Hand Hygiene in Pediatric Emergency Care Unit in a Teaching Hospital in Benin ()
1. Introduction
One of the risks associated with the administration of healthcare is the transmission of infectious agents. Such transmission usually occurs during unsafe care and can be breeding ground for infections known as healthcare-associated infections (HCAI). Such infections occur during curative or palliative care administered to a patient by a healthcare professional, though they were neither present nor incubated upon admission [1]. The World Health Organization (WHO) estimates that 1.4 million patients contract HCAI at any moment [2]. Their incidence ranges from 5% to 15% in inpatients in developed countries and could reach 25% in emerging countries [2] [3]. Since 1947, it is knowledged that the transmission of infectious agents causing HCAI occurs mainly through the hands of healthcare professionals, and that, proper hand hygiene decreases the incidence [2]. Standards have therefore been set as far as hand hygiene is concerned, regarding necessary equipment, procedures and opportunities to observe in the delivery of care [2]. For poor countries where these optimal conditions are hardly met (safe drinking water, antiseptic soap, suitable faucets, disposable hand towels, etc.) alcohol-based hand rub which has proved effective, is a great option [2]. While it is well recognized that the fight against HCAI requires good hand hygiene, adherence by healthcare professionals seems to be suboptimal in daily practice. In India, a study carried out in 2018 reported 15.7% as hand hygiene adherence rate [4]. In Benin, Yehouenou et al. found 33.3% in a survey conducted in six public hospitals across the country [5]. A study carried out in 2016 in the neonatology division of HKM National Teaching Hospital in Cotonou, revealed 15% as hand hygiene adherence rate [6]. The purpose of this study is to assess the knowledge and practices of healthcare professionals with regard to hand hygiene in the pediatric intensive care unit within the same hospital.
2. Methods
2.1. Type of Study
It was a three-month observational study conducted from June 3 to September 12, 2019.
2.2. Study Population
On the one hand, the study targeted the healthcare workers present during the study period: doctors (pediatricians and graduating pediatricians), fifth and sixth year medical students, undergraduate nursing students, and allied health professionals (nurses, nursing assistants, or paramedics); and on the other hand, the infrastructure and equipment that are required to ensure hand hygiene.
2.3. Study Tools and Data Collection
The questionnaire and grids used for observing both the healthcare professionals and the premises rely on the World Health Organization guidelines [7].
2.4. Study Variables
The variables collected include seniority in the profession, healthcare professionals training in hand hygiene and healthcare associated infections (knowledge about the modes of microorganism transmission, moments for hand hygiene, the different types of hand hygiene and their duration, etc.), accessibility of hand hygiene equipment (water, soap, alcohol-based disinfectant, etc.), compliance with attire prerequisites. The opportunities for hand hygiene during delivery of healthcare were observed, and this made it possible to determine adherence rate. Finally, we tracked microorganism (no virus) present on the hands of healthcare professionals. Epidata 3.1 and STATA 15.0 were used for data processing and analysis.
2.5. Conducting the Study
The study comprises three parts. The first one was basically a covert observation of the health workers in the implementation of their activities day and night, without their knowledge. Among others, the observation focused on the followings: patient physical examination, invasive procedures (such as placement of peripheral venous access catheters, catheterization, lumbar or as cites puncture, etc.), linen change, etc. At this stage, it was an exhaustive enrollment. The observation criteria were based on the five moments for hand hygiene according to the WHO guidelines [2]. It also focused on existing infrastructure and equipment, as well as the staff clothing hygiene. It was conducted by a doctor from the pediatric emergency care unit, familiar with observation technique and WHO guidelines. Through each 30-minute long observation dedicated to a single healthcare professional, the administration of different care provided to the patient was carefully monitored. Opportunities for performing hand hygiene were determined and recorded. The opportunity exists whenever one of the moments for hand hygiene is present and observed. Adherence rate was calculated according to the following formula:
Adherence (%) = 100 × [number of hand hygiene episodes performed/number of hand hygiene opportunities].
Hand hygiene was considered properly implemented when the health professional observed all steps and duration associated with such practice.
The second part of the study was a self-administered questionnaire on the staff knowledge about hospital hygiene and healthcare associated infections. For a questionnaire to be validated, it had to be returned by the respondent within 48 hours after administration. For each item of the questionnaire, a respondent knowledge was rated as good if the percentage of correct answers was ≥ 80%.
Finally, the health staff had to go through hand swab before and after hand washing. For the last two parts of the study, enrollment of participants was based on convenience. This type of enrollment could constitute a bias for this study. Therefore, only voluntary personnel hands were swabbed and analyzed by specialists from the hospital hygiene department. A sterile swab was used for specimen collected from the palms, fingernails and interdigital folds of each volunteer healthcare worker. Each specimen was assigned an anonymous reference number according to the healthcare worker category group, then immediately transferred to the laboratory.
2.6. Ethical Consideration
This study was carried out with the agreement of the hospital administration, in collaboration with the department of hospital hygiene. All nursing staff were informed about the study, but they were unaware of the period of covert observation and the interviewer’s identity.
2.7. Outcome
2.7.1. Characteristics of Healthcare Workers
A total of 130 healthcare workers were observed, of which 119 returned the correctly completed questionnaires within the allotted time, and 35 gave their consent for swab collection before and after hand washing. The characteristics of these healthcare professionals are presented in Table 1.
![]()
Table 1. Socio-demographics characteristics of the 119 healthcare workers who return the questionnaire.
2.7.2. Healthcare Workers’ Knowledge Regarding the Modes of Microorganism Transmission in Hospital Facilities
Healthcare workers’ theoretical knowledge is presented in Table 2. It appears that, their knowledge was globally unsatisfactory, although most of them benefitted from basic initial training.
2.7.3. Healthcare Workers’ Knowledge Regarding the Moments for Hand Hygiene, and Their Components
Healthcare professionals declared that it is necessary to practice hand hygiene before touching a patient (93.3%), after touching a patient (93.3%), after contact with a patient environment (72.3%), before an aseptic procedure (76.5%), after body fluid exposure (85.5%). Simple hand washing and alcohol based hand rub were known to all, however, only doctors and medical students mentioned antiseptic and surgical hand hygiene. The minimum duration of alcohol-based hand rub was only known by doctors, this, in a proportion of 50%.
2.7.4. Hand Hygiene Adherence Rate by Healthcare Workers during Healthcare Delivery
During the observation period, hand hygiene adherence rate was low (6.9%) regardless of the category and seniority: doctors 9%, nurses 7.5%, nursing assistants 0%, medical students 6.7%, and nursing students 3.8%. Simple hand washing was largely practiced in a proportion of 82%, while alcohol-based hand rub represented 18%. No health professional observed the minimum required duration regardless of the type of hand hygiene practiced. Table 3 is an overview of hand hygiene adherence according to category group and WHO five moments for hand hygiene.
2.7.5. Results of Healthcare Workers’ Hand Swab before and after Hand Washing
The following microorganism was identified in healthcare professionals before hand washing: Staphylococcus saprophiticus, Staphylococcus epidermidis, gram-positive type Bacillus, Enterobacter cloacae, Enterococcus faecalis, Klebsiella pneumoniae, Serratia marcescens and Candida yeast. Transient flora reduced from 15% to 2% after hand washing. Graph 1 shows the number of microorganism isolated according to the category after simple hand washing.
![]()
Table 2. Healthcare workers’ knowledge regarding the modes of microorganism transmission in a hospital facility.
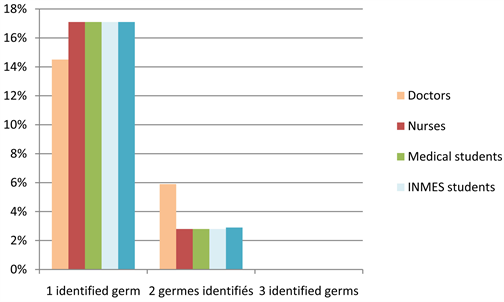
Graph 1. Number of microorganism isolated according to the professional category after simple hand washing.
![]()
Table 3. Hand hygiene adherence rate according to professional category and 5 moment for hand hygiene.
-: This category didn’t do any aseptic procedure.
2.7.6. Observing Prerequisites for Hand Hygiene
In structural terms, hospital water point-of-use was defective, particularly the absence of faucets, or their unsuitable positioning. The soap used for hand hygiene was a mild, non-antiseptic liquid soap. There was shortage of soap and tap water supply. Moreover, disposable hand towels, alcohol based hand rub dispenser at point-of-care, posters or leaflets for visual reminder were non-existent. As far as attire is concerned, almost all the healthcare personnel wore short-sleeved outfits. However, 75% of them had rings on their fingers, jewelry hanging from their ears, and almost half left their hair unprotected.
3. Discussion
The moments for hand-washing and associated techniques are cross-cutting knowledge in human medicine, both for the medical personal and paramedics. Its impact in the fight against healthcare-associated infections has been formally established [8] [9]. A proper practice of hand hygiene by healthcare professionals requires basic equipment: water point-of-use, adequate soap, alcohol-based hand rub, disposable hand towels, etc. [8] [9]. This observational study carried out in CNHU pediatric emergency care unit identified deficiencies with regard to this minimum requirement. These deficiencies could have an impact on healthcare workers’ practice. Engdaw et al. in Ethiopia reported that factors influencing hand hygiene adherence involved access to soap and water [10]. This lack of hand washing equipment is a common situation in low and middles countries [11], and that is the reason WHO recommends alcohol-based hand rub, which is easier to implement [2] [7]. Clothing requirements should be improved within the care unit, especially the wearing of rings, which can be a breeding ground for germs [12]. With the exception of nursing assistants, almost all healthcare professionals attended basic hand hygiene training. However, their level of awareness was low especially regarding transmission modes, the duration of hand washing, and alcohol-based hand hub. The medical staff underrated the risk associated with non-invasive medical equipment such as stethoscopes used from one patient to another. In outpatient medicine services, Zanetti et al. also reported a low rate of stethoscope disinfection in-between two patients [13]. A periodic in-service staff training plan with visual support on HCAI could be set up within the care unit. This will contribute to raising staff awareness about the consequences of HCAI, i.e. extension of hospital stays, additional financial costs, excess mortality and perhaps better hand hygiene practices [14] [15]. The adherence rate found in this study was low < 10% regardless of the category, and this should be a matter of great concern. Ahmed J et al. recorded a rate of 12.3% in Karachi, Tang et al. 11% to 36% depending on the season in a rural hospital in Niger [16] [17]. Higher rates of 31% are reported in Nigeria but still significantly lower than those reported in advanced countries such as England [11] [18]. The implementation of a multimodal strategy based on WHO recommendations will certainly improve hand hygiene adherence within the care unit, as various teams experimented [19] [20] [21] [22]. It is also possible to use emoticons, to remind healthcare professional about hand hygiene, and implement strategies that will boost healthcare workers’ motivation [23] [24] [25]. For example, in a first pilote study performed by Gaube et al. in a german hospital, a monitoring and feedback devices were installed above handrub dispensers that displayed frowny face to remind people to performed hand hygiene. Once used, a smiley face was shown to reinforce the positive behavior. In patient’s room, this can reinforce the hand hygiene behavior by providing instant feedback [23]. Despite the deficiencies recorded in the care unit, a reduction in the transient flora after washing was noted and no healthcare worker had more than two microorganisms on their hands. However, direct observation may have modified the behavior of healthcare professionals who unconsciously could focus on adherence to the different steps of hand hygiene, thus creating bias in the study. However, it seems that the use of simple soap reduced the transient flora as reported in the literature [2]. Nevertheless, given the microorganism isolated from the healthcare professional involved in this study, especially Enterobacter cloacae and Klebsiella pneumoniae known to be multi-resistant and responsible of HCAI in the neonatology department of the same hospital, there is crucial need to emphasize the use of antiseptic soap [26]. Training, visual reminders, and uninterrupted supply of alcohol-based solution or gel are some of the immediate actions to be taken.
4. Conclusion
Hand hygiene adherence rate in pediatric intensive care unit is low. The emergence of new viruses including SARS-COV 2 should be an opportunity for implementing a sustainable hand hygiene plan in the care unit. Indeed, national mobilization and support from development partners have enabled the acquisition of simple, effective and affordable hand washing stations, local production of chlorinated water and supply of alcohol based solution.