with a confused speech. The patient was rapidly explored by a CT scan which showed a right frontotemporal epidural, biconvex mass, spontaneously hyper dense with no local skull abnormalities (Figures 1

Figure 1. Axial noncontrast CT scan shows a biconvex, spontaneously hyperdense, right frontotemporal mass with moderate space occupying effect.
and 2). Imaging features were strongly suggestive of an epidural hematoma. Although this situation is quite rare in the elderly, the patient underwent an emergency craniotomy with the preoperative diagnosis of an epidural hematoma. Amazingly, the surgeon found no hemorrhage but rather a purple solid tumor which was completely removed. The tumor invaded partially the bone of origin which was scarified and the definitive histological diagnosis was a skull plasmacytoma (Figure 3). The patient’s immediate postoperative course was uneventful, and he recovered quickly. Six days postoperatively, the patient was discharged and addressed for complementary treatment at the oncological institute of origin.
2. Discussion
Plasma cell tumors include solitary plasmacytoma, extramedullary plasmacytoma and more aggressive multiple myeloma which represents the disseminated form of this disease. The latest accounts for approximately 10% of hematologic malignancies and usually occurs in the elderly over 40 years [1].
In sharp contrast to other hematologic malignancies, direct involvement with accumulation of plasma cells in the CNS is extremely rare in multiple myeloma patients and can only be observed in approximately 1% of cases [2]. This extramedullary presentation and⁄or complication of multiple myeloma is generally a result from bone lesions in the cranial vault [3]. Dural reported deposits are

Figure 2. Bone window CT scan showing no osteolytic changes.
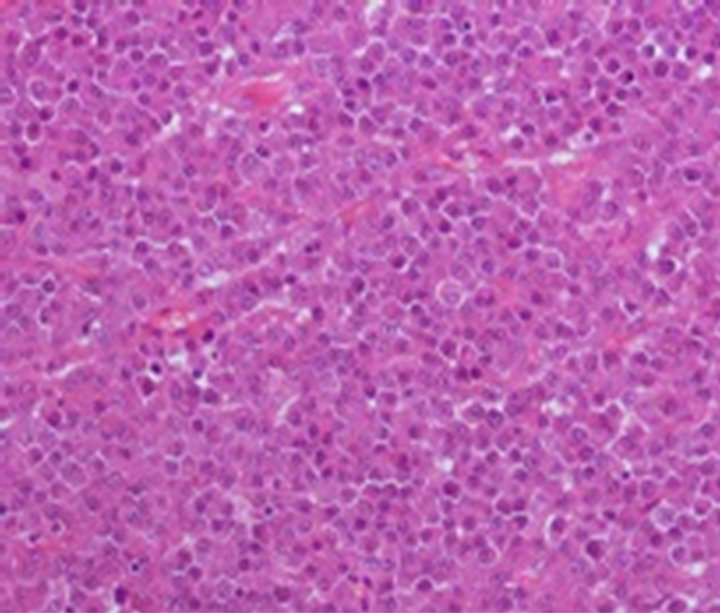
Figure 3. Photomicrograph of the tumor specimen shows classic histological features of a plasmacytoma with abundant plasma cells; Hematoxylin & Eosin, magnification: × 200.
more likely to occur from direct spread from contiguous bone lesions rather than caused by a hematogenous spread, since the dura mater is a relatively avascular structure.
In the majority of patients this complication appears as a terminal event, but it can also develop in patients with a complete systemic remission [2] which was the case of our patient.
Clinical symptoms and signs of multiple myeloma with intracranial growth are rare, but they may be present at disease presentation [4]. Signs of cerebral dysfunction depending on tumor localization can cause somatic symptoms such as fatigue, sleep disturbances, anorexia. Furthermore, patients with a tumor located anteriorly (frontal region) are expected to have emotional distress and depressive symptoms probably originating from limbic release or disinhibition [5]. In the present case, clinical circumstances and post traumatic onset of the symptoms were strongly suggestive of a head injury related lesion.
Radiologically, intracranial plasmacytomas are usually well defined and can arise either within the bone or as an extradural deposit; but always leading to bony erosion [6]. Another standpoint is that these lesions are characterized by their diffuse and important contrast enhancement. CT is better than MRI in delineating subtle bone erosions, but the best assessment is achieved by MRI due to its superiority in the study of both bone marrow and meninges [6] and in such location differential diagnosis includes more common epidural metastases or deposit of leukemia [7,8].
To the best of our knowledge, Rutherford et al, [9] reported the single English medical literature case of solitary plasmacytoma of the skull vault masquerading as an extradural hematoma. In that report, the extradural mass was associated to calvarial lytic changes. What makes our case unique is that no bony changes abutting to the tumor were noted on the preoperative CT scan. Such a finding and the lack of contrast enhanced figures led us to erroneously suspect an extradural hematoma although this condition is quite rare in the elderly (2.8 % of cases) [10]. A potential pitfall, which could entail an inadequate therapy and stresses the importance of preoperative contrast enhanced images as a preferred policy for investigation of extradural masses especially in the elderly and among patients with already known malignancies.
The treatment schedules used for CNS multiple myelomas are heterogeneous, and there is no widely accepted therapeutic approach. If anatomically suitable, the primary therapy is surgery followed by irradiation, since the tumor is exquisitely radiosensitive [3].
Radiosurgery, on the other hand, has been advocated for suitable tumor remnants [11].
Patients with intracranial multiple myeloma, like ours, have been reported to survive for less than one year. A dismal prognosis, that high-dose chemotherapy followed by autologous or allogenic stem cells transplantation has improved [4]. Furthermore, recent discoveries on the fundamental molecular mechanisms behind multiple myeloma cell growth and survival have led to the introduction of novel classes of pharmacologic agents such as thalidomide and bortezomib which may have different activity on extramedullary myeloma due to an antiangiogenic/antiapoptotic effect [4,12].
3. Conclusion
Intracranial plasmacytoma may be confused with epidural hematoma if clinical presentation is suggestive of an acute head injury. Attention needs to be drawn to this preoperative misinterpretation, which may entail an inadequate therapy. For such considerations, we consider that contrast enhanced radiological investigations are of paramount importance for assessing the differential diagnosis of extradural masses, especially in the elderly and in patient with already known malignancies.
NOTES