Epidemiological and Clinical Aspects of Male Infertility in Patients Consulting at the Urology Department of the Yaounde Central Hospital ()
1. Introduction
Couple infertility is the inability to achieve a clinical pregnancy after 12 months or more of regular sexual intercourse (2 to 3 times/week), in the absence of any contraceptive method [1] [2] . It’s a worldwide public health problem because its frequency and psychosocial impact. About 48.5 to 72.4 million (7 to 9%) couples worldwide have an unresolved fertility problem [3] . In the United States and Western Europe, this problem affects approximately 10 to 15% of married couples [4] . In Africa, more particularly in the sub-Saharan region, the infertility rate among couples varies from one region to another [5] : 30.3% in Nigeria [6] and 20 to 30% in Cameroon [1] . Causes are purely masculine in 40% of cases, feminine in 40% and mixed in 20% of cases [7] . No cause is usually found in 2 to 3% of cases.
Male infertility is the inability of a man to procreate due to an abnormality in his sperm. It is a recent discovery in African societies, because previously only women were involved in the cause of infertility [8] [9] .
To assess male infertility, the spermogram is an efficient baseline paraclinical investigation that allows for etiological exploration and directs prescribers towards other complementary workups. Male infertility may result to quite complex moral repercussions on the individual, the family and society, particularly with regards to marital dynamism [9] . There is paucity of data on the etiological and clinical aspects of male infertility in our setting [1] [10] [11] [12] [13] . We aimed at studying the epidemiological and clinical aspects of male infertility in patients consulting at the Urology Department of the Yaounde Central Hospital (YCH), more specifically, the sociodemographic profile and clinical characteristics of men suffering from male infertility in the Urology Department of the YCH.
2. Methods
2.1. Study Type, Duration, Period and Site
We carried out a descriptive cross-sectional study for 7 months, with retrospective data collection over 5 years and 3 months (from January 1, 2016 to April 30, 2021), at the Urology Department of the HCY. Created in 1933, the Yaounde Central Hospital is a second category reference hospital, which contains 33 admission beds within its Urology department. The department is managed by urology professors, specialists and residents undergoing specialization.
2.2. Sampling
The study population consisted of men who had been followed at the Urology Department of the YCH for male infertility. Any patient’s file with diagnosis of infertility and presenting with spermogram results was included. Any incomplete file for which the patient contacted by telephone refused to provide verbal consent was excluded. The minimum sample size was calculated using the
Cochrane’s formula:
with n as minimal sample size,
d as level of precision = 5%, Z as standardized significance level = 1.96, and p = prevalence of male infertility in the sub-Saharan African population = 5.68% [14] . After numerical application, n= 83. To increase the reliability of our results, we exhaustively recruited all cases that met our selection criteria.
2.3. Procedure
After obtaining ethical clearance and research authorization from the YCH administration, we went to the urology department. From admission, consultation and/or hospitalization registers, names and information of patients followed during the study period for infertility were identified. A thorough search of their files at the hospital archives was done. In case file reported information was incomplete and patient’s contact was available, patients were contacted to obtain their verbal informed consent and complete the information. All information was reported on a structured and pre-tested data collection form. Studied variables were sociodemographic, anthropometric (Body Mass Index (BMI)), past history with comorbidities, clinical characteristics and etiologies of male infertility.
During the study, infertility was defined as the inability to achieve pregnancy after 12 months or more of regular, unprotected sexual intercourse by a couple of childbearing age [15] . It was classified as primary if there was no pregnancy after a minimum of one year of regular unprotected sexual intercourse in a couple in which the woman had never been pregnant [16] , and secondary if it was impossible to obtain a new pregnancy for a couple who had already conceived a pregnancy in the past. Male infertility was referred to as the inability of a man to procreate due to an abnormality in his sperm [8] .
2.4. Data analysis
Data reported on data collection forms were entered into a data entry form designed on CSPro software version 7.2. The database was later exported for descriptive statistics using the IBM SPSS software version 23. Qualitative variables were summarized in frequencies and percentages while quantitative variables were summarized in means with their standard deviations for normally distributed data, or medians and interquartile ranges otherwise.
2.5. Ethical Considerations
We had obtained ethical clearance No. 2884 CEI-Udo/08/2021/T of August 2, 2021 from the Institutional Research Ethics Committee for Human Health of the University of Douala, as well as authorization from the administration of YCH. Technical sheets were anonymous, and data were confidential and reserved solely for science. For patients contacted by telephone to complete the technical sheets, their consents were required and they were free to withdraw it at any time.
3. Results
Of the 263 patients treated at the YCH Urology Department, 148 files were found at the hospital archives, of which 38 patients among those contacted by telephone refused to provide their consent. We thus retained and analyzed 110 files. The median age was 37.0 years, with an interquartile range of 8.3, a minimum and maximum of 27 and 59 years respectively.
Epidemiological characteristics of male infertility
The epidemiological characteristics of the participants are shown in Table 1.
Of the 110 patients, 95 (86.4%) were married, 58 (52.7%) were from the Western region, 76 (69.1%) were employed, the history found was dominated by mumps, 40 (36.4%) and hypertension 6 (5.5%), varicocele surgery 25 (22.7%), alcoholism 87 (79.1%) and smoking 15 (13.6%).
Clinical characteristics of male infertility
The spermogram abnormalities, the different etiologies and the types of male infertility found in our study are shown in Table 2.
Table 1. Epidemiological characteristics of male infertility.

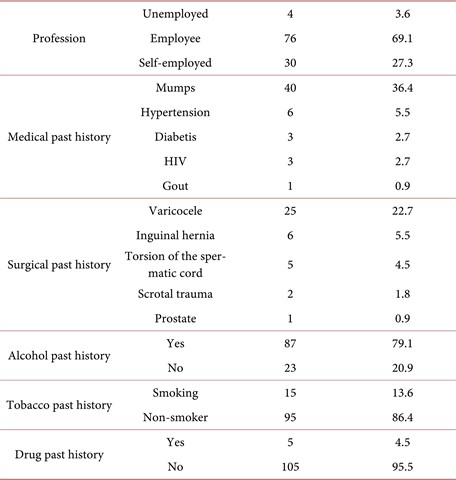
Table 2. Distribution of patients according to abnormalities found on the spermogram, etiologies, BMI and type of infertility.
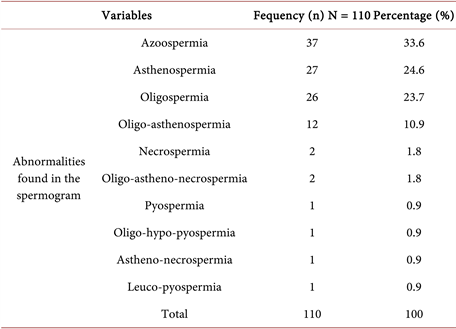
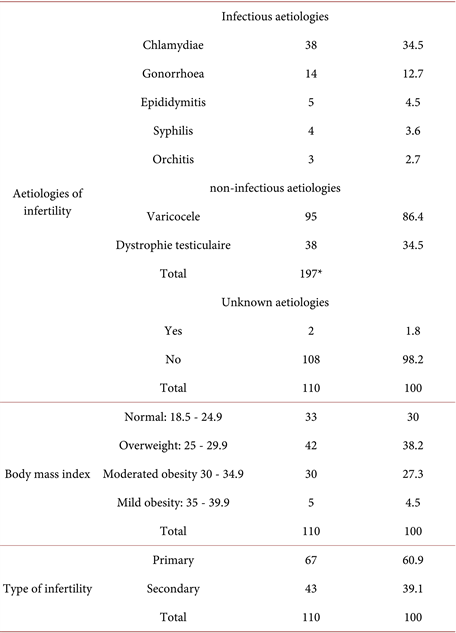 *Several etiologies were found in certain patients.
*Several etiologies were found in certain patients.
Spermatogenesis disorders were found in all our patients. The most common abnormalities found on the spermogram were azoospermia, asthenospermia, oligospermia and oligo-asthenospermia with the respective numbers of 37 (33.6%), 27 (24.6%), 26 (23.7) and 12 (10.9%). As for the etiologies, Chlamydia and gonococcal infections were the most common infectious etiologies with 38 (34.5%) and 14 (12.7%) respectively. For non-infectious etiologies, varicocele was found in 95 (86.4%) patients, followed by testicular dystrophy in 38 (34.5%) patients. No etiology was found in 2 (1.8%) patients. Overweight patients represented 38.2% and those with mild and moderate obesity represented 27.3% and 4.5%, respectively. Infertility was primary in 67 (60.9%) patients.
4. Discussion
Out of 263 files found at the Urology Department of the YCH, we were only able to use 110 (41.8%) files. This is an inherent characteristic of retrospective studies in our context. However, we believe that our study is reliable because we exceeded our minimum sample size.
4.1. Socio-Demographic Profile
The median age was 37.0 years. The most represented age group (30 - 39 years) was identical to that found by Sankare in Bamako [8] . The 84.6% of married men found in our study (Table 1) is higher than the 62.9% found by Ashifatu in 2006 at the Cocody University Hospital in Ivory Coast [17] . This could be explained by the fact that the desire to procreate is more felt when one is married as having a child becomes the couple’s next objective. The dominant regions in our study (west and center) were also found by Noubom et al. [1] in Cameroon. In our study, 69.1% of participants were employees (Table 1). This could be explained by the fact that they have means to go to the hospital. This result is different from 47.8% found by Fizazi in 2014 in Algeria [11] in the informal sector.
In our study, 11.8% of our patients presented co-morbidities. The past history found was dominated by mumps: 40 (36.4%) and hypertension: 6 (5.5%). Sankare [8] found the history of mumps in 24.0%, the history of hypertension in 5% of patients, and diabetis in 2%. Mumps can have repercussions on the testicles by causing their atrophy, especially when it occurs in adulthood. Hypertension in men leads to a lower than normal sperm volume, reduced sperm motility and number [18] , and one of the complications of diabetes is the disruption of the male reproductive system and spermatogenesis [19] .
The other past history was dominated by surgery for varicocele 25 (22.7%), alcoholism 87 (79.1%) and smoking 15 (13.6%) (Table 1). This would mean that up to 22.7% of patients who have had varicocele surgery have an unresolved infertility problem. This result agrees with that found by Mohammed Frikh et al. in 2019 in Morocco [20] who found a history of varicocele in 25% of patients and is lower than the 44.7% found by El Hajjami in Morocco in 2017 [17] . Gueye et al. showed that 30.77% of patients who benefited from varicocele treatment did not have an improvement in their sperm parameters. The duration of progression of the disease largely determines the disturbances in the spermogram. Hence the need for early treatment of varicocele in order to preserve the chances of fertility [21] . In Sangare's series in Bamako in 2009 [8] smokers represented 30%. There is a passage of the blood-testicular barrier of certain substances contained in cigarette smoke. These lead to an alteration of classic sperm parameters and the nuclear quality of spermatozoa. Smoking also has repercussions on the offspring of these smokers: poor quality embryo, development of certain cancers in early childhood [22] . Heavy alcohol consumption reduces testicular endocrine secretion and plays a harmful role in spermatogenesis [23] . Fizazi in 2014 in Algeria [11] found 2.0% and EL Hajjami in 2017 in Morocco [17] found 2 and 8.1% of alcohol consumers respectively. This difference lies in the fact of differences in cultures and religions across Africa.
4.2. Clinical Features
In the spermogram, the most frequent abnormalities (Table 2) in our patients were also found by Nana et al. in Cameroon in 2007 [13] , Gainsi in Cotonou in 1990 [24] and Moussa D et al. in Niamey in 2015 [25] . This could be explained by the high frequency, in our context, of sexually transmitted infections that are often mistreated. Noumi et al. in Bansoa in 2008 [26] had a predominance of asthenospermia at 21.1%, and Niang et al. in Senegal in 2009 [27] found oligospermia at 28.6% as the first abnormality in the spermogram. These differences can be explained by the fact that although the spermogram is the key test for exploring male fertility, its sensitivity and specificity in the diagnostic approach remain moderate given the possible limits of its interpretation [28] .
Chlamydia and gonococcal infections were the most common infectious etiologies with 38 (34.5%) and 14 (12.7%) respectively (Table 2). Frikh et al. [20] in 2019 in Morocco and Fizzazi in 2014 in Algeria [11] found infection rates of 22.4% and 22% respectively.
For non-infectious etiologies, varicocele was found in 95 (86.4%) patients, followed by testicular dystrophy in 38 (34.5%) patients (Table 2). Several authors have found these two non-infectious etiologies to be dominant [1] [8] [10] [20] . According to the WHO, varicocele is associated with sperm abnormalities, a reduction in testicular volume and a deterioration in Leydig cell function [29] .
In our study, overweight patients accounted for 38.2% and those with mild and moderate obesity accounted for 27.3% and 4.5%, respectively (Table 2). In Fizazi's study in 2014 in Algeria [11] , 50% of patients were overweight. A meta-analysis carried out in 2013 on 14 studies highlighted an increased risk of oligospermia or azoospermia in cases of high BMI [30] . We found no cause of infertility in 1.8% of cases (Table 2), a percentage much lower than the 29% found by Fizzazi et al. [11] . We found primary type infertility in 60.9% of patients (Table 2), a frequency close to 62% found by Mohammed et al. in 2019 [20] and 66.5% found by Niang et al. in Senegal in 2009 [10] . Couples without children tend to consult more often than others to treat their infertility.
4.3. Limitations of the Study
We only found the files of 110 patients (or 41.8%) out of the 263 treated in the department. However, we believe that our study is reliable because we exceeded the minimum sample size. For patients contacted by telephone, there could be recall bias.
5. Conclusion
Married people made up 86.4% of our sample, the history found was dominated by mumps and hypertension, history of surgery for varicocele, alcoholism and smoking. A spermatogenesis disorder was found in all our patients, dominated by azoospermia, asthenospermia, oligospermia and oligo-asthenospermia. Chlamydia and gonococcal infections were the most common infectious aetiologies. For non-infectious etiologies, varicocele and testicular dystrophy dominated. Overweight patients represented 38.2% and those with mild and moderate obesity represented 27.3% and 4.5% respectively. Infertility was primary in 67 (60.9%) patients. Continuing training of staff, intensification of campaigns for provider behavior changes communication and health promotion focused on comorbidities and early detection of spermogram abnormalities would make it possible to reduce the frequency of male infertility. Computerization of the archiving service could lead to properly preserve patient data.
Authors’ Contributions
Mbassi, Fouelifack Ymele, Dongmo Tiodjou and Maguira Dehukwe designed the study, recruited, analyzed the data and wrote the manuscript. Biwole Sida designed the study and supervised the process until manuscript submission.
Acknowledgements
We thank the YCH administration for allowing us to carry out this study in their facility, as well as the staff of the Urology Department who made the registers and patient files available to us. Finally, our thanks go to the patients who contacted us by telephone and allowed us to complete the information.