Epidemiological Profile and Location of Lesions According to #ENZIAN of Patients Operated on for Endometriosis in a Public Endoscopic Surgery Centre, Yaounde, Cameroon ()
1. Introduction
Endometriosis is the ectopic presence of endometrial tissue outside the uterine cavity [1] [2] [3] . It is a frequent, chronic, inflammatory and hormone-dependent disease in women of childbearing age. Endometriosis is a heterogeneous disease, with five often associated forms: superficial peritoneal endometriosis, ovarian endometrioma, deep pelvic subperitoneal endometriosis (EP), adenomyosis and extra-pelvic endometriosis. The widespread use of laparoscopy in the practice of gynaecology means that this pathology can be better explored. After the clinical decision to perform a diagnostic laparoscopy, the second decision is whether surgery will be performed during this intervention or postponed for a second intervention, eventually after referral. When surgery is anticipated, it is important to estimate the surgical difficulty and risks, and the anticipated type of surgery. These are needed to inform the patient, obtain informed consent and plan the intervention, call for a classification system, that includes all aspects of the disease such as peritoneal endometriosis, ovarian endometriosis, deep endometriosis, and secondary adhesions and also be easy to use. In the past, several systems have been created to describe the anatomical extent of endometriosis [4] ; more than twenty classifications have been published, three of which are the most widely accepted and used: revised American Society for Reproductive Medicine (rASRM) classification; Endometriosis Fertility Index (EFI) and the Enzian classification [4] . The rASRM classification has shown its limitations in describing deep endometriosis [4] ; on the other hand, the Enzian classification, which has recently been updated and modified under the name #Enzian, has proved to be the most effective tool for classifying deep endometriosis and now takes account of locations: peritoneal, ovarian, tubal and also adhesions. As this pathology is still relatively unknown in underprivileged areas, we set out to determine the epidemiological, clinical profile and if of patients operated on in CHRACERH, Yaounde-Cameroon.
2. Materials and Methods
We conducted a cross-sectional analytical study with retrospective data collection. We collected data from patients who underwent laparoscopy for treatment of endometriosis over a period of 05 years (from 1 January 2017 to 31 March 2022): Patients diagnosed with endometriosis by laparoscopy; Patients with a usable laparoscopic videography and whose laparoscopic reports were available; the sampling was non-probabilistic, consecutive and exhaustive, with a minimum of 159 patients; Socio-demographic data were obtained using medical records, supplemented if necessary by telephone calls; lesion location was based on ultrasound data, magnetic resonance imaging (when available) and laparoscopic lesions were located using the nomenclature of the #ENZIA classification, which is the most recommended to date [4] . The locations of the various endometriotic lesions are indicated in capital letters (see Figure 1):
· P for peritoneum;
· O for ovary;
· T for the tube;
· A for the vagina, rectovaginal space and retrocervical space;
· B for the uterosacral ligaments, cardinal ligaments and lateral pelvic wall;
· C for the rectum;
· F for other locations (FA: adenomyosis; FB: bladder; FI: intestine; FU: ureter).
The Quantitative variables were expressed as means with standard deviations and qualitative variables were expressed as numbers with their percentage. The data was analysed using Cs Pro 7.0 and SPSS 23.0;
3. Results
In total, we were able to use 159 patients’ files and videos during our study period.
3.1. Epidemiology Profile
The mean age of the study population was 32.9 ± 5.9 years with extremes ranging from 18 to 48 years; the most represented age group was [30 - 40[, i.e. 53.5% of cases with a median of 32 years. More than half were single, i.e. 82 (51.6%) and 81 (50.9%) patients worked in the public sector. West Cameroon was the
![]()
Figure 1. Laparoscopic view of the different #Enzian sites.
most represented region, i.e. 43.4% (n = 69) of cases. The majority of the population had a secondary education, i.e. 49.1% (n = 78) of cases; the Catholic religion was the most represented, i.e. 61.0% (n = 97) of cases (see Table 1).
![]()
Table 1. Epidemiological profile of patients.
3.2. Clinical Profile of Patients
3.2.1. Patient History
In our study, the majority of patients were nuligravid in 61.6% (n = 98) of cases; furthermore, the mean age at menarche was 11.9 ± 0.9 years with extremes ranging from 9 - 16 years; the mean duration of menstruation was 4.2 ± 0.7 days with extremes ranging from 2 - 6 days, and the mean duration of the menstrual cycle was 28.8 ± 1.04 days with extremes ranging from 25 - 34 days. 48 patients (30.2% of our sample) had a history of infection, the most frequent being chlamydia. In our study 13 patients (8.18%) had a history of gynaecological surgery, the most frequent of which was myomectomy by laparotomy (3.18%) (see Table 2).
3.2.2. Diagnostic Approach and Localisations of Endometrioses
Infertility was the most frequent reason for consultation, in 72.3% (n = 115) of cases, followed by dysmenorrhoea in 60.8% (n = 96) of cases and chronic pelvic pain in 37.7% (n = 60). A further 46 (28.9%) patients complained of profound dyspareunia, 17 (10.7%) of dyschezia and 9 (5.7%) of dysuria (see Table 3).
In our series, adenomyosis was diagnosed on pelvic ultrasound in 100% (n = 24) of patients and ovarian endometriomas in 57/61 (93.4%) patients (see Table 3
![]()
Table 2. Breakdown of patients according to previous history.
![]()
Table 3. Distribution of the population according to the most frequent symptoms of endometriosis and investigations done.
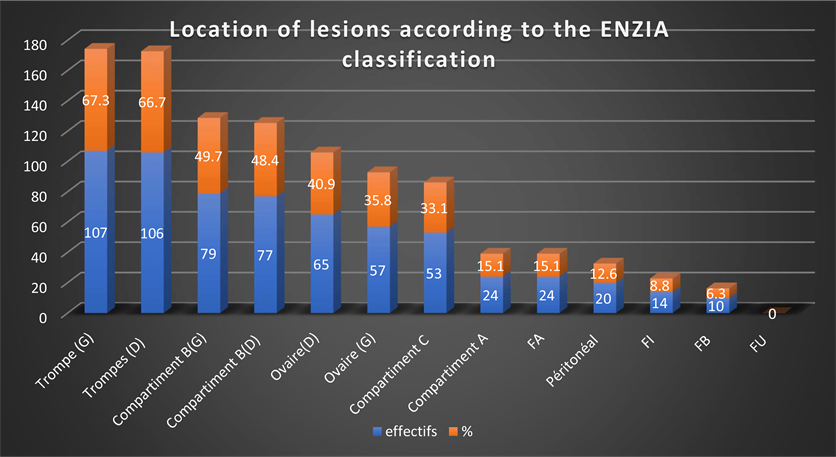
FU: ureteral location; FB: bladder location; FA: adenomyosis; FI: intestinal location: Compartment A: recto-vaginal septum, Compartment B: utero-sacral, proximal and distal parametres, Compartment C: rectum.
Figure 2. Distribution of endometriosis lesions in the study population according to the #ENZIAN classification.
and Figure 2). Magnetic Resonance Imaging (MRI) was used as a diagnostic tool in only one patient. In the absence of lesions on imaging, diagnostic laparoscopy was performed immediately in 77 (48.4%) patients.
Tubal lesions were the most common, 66.7% (n = 106) on the right and 67.3% (n = 107) on the left. This was followed by Compartment B (uterosacral ligaments, cardinal ligaments and lateral pelvic wall) 48.4% (n = 77) on the right and 49.7% (n = 79) on the left, endometriomas 40.9% (n = 65) on the right and 35.8% (n = 57) on the left (see Figure 2).
4. Discussion
Endometriosis is one of the common diseases with the longest delay in diagnosis [1] . This delay exacerbates the disease and its consequences. The widespread use of laparoscopy in the practice of gynaecology means that this pathology can be better explored. Our study of the epidemiological and clinical profile of patients operated on for endometriosis at CHRACERH also revealed a late recourse to treatment, with an average age of 32.9 ± 5.9 years. Our results are similar to those of Belletis et al. [5] in 2010 who found an average age of 33.2 ± 6.3 years in patients treated for pelvic endometriosis in Brazil and those of Bilkissou et al. [6] in the city of Douala (Cameroon) who found an average age of 34.65 ± 6.7 years. This can be explained by the fact that 2 out of 3 women are unaware of the existence of endometriosis [7] and therefore the diagnosis is generally made an average of 8 - 12 years after the onset of symptoms [1] .
Endometriosis is often associated with infertility, and was the most frequent reason for consultation in our series. As a result, 61.6% of the women in our study population were nulliparous, a result slightly higher than but in line with that of Belletis et al. in 2010 in Brazil, who found a percentage of 56.5% nulliparous [5] , and Boumaraf et al. in 2021 in Algeria, who found a percentage of 50% nulliparous [8] —this difference may be explained by the fact that we recruited our patients from a reference centre for human reproduction.
Endometriosis was discovered in 72.3% of cases during infertility treatment. This is significantly higher than the results found by Haas et al. [9] in 2013, who found infertility in 40.71% of cases, and Belletis et al. [5] in 2010, who found infertility in 39.8% of cases. Apart from the fact that this proportion can still be justified by the location of the study, this difference draws attention to the trivialisation of the symptoms of endometriosis in a disadvantaged environment, where the pain associated with dysmenorrhoea has to be borne by the young woman, partly because of beliefs and partly because of the difficulty of accessing information and therefore appropriate treatment. This situation encourages the use of alternative treatments such as herbal medicine or the use of traditional witch doctors [10] . This hypothesis is reinforced by the fact that after questioning, dysmenorrhoea was present in 60.8% of our patients, as found by Belletis et al. [5] in 2010 in Brazil, who found dysmenorrhoea in 62.2% of cases, and by Haas et al. [9] in 2013 in Australia, who found a percentage of 65.71%.
Boumaraf et al. in Algeria in 2021 [8] in a study of the characteristics of endometriosis in their population found that: the most frequent location of endometriosis was ovarian in 50% of cases. This is not in agreement with our results, which revealed tubal lesions, followed by deep endometriotic lesions and then ovarian lesions. This difference could be explained by the fact that our study population consisted of patients managed by laparoscopic surgery, and that not all endometriomas are managed by laparoscopy after a positive ultrasound diagnosis.
Imaging is the method of choice for diagnosing cystic ovarian endometriosis, adenomyossis and suspecting deep endometriosis. However, neither clinical exam nor imaging can exclude smaller and superficial lesions [11] . In our study, only one patient underwent preoperative MRI, justified on the one hand by the absence of a radiologist with endometriosis expertise in our context, and therefore increa risk of false negatives, and on the other hand by the additional cost of this examination, bearing in mind that diagnostic laparoscopy is part of the management protocol. All the patients had undergone transvaginal ultrasound (TVS) to identify cases of adenomyosis and endometriomas. No transrectal ultrasound was performed. A common mistake is that endometriosis can be excluded because of negative exams including imaging resulting in the well-known diagnostic delay of diagnosis in endometriosis.
Therefore, the indication to perform a laparoscopy because of suspected endometriosis remains a clinical decision, knowing that a woman with infertility or chronic pain has a 50% probability of having typical endometriosis and over 70% of having subtle lesions. In our context it was a population of women in 52% infertile, on average at an advanced age justifying the immediate performance of a laparoscopy to treat as far as possible infertility problems or pain syndromes not giving in for to usual therapies.
Concerning deep endometriosis lesions, compartment B was the most affected compartment, i.e. 49.7% on the left and 48.4% on the right. This result is equivalent to that found by Haas et al. [12] who found a predominance of deep endometriosis lesions in compartment B in 64.4% (this study was carried out using the old Enzian classification in which compartment B was not separated into 2).
Concerning deep endometriosis lesions, compartment B was the most affected compartment, i.e. 49.7% on the left and 48.4% on the right. This result is equivalent to that found by Haas et al. [12] who found a predominance of deep endometriosis lesions in compartment B in 64.4% of cases (this study used the old Enzian classification in which compartment B was not separated into 2). Followed by compartment A in 15.1% of cases, this result, although lower than that found by Haas et al. [12] in 2013 which was 40.71%, is the second compartment affected by deep endometriosis in our study.
The high prevalence of deep endometriotic lesions reflects the advanced forms at the time of diagnosis in our context, but also the physical and psychological suffering that these patients may experience as a result of ignorance or inaccessibility to quality care.
5. Limitations of the Study
The financial cost of MRI did not allow it to be carried out systematically in all patients. Also the retrospective nature of the study did not guarantee a methodical and systematic exploration of all endometriosis sites.
6. Conclusion
The women operated on for endometriosis were of a more advanced age, and predominantly nulliparous. Infertility was the most frequent reason for consultation despite the fact that they present with other symptoms of endometriosis which are not the main reason for consultation. According to #ENZIAN classification, the tubal location most frequently encountered for superficial lesions, followed by Compartment B and endometriomas.