Effectiveness of an Educational Intervention for Postpartum Depression in a Pre-Parent Classroom ()
1. Introduction
Postpartum depression is a severe public health problem with a global incidence of approximately 10% - 20%. Contributing factors include history of depression, marital status, antenatal emotional status, and parenting stress [1] [2] [3] . As postpartum depression can lead to suicidal ideation in women and disrupted attachment formation due to the limited ability to perform maternal roles [4] , efforts are necessary to prevent postpartum depression during gestation.
In Japan, the “Maternal Health Checkup Project” was launched in 2017 for suicide prevention and understanding pregnant women’s mental health. Screening is recommended during the two-week and one-month postpartum check-ups. Once high-risk expectant mothers are identified through a diagnosis of mental illness, local government agencies and hospitals collaborate to support them as at-risk expectant mothers (i.e., requiring extra support after birth due to factors such as unstable income or mental illness) [5] . However, a drawback of this approach, which targets all pregnant and nursing mothers, is that its efforts are less visible and less valued, which is why proactive support is necessary [6] . Proactive support should be targeted to all women, as many perinatal women are less likely to seek help themselves [7] .
Cognitive-behavioral and interpersonal therapies have proven effective in preventing postpartum depression [8] . These therapies are effective for high-risk pregnant women with mental disorders [9] and often require specialized knowledge; however, limited research has investigated their effectiveness for low-risk pregnant women. Furthermore, general pregnancy health education typically focuses on pregnancy and childbirth processes [10] ; it lacks content on perinatal mental health [11] . In Japan, it is recommended that pregnant women and their families be provided with opportunities during pregnancy to learn about postpartum mental health; however, this is currently performed in only 49% of Japanese municipalities [12] .
Lack of partner support [1] is a key factor associated with perinatal depression, and women receiving substantial social support from their partners during pregnancy show lower postpartum psychological distress [13] . In addition, instrumental and emotional support should be encouraged to minimize conflict between fathers and mothers [14] .
Insufficient research exists on postpartum depression among low-risk pregnant women (i.e., those without diagnosed mental illnesses), and little is known about the effects of preventive interventions for promoting communication between couples and preparation for child-rearing among this group. One of the preventive interventions for postpartum depression is improving communication between couples [13] [14] . Therefore, we hypothesized that promoting effective communication between couples would facilitate the prevention of postpartum depression. Specifically, mothers hypothesized that the intervention during pregnancy would reduce 1) parenting difficulties and 2) depression compared to controls. The fathers hypothesized that the intervention group 1) would have fewer parenting difficulties and 2) would cope better if the mothers had postpartum depression than would the control group. It was predicted that as fathers’ feelings of difficulty in child-rearing (including marital relationships) decreased, mothers’ feelings of difficulty in child-rearing and depression would also decrease. This study has scientific value and contributes to the development of the next generation by providing guidelines for married couples. Thus, we examined the effects of a mental health program for expectant couples focused on providing information for the prevention and early detection of postpartum depression.
2. Methods
2.1. Research Target
This study was conducted with couples from pregnancy to one month postpartum. Participants were first-time mothers and their partners who, after 16 weeks of pregnancy, participated in a “First-Time Parenting Class” commissioned by City A and conducted by the Midwives Association. Inclusion criteria were couples who consented to the study, could understand Japanese, and had a single pregnancy. Pregnant women with mental illness were excluded.
2.2. Intervention Methods
The one-time class, designed for couples, lasts approximately 2.5 h. For fathers, the program includes pregnancy experience, baby-holding experience using a doll, bathing, and explanations of various notifications and health services; for mothers, it includes opportunities to interact and exchange information with other pregnant women. The lecture content, presented by midwives, includes physical changes during pregnancy and fetal development, the father’s role during childbirth, and newborns’ characteristics and care. In this study, the booklet “Mental Health for Parents-to-Be” was only distributed to the intervention group (IG) and was partially explained using seven presentation slides. Approximately 12 min were required for the explanation, delivered by the primary investigator or two sub-researchers. We wanted to provide postpartum depression information and encourage fathers to communicate with mothers. The presentation content has been previously reported [15] and is presented in Table 1.
2.3. Survey Period and Data Collection Method
A quasi-experimental research was conducted with a control group (CG) from July 2015 to April 2016 and the IG from June 2016 to July 2017. A randomized controlled trial was not conducted to avoid creating issues in the group if some
![]()
Table 1. Content of education interventions.
couples received materials that others did not have. Couples who agreed to participate completed a pregnancy questionnaire that was collected at the start of the class. The second questionnaire was distributed and collected via mail, one month postpartum from the expected date of delivery.
2.4. Survey Details
2.4.1. Recognition of Postpartum Depression and Information Sources (Mothers and Fathers, Pregnancy Period)
Both mothers and fathers chose from three options regarding their awareness of postpartum depression: “I know the term well,” “I know the term,” and “I do not know the term.” Those who answered “I know the term well” indicated their information sources. Content validity was verified by two researchers who were midwifery faculty members.
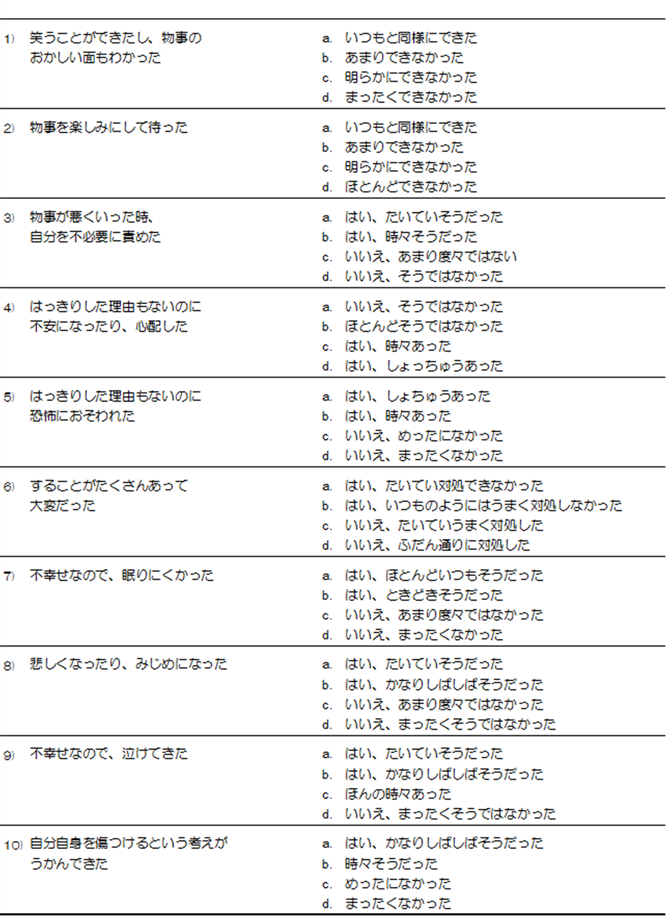
2.4.2. Depression State (Mothers Only, During Pregnancy and One Month Postpartum)
The Edinburgh Postnatal Depression Scale (EPDS) is a quantitative measure developed by Cox et al. [16] , and the Japanese version was developed by Okano et al. [17] . The EPDS is a 10-item, 4-point (0 to 3) self-report questionnaire, with scores ranging from 0 to 30. Cronbach’s alpha was 0.67 one month postpartum [17] . A border value of 8 - 9 indicates high validity with a sensitivity of 0.75 and a specificity of 0.93. A score of 9 or higher indicates possible postpartum depression. In this study, Cronbach’s alpha was 0.822 during pregnancy and 0.847 one month postpartum.
2.4.3. Child-Rearing Difficulty (Mothers and Fathers, One Month Postpartum)
For mothers, we assessed their sense of child-rearing difficulty using the Japan Child and Family Research Institute (JCFRI) Child-Rearing Support Questionnaire (Millennium Version) [18] .
Previous studies have confirmed that postpartum depression is related to challenges in child-rearing [19] . This scale is divided into five domains—Domain 1: child-rearing difficulties; Domain 2: problems with husband/father/family functioning; Domain 3: mother’s anxiety/depressive tendencies; Domain 4: husband’s physical and mental disorders; and Domain 5: difficult baby. Each domain is scored on a 4-point scale (1 - 4); the higher the score, the worse a family’s performance in a particular domain. In a previous validation study, Cronbach’s alpha ranged from 0.85 or more for each item [19] . In this study, Cronbach’s alpha ranged from 0.877 to 0.915 and was 0.647 for the “difficult baby” subscale.
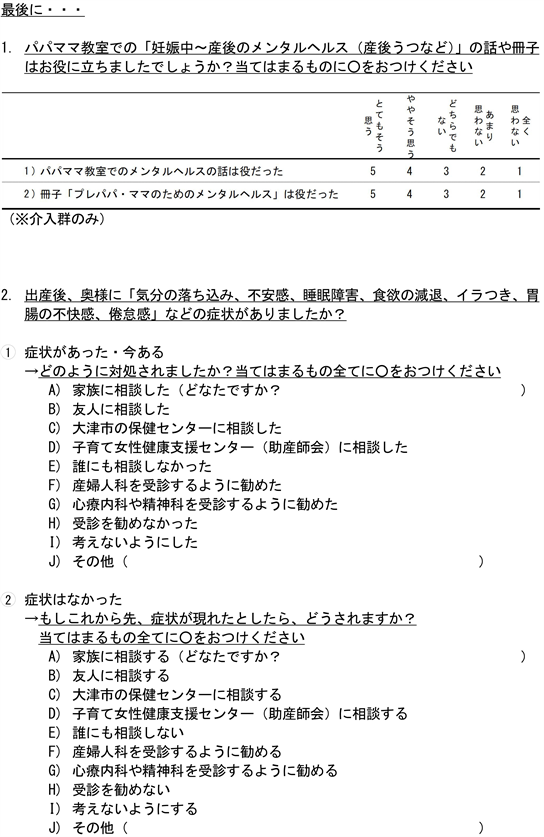
The JCFRI Child-Rearing Support Questionnaire for Fathers [20] was used for fathers. This scale comprises five domains; we used Domain 1: child-rearing difficulties; Domain 3: father’s anxiety and depression; and Domain 4: the state of the marital relationship. Domain 2: related to child abuse, and Domain 5: requiring an interview, were excluded. Each domain is rated on a 4-point scale (1 - 4), with higher scores on Domains 1, 3, and 4 indicating poor performance. Cronbach’s alpha ranged from 0.803 to 0.908 [20] . In this study, it ranged from 0.835 to 0.903.
2.4.4. Coping Strategies and Information Helpfulness When Mothers Show Depressive Symptoms (Fathers, One Month Postpartum)
Regarding measures taken when mothers are perceived to be depressed, fathers chose multiple responses from various options: “Consult,” “Avoid thinking about it,” and “Did not recommend the mother to consult a doctor.” The IG rated the effectiveness of the booklet and mental health talk on a 5-point scale, ranging from “very helpful” to “not helpful at all.” In this study, content validity was verified by two researchers who were midwifery faculty members.
2.5. Ethical Considerations
This study was conducted after obtaining approval from the research ethics review board of the Faculty of Medicine, University of Tsukuba (approval number: 1102), Shiga University of Medical Science (Approval number: 26-17).
The study purpose, measures taken for privacy protection, an explanation that study participation was voluntary, and that there was no penalty associated with withdrawing during the study were expressed verbally and in writing, and all participants provided written informed consent.
2.6. Sample Size
The sample size was calculated by effect size d = 0.5, α = 0.05, power = 0.8 and an allocation ratio = 1 to compare perceptions of child-rearing difficulties in terms of the results of the independent t-test. The required sample size was 128 couples, one month postpartum; however, considering a 70% dropout rate based on Iwahuji and Muto [21] , we recruited 600 couples.
2.7. Statistical Analysis
First, basic statistics were calculated, and a histogram was generated to confirm a normal distribution of the data. Then, for intergroup comparisons, variables with normality were analyzed using Student’s t-test. Finally, the χ2 and Fisher’s exact probability tests were used for percentage comparisons, and the McNemar test was used for before/after comparisons. SPSS Version 27.0 was used for all analyses, and a p-value < 0.05 was considered statistically significant.
3. Results
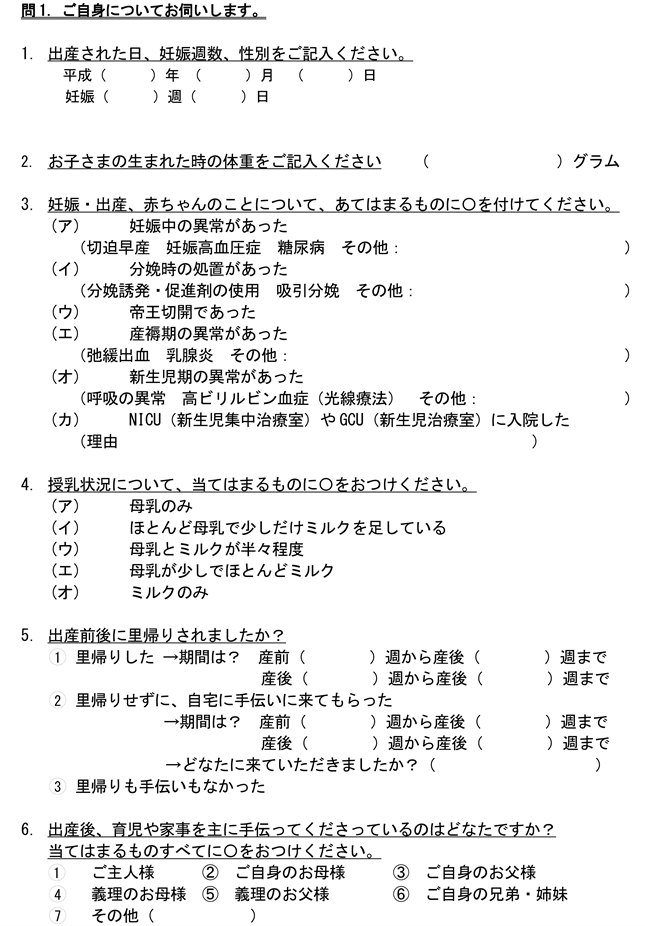
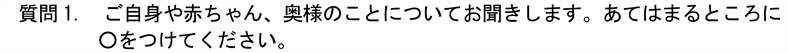
Questionnaires were distributed to 640 couples and returned by 574 couples before attending the parenting class. We lost 277 couples to follow-up in the first month postpartum. Only complete data from the gestational period and the first month of the puerperium of the paired couples were included in the analysis. Thus, in the end, we analyzed data from 158 couples (CG = 86, IG = 72, effective response rate: 27.5%) (Figure 1).
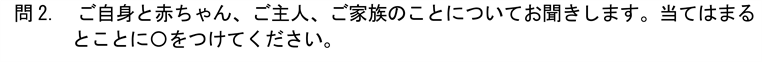
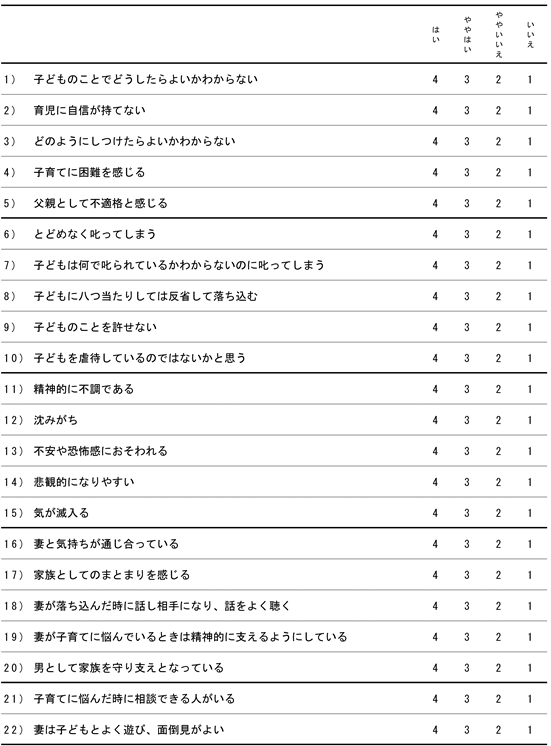
Table 2 shows participants’ socio-demographic and pregnancy- and delivery-related characteristics, pre- and one month postpartum. Further recognition of postpartum depression was checked before the intervention, but there was no difference between the two groups, “I know the term well,” was CG 54.7%, IG 52.8% (p = 0.81) for mothers and CG 24.4%, IG 30.6% for fathers (p = 0.39) (Table 3). Although randomization was not possible, comparison was made because there was no significant difference between the IG and CG.
![]()
Figure 1. Number of individuals in the control group (CG), intervention group (IG), and dropouts.
![]()
Table 2. Basic attributes of the participants (intervention group, control group).
aStudent’s t-test, mean ± standard deviation; bχ2 test; cFisher’s exact probability test; One month of breastfeeding was analyzed with or without breastfeeding. CG = Control group; IG = Intervention Group; Satogaeri childbirth = returned to their parental home to give birth; NICU = Neonatal intensive care unit.
![]()
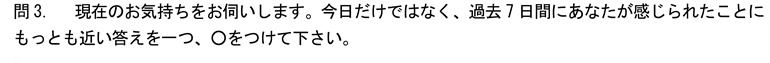
Table 3. Recognition of postpartum depression and information sources.
CG = Control group; IG = Intervention group; Knowledge was assessed based on participants’ responses to the following three options: “I know the term well,” “I know the term,” and “I do not know the term” or no answer. For Sources, multiple responses allowed only for those who answered “I know the term well.” regarding their knowledge. Knowledge was analyzed based on participants’ response to the following response options: “I know the term well,” vs. “I know the term,” “I do not know the term,” and no answer. aχ2 test; bFisher’s exact probability test = effect size (w).
![]()
Table 4. Maternal depression state, maternal and paternal child-rearing difficulty.
aMcNemar test; bχ2 test; cStudent’s t-test: mean ± standard deviation, effect size χ2 test = effect size (w), Student’s t-test = effect size (r), EPDS = Japanese version of Edinburgh Postpartum Depression Self-Assessment Questionnaire; CG = Control group (n = 86); IG = Intervention Group (n = 72); Pre = Pregnancy; Post = Postpartum.
No significant difference was found between mothers’ child-rearing difficulty (p = 0.23) and depression score rates (p = 0.18) in the first month after childbirth. Similar results were obtained for paternal variables (Table 4).
Regarding measures taken when women showed depressive symptoms, percentage comparisons of coping methods revealed differences between fathers in
![]()
Table 5. Coping strategies and helpfulness of the information provided when the partner displays depressive symptoms.
aχ2 test; bFisher’s exact probability test; effect size χ2 test, Fisher’s exact probability test = effect size (w); Survey of couples, one month postpartum; coping strategies: multiple answers allowed; OB/GYN: obstetrics and gynecology; Mental health talk: Content of intervention.
the CG and IG. “Consult family” (p = 0.035), “consult friends” (p = 0.033), and “consult the city health center” (p = 0.047) were higher in fathers of the IG (Table 5). Comparatively, the most common response for coping methods in both groups was “consult with family” (CG = 33.7%, IG = 54.2%), while “consult with a psychosomatic medicine specialist or psychiatrist” was the least common (CG = 4.7%, IG = 4.2%); however, the effect size was small. Regarding how helpful the discussion on mental health was, 73.6% of IG fathers answered “very helpful” or “somewhat helpful.” Regarding the booklet, 51.4% answered “very helpful” or “somewhat helpful.”
4. Discussion
The average age of mothers during their first childbirth in Japan is 30.7 years [22] , and the number of families living in three-generation households has declined to 10% [23] . The cesarean section rate at delivery is also approximately 10% - 20%, which is similar to the overall delivery situation in Japan [24] . This confirms that the participants’ attributes in our study were representative of the national statistics for first month postpartum in Japan.
In the current study, a higher participant percentage had EPDS scores above 9 during pregnancy compared to previous reports (8.9% - 15.8%) [1] [25] . Depressive tendencies were also high one month postpartum relative to previous research [26] . There was no change in the percentage of EPDS scores above 9 for CG participants (18.1%), while there was a reduction in the one-month postpartum scores for IG participants (23.6% vs. 19.4%). Some previous studies have shown that fewer mothers show depressive tendencies after childbirth than during pregnancy [25] , while others have reported higher depression after childbirth [26] . High scorers might have dropped out and were thus excluded from the analysis, as it would have been challenging for them to continue the program if they had developed postpartum depression one month later. Since an accurate determination of the onset of postpartum depression requires diagnosis by a physician and information provision from and collaboration with medical institutions, this is a limitation of evaluating interventions through self-report questionnaires, as was undertaken in this study. No significant difference was found in the results of mothers’ child-rearing difficulties between the two groups. The findings regarding mothers’ sense of difficulty in child-rearing (Domain 1) were comparable to the mean values at one month postpartum [27] .
Further, our intervention was based on promoting communication between couples. The father’s “state of marital relationship” variable was not significant between the CG and IG. Marital status as viewed by the fathers was similar across both groups to that of low-risk one-month postpartum fathers in a previous study [28] . Since the couples discussed and participated in the event at will, it can be assumed that they originally had a good relationship. Although there was no significant difference in the husband’s mental and physical health problems, both groups scored slightly higher [27] .
A previous study reported that 5.2% of fathers had postpartum depression [29] . However, few intervention studies have focused on postpartum depression in fathers. In our study, the information provided to the IG did not convey the importance of maintaining paternal physical and mental health or its effects on maternal mental health. Medical professionals need to pay attention to mental health among fathers as it affects maternal child-rearing stress [30] . Therefore, future interventions related to paternal mental health should be considered.
In this study, 39 fathers (54.2%) in the IG answered that they consult their families (p = 0.035). Fathers in the IG were more likely to understand the necessity of taking action if their partners experienced depressive symptoms. Intervention studies to reduce maternal depression have reported no psychological intervention effects from using information booklets before childbirth [31] . Conversely, a study investigating marital relationships reported that problem-focused information and support provided prenatally are invaluable to families [32] . From the results of our study, we could not verify whether fathers could detect maternal depression at an early stage. However, we believe fathers can better understand postpartum depression when provided relevant information. Healthcare personnel provide specific, addressable information to expectant parents, which may prevent perinatal psychological problems and contribute to couple empowerment [33] . Rosenquist [34] suggested that fathers monitor and recognize symptoms of maternal depression. Additionally, this study found that few fathers knew much about postpartum depression. Since mothers with depressive symptoms report lower perceptions of husbands [32] , healthcare providers should encourage fathers to receive support when needed and help them cope with their difficulties. Providing postpartum depression information and helping facilitate marital communication make them more likely to notice changes in their partners early on and seek help from those close to them.
In this study, scores on “consult the city health center” were higher for fathers in the IG than those in the CG (P = 0.047). Mothers and fathers may have been familiar because the midwives organized the parent classes. Individuals with depression often do not seek medical attention due to stigma and personality traits such as self-esteem [35] . Postpartum women may also avoid actively seeking help. Furthermore, families are often reluctant to attend to mothers’ emotional and practical needs [36] .
We predicted that individuals and families might experience stigma related to seeing a psychiatrist.
Hence, when providing this information, we advised participants to first consult someone close to them. Tamaki [37] found that only a few people consulted psychiatrists when physical and mental disorders occurred after childbirth. Therefore, the method of providing information and difficulties in visiting a psychiatrist or psychosomatic medicine practitioner impact the likelihood of mothers developing postpartum depression. Health institutions should continue to provide information on seeking help from medical professionals and identify contact points that are easy to consult, in addition to recommending that parents rely on support from close individuals. However, given the small effect size in this study, further research is needed.
To our knowledge, this study is one of the few to target postpartum depression coping strategies. Another strength is its focus on low-risk participants. Although still an uncommon approach in the field of prenatal interventions, participating men are encouraged to consult with their family, friends, and health centers to help them deal with their partners’ depression.
Strengths and Limitations
This study’s response rate (27.5%) was higher than in Hawkins et al.’s study (25%) [38] . The target population may have been motivated to participate in preparatory education since the parenting classes were held only once a month and on a first-come, first-served basis. On the other hand, each partner had to provide their informed consent; a couple was excluded unless both partners consented. Further, our intervention was conducted during a parenting class; therefore, time constraints were experienced. These circumstances could be mitigated by a more effective approach to implementing parenting classes specializing in mental health programs.
5. Conclusion
In this study, the mothers’ interventions during pregnancy failed to reduce 1) parenting difficulties and 2) depression compared with controls. We found that the fathers’ IG failed to reduce parenting difficulties, but coped better with the mothers’ potential postpartum depression than did the CG. Therefore, one hypothesis was proved. Healthcare facilities must implement parenting classes to increase opportunities to provide information on mental health. In addition to planning parenting classes, antenatal checkups at hospitals, pregnancy notifications at municipalities, and online services could also be used to provide support. The postpartum period and individual-based interventions should also be considered [39] . In this way, fathers will become more knowledgeable about postpartum depression, and relationships between expectant mothers and fathers can be enhanced.
Implications for Practice
IG fathers were more likely to understand the necessity of taking action if their partner showed depressive symptoms. Thus, providing information regarding the prevention and early detection of postpartum depression during pregnancy will deepen parents’ understanding and help them cope with postpartum depression.
Acknowledgements
We would like to express our deepest gratitude to the Shiga Prefecture Midwives’ Association for allowing us to conduct this study and to the couples who cooperated.
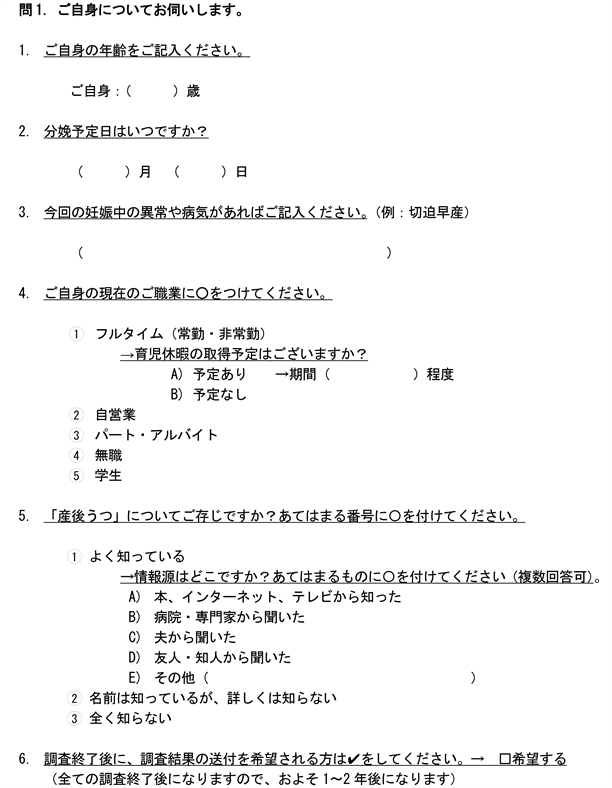
Appendix