The Efficacy and Role of Probiotics for Maintenance of Remission in Crohn’s Disease: A Meta-Analysis and Survey ()
1. Literature Review
Chronic inflammatory bowel disease (IBD) is an umbrella term to describe Crohn’s disease (CD) and ulcerative colitis (UC), two disorders characterized by inflammation in the gastrointestinal tract. Population-based evidence estimates that the global prevalence of IBD has increased by 31% from 1990 to 2017 [1] . A rising incidence rate of IBD burdens countless people with healthcare costs, possible impediments to life aspirations, and impaired quality of life. IBD’s general classification warrants further specification for conducting narrowed research to a subset of IBD, CD. Unlike UC where superficial inflammation occurs in the colon, CD inflammation is transmural and segmented along the entirety of the gastrointestinal tract. This disparity among diseases might explain why treatment methods effective in UC do not have the same capacity for CD patients. While idiopathic, CD appears to be caused by a combination of genetic, immunological, and environmental factors that trigger an overly aggressive immune response to commensal bacteria disturbing intestinal epithelial integrity [2] . The complex interplay among these factors is a key mechanism to understanding CD’s pathogenesis and pathways to its treatment.
CD is classified as a relapsing-remitting disease; therefore, patients experience inflammatory flare-ups with intervening phrases of symptom-free remission. Symptoms and extraintestinal complications include but are not limited to diarrhea, abdominal pain, malnutrition, fistulas, anemia, and aphthous ulcerations [3] . More than 70% of CD patients undergo operations in their lives. New lesions can recur during clinical relapse and possibly necessitate additional procedures. The median time to surgical recurrence is 10 - 20 years, clinical recurrence is 3 - 5 years, and endoscopic recurrence is 6 months [4] . Maintenance and treatment of CD require physicians’ involvement indefinitely, so its impact on the healthcare system will continue to rise exponentially.
Current therapies aim to alleviate symptoms and prevent relapse; consequently, in most cases, drug treatments become a permanent part of individuals’ medical regimens. Drug treatments include traditional anti-inflammatory agents (corticosteroids), immunosuppressants, and biologic therapies that, if successful, will slow the progression of the disease. The most widely accepted treatment approach is a combination of immunosuppressants, where approximately 56% of patients enter corticosteroid-free clinical remission [5] . Long-term, frequent use of many treatment drugs is associated with toxicity and adverse events; thus, there remains a significant outstanding need for safer, effective alternatives to prevent, alter the behavior of, and ultimately cure CD and its accompanying symptoms.
Recently more research has provided a better understanding of the symbiotic relationship between the gut microbiome and the immune system and its responsibility in human health. The gut’s predisposed function to maintain the composition of resident microbiota among the microbiome likely influenced the origin of human immune system homeostasis and subsequent fluctuations [6] . 70% of immune cells reside in the gut, cross-talking between microbes and the immune system to facilitate metabolic and nutritional functions [7] . The gastrointestinal tract provides residency to high concentrations of diverse species of commensal bacteria that normally maintain a symbiotic relationship with the host. The interdependence of the immune system and bacteria warrants the hypothesis that altering the gut flora could rectify malfunctioning immune cells in CD; hence, probiotics have emerged as a potential biotherapeutic.
Probiotics offer an affordable and less invasive alternative to primary methods of treatment. Probiotics are derived from cultured foods to resemble commensal gut bacteria. The live microorganisms potentially yield health benefits for consumers [8] . While the Lactobacillus and Bifidobacterium genus are the most common, numerous single and multi-strain probiotic products exist. The incorporation of probiotics into the therapeutic agenda for CD is based on the theory of dysbiosis, which suggests that intestinal inflammation occurs as a result of an imbalance between commensal and pathogenic bacteria. [9] . High-throughput sequencing instruments have offered insight into the microbial makeup of patients with CD: harmful microbial species (Bacteroides, adherent/invasive Escherichia coli (E. coli.), Enterococci, Pasteurellaceae) are in abundance, and beneficial species (Bifidobacterium, Lactobacillus, Erysipelotrichales, Bacteroidales, and Clostridiales) are depleted [10] . Probiotic products could therefore offer instrumental mechanisms in CD therapy: probiotics compete with microbial pathogens for receptors on epithelium surface; immune system function to stimulate and/or modulate gut-associated tissue cells; suppression of pathogen growth and activity of antimicrobial factors; enhancement of mucosal barrier function intestinal integrity; and induction of T-cell death [11] . Studies of probiotics in animal models with induced colitis have supported these mechanisms of therapy [12] [13] [14] . While animal models administered probiotics have experienced inflammation resolution, limited efficacy has been demonstrated in ulcerative colitis [15] [16] and pouchitis [17] , and no experimental research in CD.
The microbiome possesses tremendous variability; therefore, probiotic therapy cannot be uniform. Probiotic selection and dosage may require adjustment for each patient to be effective. It is also plausible that the health benefits of probiotics position the intervention to adopt a supplementary role to conventional treatments. There is a sound conceptual basis for probiotic intervention to treat CD; however, quality randomized clinical trials (RCT) investigating probiotics’ clinical capacity for reducing relapse and inducing remission are extremely scarce. RCTs must offer insight into the dose, duration of treatment, strains (or combination) used, and timing of intervention during the progression of the disease is necessary.
Currently, no study has yielded evidence to support the use of probiotics for the maintenance treatment of CD, so when linking commercially available probiotics to capacity to treat GI diseases, organizations’ recommendations fail to report on probiotics’ role in CD therapy [7] . Additionally, the majority of CD and probiotic studies identify in the conclusion a demand for quality, large-scale research to adequately reveal probiotics’ efficacy if this beneficial relationship is present [18] . This meta-analysis intends to fill this gap in the literature by gathering a larger quantity of data regarding probiotics’ efficacy in maintaining remission and preventing clinical and endoscopic relapse in CD. Pooling intervention studies, if homogeneity exists, may provide a large sample with sufficient power to demonstrate that this approach to treatment is effective; thus, this investigation could provide clarity into the assertion of the American Gastroenterological Association (AGA) that this was an area lacking in research evidence [19] . Furthermore, while studies have inquired about gastroenterologists’ perceptions on probiotics treatment for all GI diseases, no study has successfully interpreted gastroenterologists’ perceptions and implementation of probiotics in specifically CD treatment [20] . This information can aid the AGA in developing universal probiotic practice guidelines for CD thus providing clarity for the gastroenterology society.
This research aims to provide insight into probiotics’ clinical efficacy and therapeutic role in CD treatment. The interpretation of probiotics’ ongoing relevance in GI practice settings and the pooling of existing research will answer the research question “What is the role of probiotics in the treatment of Crohn’s disease, and are they efficacious in preventing relapse in patients?”
2. Method
2.1. Survey
Online survey tools have historically provided modalities for researchers to assess physician perceptions and practice patterns; thus, a quantitative survey was a logical approach to determine gastroenterologists’ opinions of probiotics for CD [20] . Probiotics are not a standardized treatment for CD; therefore, directly addressing gastroenterologists and inquiring if they have observed any benefits for CD patients is the only way to assess probiotics’ clinical implications.
To address the proposed question, a 15-question survey (Appendix 1) designed to take approximately 3 minutes was distributed through the online platform SurveyMonkey. Survey participation was offered through email to practicing community and academic-based gastroenterologists affiliated with the Crohn’s and Colitis Foundation, Children’s Hospital of Wisconsin, Advocate Aurora Health, GI Associates, Ascension Wisconsin, University of Wisconsin Division of Gastroenterology, and Freoedtert and the Medical College of Wisconsin. The survey was limited to Wisconsin gastroenterologists to focus on a specific geographical area, and within the three week period that the survey was accessible 86 gastroenterologists were reached. The online method provided an organized platform to store response data and maximized accessibility for respondents, increasing convenience and the response rate. Anonymity was maintained to reduce bias and yield responses that accurately reflected participants’ ideologies.
Question design allowed for simple categorization of participants’ responses, 12 questions were multiple choice, two were sliders, and one was an optional text box for providing personal contact information to receive research results. Only close-ended questions were included, although questions allowed respondents to add additional comments regarding their responses to each question. The survey was reviewed independently by an expert in probiotics on the content and format of the questionnaire.
Many of the questions were adapted from a study addressing probiotics as therapy in gastroenterology conducted by a team of researchers in the Division of Gastroenterology at Washington University in St. Louis School of Medicine in St. Louis, Missouri [20] . The first three questions determined gastroenterologist experience, clinical setting, and years of experience. The remaining questions accessed respondents’ perspectives and experiences about probiotics and CD. Physicians were questioned on their familiarity with popular commercially available probiotics as defined by the journal of Microbial Biotechnology: Florajen Products (a blend of Lactobacillus and Bifidobacterium), Align (Bifidobacterium Infantis 35264), Culturelle (Lactobacillus GG), Mutaflor (E. coli Nissle 1917), Fortified Yogurt (DanActive/Yakult/Lifeway/etc.), Florastor (Saccharomyces boulardii lyo), Flora-Q (a blend of 4 species), and VSL#3 (a blend of 8 species) [21] . After gastroenterologists identified the number of patients taking probiotics for CD, they were asked about observed symptom reductions in said patients. Symptoms were modeled off the Crohn’s disease Activity Index [22] .
Descriptive statistics were generated as proportions of respondents and analyzed in a simple analytical method through tables and charts. A minimum sample size calculation procedure was applied and determined to be any sample below a 10% response rate.
2.2. Meta-Analysis
The second component of the study is a meta-analysis of the efficacy of probiotics for the maintenance of remission and prevention of clinical and endoscopic relapse in CD: a potential additional role for probiotics. The proposed question is a medical inquiry whose purpose is to determine a treatment effect; therefore, a rational method to answer this question is apparent in other studies who investigate the treatment effect of an intervention for CD patients. A study determining the efficacy of antibiotics on prevention of relapse utilized a meta-analysis justifying a meta-analysis as the adequate method to determine probiotics’ treatment effect [23] . Experimentation was considered, but a lack of lab resources and qualifications eliminated the methodology. A content review or systematic review could have been conducted; however, this methodology forgoes statistical analysis of outcomes which is necessary to produce an original conclusion concerning the role of probiotics in CD treatment that answers the research question.
The most logical method is a meta-analysis to synthesize outcomes, as there is a limited body of quantitative studies assessing probiotics impact on CD relapse. Currently, no studies individually demonstrate a benefit to probiotic therapy for CD; therefore, this gap justifies pooling results in a single meta-analysis to generate a larger sample size to adequately evaluate if this efficacy exists. This meta-analysis was designed to emulate standard quality meta-analysis protocol as defined by the QUOROM statement checklist: comprehensive set of 21 guidelines published to address standards for improving the quality of reporting of meta-analyses of clinical RCTs and minimizing their susceptibility to bias [24] . Other probiotic efficacy meta-analyses that adhere to QUOROM reporting principles have been published [25] [26] .
2.3. Selection Criteria and Search Method
The inclusion criteria for this review were defined a priori and outlined in Table 1.
Electronic databases and journals were utilized to search for appropriate abstracts or fully published RCTs: National Library of Medicine Pubmed (2000-present), the Cochrane Controlled Trials Register (CENTRAL) (2001-present), Frontiers in Medicine, UpToDate, EMBASE, World Health Organization (WHO) International Clinical Trials Registry, Clinicaltrials.gov, Clinical Gastroenterology, and Hepatology AGA, and Gastrojournal.org to identify comparative studies of probiotics and CD. A text search was conducted using the following keywords: “Crohn’s”, “IBD”, “Probiotic”, “Relapse”, “CDAI”, “Recurrence”, “Lactobacillus”, “Bifidobacterium”, “Saccharomyces”, “Escherichia coli”, and “VSL#3”. Secondary and hand searches were performed on references listed in relevant studies and review articles to identify additional citations not recognized in the initial search. The risk of publication bias was minimized by contacting two experts in the field to determine if they were aware of any additional
or unpublished studies. Finally, the details of identified studies were scanned according to inclusion criteria established a priori.
2.4. Validity Assessment
The Cochrane risk bias tool and Jadad quality score were utilized to assess the methodological quality of identified studies. Bias is determined based on random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective outcome reporting, and other sources of bias. This assessment was then relayed in a risk of bias summary table outlining each domain as judged at low, unclear, or high risk of bias. Jadad quality scores, constructed through assessment of randomization, blinding, and dropouts, were also reported for all RCTs: a score of 0 - 2 indicates a low-quality report and 3 - 5 indicates a high-quality report.
2.5. Data Extraction
An expert in the field conducted a final content review of RCTs identified for inclusion. Information on study design, population, intervention, control, and outcomes were extracted independently from each RCT using a standardized extraction table.
2.6. Analysis
Review Manager (RevMan5.4.1) software on an intention-to-treat basis. Methodological diversity was evident among individual studies; therefore, dichotomous outcome data were pooled using a random effects model to give a more conservative estimate of the effect of probiotics in CD and accounting for heterogeneity between studies. The Mantel-Haenszel method calculated the overall, unconfounded impact of probiotics, compared with a control, as expressed as a relative risk (RR) of relapse of disease activity with 95% confidence intervals (CIs). The respective p-values were assessed at a significance level of 0.05. The objective to differentiate the risk of relapse justifies calculating RRs over odds ratios; further, a RR value of one indicates that there is no difference in risk of relapse between the compared groups. An RR > 1.0 indicates an increase in risk among the exposed (probiotic intervention) compared to the unexposed (control), whereas an RR < 1.0 indicates a decreased risk for the exposed group. Review Manager (RevMan5.4.1) software was utilized to analyze data on an intention-to-treat basis, generate forest plots of pooled RRs, and interpret funnel plots for publication bias.
Calculations of heterogeneity characterize inconsistency within a single meta-analysis, assessing whether the variation across trials is due to true heterogeneity, or chance. Heterogeneity was quantified using the Chi2 test (a P-value of 0.10 was considered statistically significant) and the I2 statistic. An I2 statistic greater than 75% indicated high heterogeneity among studies and if less than 25%, studies demonstrated low heterogeneity [27] . If studies were uniform, the fixed-effect model would have relevance.
Planned subgroup analyses were performed to investigate additional characteristics and factors of heterogeneity potentially relevant to the efficacy of probiotics: endoscopic relapse versus clinical relapse, single-species probiotics versus multi-strain probiotic blends, and probiotic versus placebo as compared to probiotic versus maintenance treatment.
3. Results
3.1. Survey
Of the 86 surveys distributed to Wisconsin gastroenterologists, 32 responded with a response rate of 37%. A notable respondent characteristic was the equal distribution among academic-based gastroenterologists (n = 16) and community-based (private and group practice setting) gastroenterologists (n = 16).
90.6% of respondents cited that probiotics are safe. Figure 1 highlights respondents’ familiarity with commercially available probiotic products. A majority of respondents not only recognized commercial formulations of Florajen, Align, fortified yogurt, and Florastor but also recognized the compounds VSL #3 and Culturelle mostly used in the clinical trial setting. Few respondents were aware of Flora-Q, a discontented probiotic, and Mutaflor, a nonpathogenic E. coli culture more widely recognized in Europe.
![]()
Figure 1. Gastroenterologists’ familiarity with commercially available probiotic preparations.
As demonstrated in Figure 2, 30 respondents felt probiotics could rarely or sometimes be a treatment for CD, and when asked if they foresaw a potential role of probiotics in CD treatment, 37.5% cited yes. Gastroenterologists identified the roles, if any, they believe probiotics could facilitate. Figure 3 denotes 64% believe probiotics function as a supplement to conventional therapies, and 68% recognize probiotics as a modality to alleviate common CD symptoms. 4 respondents skipped the question indicating that the answer selections didn’t align with their ideologies.
The average percentage of gastroenterologists’ patients consuming probiotics is 26%. Figure 4 illustrates the relationship between respondents’ patients with CD taking probiotics and their observed symptom resolutions. Diarrhea, abdominal pain, and general well-being are the symptoms most influenced by the probiotic intervention. Florajen and VSL #3, both multi-strain blends, were the highest-reported probiotics to demonstrate favorable outcomes. The two probiotics respondents were least familiar with, Mutaflor and Flora-Q, had minimal
![]()
Figure 2. Gastroenterologists’ perspective on if probiotics are effective in treating CD or its symptoms.
![]()
Figure 3. Gastroenterologists’ belief of beneficial mechanisms of probiotics.
![]()
Figure 4. Observed outcomes of gastroenterologists’ patients taking probiotics (observations derived from 26% of patients on average that each gastroenterologist oversees the care of).
beneficial observations. Fortified yogurt, Culturelle, and Florastor had the lowest frequency of reported beneficial outcomes when unfamiliar probiotics were disregarded. 12 respondents skipped this question implying that gastroenterologists don’t have patients on probiotics or they observed no impact.
65.5% do not recommend probiotics for the treatment of CD or symptom complexes because there is not enough evidence to support routine use, and 48% believe treatment is inferior to/does not provide additional benefit over standard therapeutics. 3 gastroenterologists commented on question 14 that probiotics are an effective adjunctive treatment and 3 others linked AGA probiotic guidelines in the comments.
3.2. Meta-Analysis
Description of Studies
The literature search yielded 653 records and screened 255 reports. Figure 5 summarizes the study’s flow of inclusion and exclusion. The characteristics of 13 excluded studies are outlined in Table 2. 12 studies remained for analysis and were suitable for inclusion (Appendix 2: included study characteristics).
One study examined the effects of E. coli Nissle [28] . Three studies examined Lactobacillus rhamnosus strain GG (LGG) [29] [30] [31] . Two studies investigated Saccharomyces boulardii, a probiotic yeast [32] [33] . Three additional studies investigated stains of the lactobacillus genus: L. johnsonii (LA1) and L. casei [34] [35] [36] . Finally, three studies evaluated the use of probiotic cocktails containing several bacterial strains: one implements “Synbiotic 2000” (four probiotics and four prebiotics) and two observe VSL#3 (eight probiotics) [37] [38] [39] . Campieri (2000) was the only trial whose intervention group included a period of antibiotics before examining probiotic and control groups’ relapse; while
![]()
Figure 5. PRISMA study flow diagram of search results.
![]()
Table 2. Characteristics of excluded studies.
treatment remained separate, antibiotic dosage may have altered the effects of probiotics thereafter. All studies measured relapse in quiescent CD and compared probiotic and control group outcomes. The similar characteristics allowed for the pooling of studies in a single meta-analysis of the effects of probiotics as a class and methodological differences as treated as mediators to be analyzed in subgroup simulations.
Bias
Figure 6 assesses the risk of bias among included studies. Cochrane Collaboration’s risk of bias tool judged all studies as low or unclear bias. In a funnel plot larger, more precise studies with lower standard errors are expected to have risk ratios closer to the pooled estimate of the treatment effect (vertical line through the tip of the funnel), whereas the risk ratios of smaller, less precise studies with higher standard errors are expected to be more widely distributed around the pooled estimate, thus forming an inverted funnel shape [40] . The symmetrical shape of Figure 7 suggests no publication bias.
3.3. Effects of Intervention
Maintenance of Remission/Relapse
Overall, 80 (23.3%) of 344 patients assigned to probiotics experienced a relapse of disease activity, compared with 106 (29.6%) of 358 allocated to the control group. The RR of relapse in patients with quiescent CD differed in probiotics and control groups by 0.78 at a 95% CI = 0.62 - 0.98 (Figure 8), with no heterogeneity detected between studies (I2 = 0%, P = 0.65). The I2 statistic delineated that some 0% of the variance in observed effects reflects variation in true effect rather than sampling error. None of the CTR independently reported a significant effect of probiotic use on relapse; however, when a larger sample size was obtained by pooling the effects through a meta-analysis, probiotics as a class
![]()
Figure 6. Risk of bias summary: review author’s judgements concerning risk of bias criteria for included studies.
![]()
Figure 7. Funnel plot of the log risk ratios.
![]()
Figure 8. Forest plot of randomized controlled trials reporting the efficacy of probiotics versus control group in inducing in preventing relapse in quiescent CD. The results of tests for heterogeneity (Mantel Haenszel with Chi-squared statistic with representative P-value) and shown in addition to Z statistic to respective P-value to analyze the strength of the observed effect.
suggested that probiotics have significant efficacy (p = 0.04) in preventing relapse of CD compared with the control. The risk of withdrawal and serious adverse events was consistently low among probiotics and control groups; however, a more consistent approach to reporting adverse events is needed to draw firm conclusions. Sensitivity analysis performed by comparing analysis methods (fixed vs. random effects, odds ratio vs. relative risk) and study risk of bias (high vs. low) did not impact meta-analysis results. Sensitivity was also appraised by computing a “remove-one” analysis where additional meta-analyses disregarding one study could gauge the impact of each study on the combined effect. While Bourreille 2013, a large study, was identified as a potential outlier due to its significant assigned weight in the meta-analysis. The meta-analysis without Bourreille 2013 supplied similar results (Figure 9); thus, this study’s inclusion in the meta-analysis is justified, regardless of its significant weight.
Overall, 44 (16.2%) of 260 patients assigned to probiotics experienced a relapse of disease activity, compared with 64 (23.1%) of 277 allocated to the control group. The RR of relapse in patients with CD with probiotics versus control groups was 0.69 at a 95% CI = 0.49 - 0.97, with no heterogeneity detected between studies (I2 = 0%, P = 0.66). The meta-analysis identified statistical significance that probiotics are efficacious in reducing relapse in patients with quiescent CD.
3.4. Subgroup Analysis
Endoscopic Relapse versus Clinical Relapse Analysis
When 12 RCTs were categorized into types of relapse outcome measures, two groups materialized: endoscopic relapse, as defined by a Rutgeerts score of i3 or i4 (severe endoscopic recurrence indicative of relapse), and clinical relapse, as defined by a CDAI score above 150 (Figure 10). Neither subgroup was statistically significant, and no heterogeneity existed in either subgroup between studies or when comparing subgroup differences (I2 = 0%). The endoscopic relapse outcome was slightly superior in decreasing the relapse risk in the probiotic group (RR = 0.54; CI = (0.25 - 1.16)) over clinical relapse (RR = 0.81; CI = (0.64 - 1.03)); however, it is integral to note that clinical relapses had significantly more total event data.
Placebo Control versus Maintenance Treatment (Mesalazine) Analysis
12 RCTs were assembled based on the defined control group: placebo or Mesalazine, an Aminosalicylate drug prescribed to treat CD (Figure 11). Neither
![]()
Figure 9. Forest plot of randomized controlled trials reporting the efficacy of probiotics versus control group in inducing in preventing relapse in quiescent CD. Boureille 2013 was assigned 0 weight. The results of tests for heterogeneity (Mantel Haenszel with Chi-squared statistic with representative P-value) and shown in addition to Z statistic to respective P-value to analyze the strength of the observed effect.
![]()
Figure 10. Forest plot of RTCs with random effects model reporting the efficacy of probiotics versus control group for endoscopic relapse (Rutgeerts score i3 or i4) (1.1.1) and clinical relapse (CDAI) (1.1.2). For each comparison, the results of tests for heterogeneity (Mantel Haenszel with Chi-squared statistic with representative P-value) and shown in addition to Z statistic to respective P-value to analyze the strength of the observed effect.
![]()
Figure 11. Forest plot of RTCs with random effects model reporting the efficacy of probiotics versus placebo control group (1.1.1) or maintenance treatment control group (1.1.2). For each comparison, the results of tests for heterogeneity (Mantel Haenszel with Chi-squared statistic with representative P-value) and shown in addition to Z statistic to respective P-value to analyze the strength of the observed effect.
subgroup was statistically significant and detected no heterogeneity between studies in subgroups (I2 = 0%). The risk of relapse decreased more in the probiotic group as opposed to Mesalazine (RR = 0.46; CI = (0.21 - 1.02)). Relapse risk was reduced less for the probiotic group against placebo (RR = 0.82; CI = (0.64 - 1.04)); however, it is integral to note that the placebo subgroup had significantly more total event data.
Single versus Multi-Strain Probiotics
10 RCT were arranged based on the probiotic product: single species (strains belonging to lactobacillus genus and E. coli Nissle 1917) or multi-strain probiotics (VSL #3 and Bifidobacterium longum/Synergy 1) (Figure 12). Bourreille (2013) and Guslandi (2000) were not included in the subgroup analysis because trials utilized a yeast probiotic, Saccharomyces boulardii, which does not apply to either subgroup. Multi-strain probiotic intervention was statistically significant. No heterogeneity was detected between studies among each subgroup (I2 = 0%); however, heterogeneity tested between subgroups was moderate (I2 = 52.7%). The risk of relapse decreased more in the probiotic group as opposed to the control when a multi-strain product was utilized (RR = 0.57; CI = (0.33 - 0.99)). The RR value for single species intervention was close to one indicating a little-to-no difference in risk between control and placebo (RR = 0.98; CI = (0.61 - 1.58)).
![]()
Figure 12. Forest plot of RTCs with random effects model reporting the efficacy of single strand probiotic (1.1.1) and multi-strain probiotic (1.1.2). For each comparison, the results of tests for heterogeneity (Mantel Haenszel with Chi-squared statistic with representative P-value) and shown in addition to Z statistic to respective P-value to analyze the strength of the observed effect.
4. Discussion
The popularity of probiotics has increased up to 3-fold in recent years; moreover, 1 in 5 people report use for gastrointestinal and general health resources [41] . This increase in frequency fortifies the theory that a symbiotic relationship exists between the gut microbiome and the immune system, ultimately influencing human health. Gastroenterologists have access to a new therapeutic: patients can use probiotics to restore order to diseased or overly symptomatic digestive tract and maintain general health and gastrointestinal homeostasis. Previous research has shown probiotics as an effective treatment modality for common gastrointestinal disorders like C. diff and IBS, subsets of IBD including ponchis and UC, and CD in animal models where probiotics demonstrate colitis reduction properties; however, while no study has proven efficacy for probiotics in CD, the treatment has great promise.
This meta-analysis supplies an important advancement to the literature surrounding probiotic efficacy for CD. The results suggest that probiotics are efficacious in reducing relapse of CD patients in surgically or medically induced remission. The p-value of 0.04 analyzed against the significance level of 0.05 indicates sufficient evidence to claim that probiotic treatment can facilitate the maintenance of remission. This review is the first CD study to demonstrate probiotics’ efficacy fueling the need for additional large sample studies with enough power to replicate and solidify this study’s findings. One potential justification for the novel success is the extensive literature search method performed. Platforms search were not limited to well-published, reputable electronic databases; however, comprehensive hand-searches of various journals, reference lists, and “gray” literature (unpublished theses, reports, etc.) maximized the likelihood that all eligible trials to be identified. RCTs potentially missed in previous meta-analyses were included in the study pool and offered new insight into the most current review of probiotic intervention efficacy. Two more recent studies of 185 additional patients [33] [38] were not apparent in existing meta-analyses [25] [26] . This meta-analysis included 12 studies with 186 participants and demonstrated statistical significance, fortifying the conclusions made by previous meta-analyses that identified a need for larger-scale studies to determine the true effect of probiotics on CD. Additionally, RCTs included in previous reviews that examined the effects of probiotics in children were excluded from this meta-analysis in an attempt to institute a more homologous patient population. The total RR for this study was 0.78, indicating that probiotics decrease the risk of relapse by 22%. In addition, the success of this study contributes to closing the knowledge gap that the AGA identified, offers insight to establish standardized guidelines on probiotics and CD, and provides clarity for gastroenterologists on the implementation of probiotics in their practices.
The results are subject to type I error, although the chances of this are 5% due to the selected significance level. It is necessary to consider that the report’s findings are limited to the notable paucity of data on the intervention of probiotics to maintain remission in quiescent CD, putting reliability into question. A further limitation is that substantial methodological heterogeneity exists among studies. The defined control group and methods used to assess relapse, while independently validated and appropriate in their own right, were not uniform throughout the included studies; consequently, inconsistencies might have introduced biases not accounted for. Other factors that may have impacted the efficacy of probiotic treatments include whether participants had received antibiotics before the trial; the possibility that the severity of patients’ disease activity differed between the included studies; and the opportunity for variability between medically and surgically induced remission. Additional design heterogeneity resides in the probiotic product; thus, when only one or two studies are analyzed, no power exists prohibiting the assessment of the effect of individual bacterial strains on CD treatment. Finally, the quality of RCTs is inadequate, as the risk of biases in studies is unclear.
The meta-analysis only defined efficacy for maintenance treatment as measured by the risk of relapse; therefore, the results do not indicate that probiotics can treat CD. While effective in the quiescent period of CD, probiotics are defective in the active phase. 63% of gastroenterologists reinforced probiotics’ inability to treat CD; rather, 64% reported that probiotics have an adjunctive role in CD treatment. Probiotics render health benefits independent of recurrence, providing a useful adjunctive to conventional medical therapy. Numerous trials on probiotics in patients with irritable bowel syndrome (IBS) prove strains have improved patients’ quality of life [42] . Given that 46% of patients in remission with clinically quiescent CD still report IBS-type symptoms, probiotics could be a novel asset to patients in this difficult-to-treat cohort [43] . While probiotics cannot treat CD without accompanying conventional drug therapies, probiotics still yield health benefits for CD patients. If probiotics can contribute to an aspect of CD treatment, smaller doses of treatment drugs will be required to sustain remission. The reduction of drugs inevitably reduces accompanying side effects like toxicity and adverse effects benefiting patients in the long run as they attempt to treat this chronic illness. Similar conclusions derived from the meta-analysis and survey indicate a linkage between gastroenterologist behavior and clinical research; the alignment of gastroenterologists’ ideology with clinical data suggests their affinity to modify treatment regimes if new research arises.
Limitations of this survey are those inherent to any survey study; sampling bias may have affected the data if gastroenterologists with limited familiarity with probiotics failed to respond. The response rate was 37%, which, while higher than often encountered in anonymous voluntary questionnaire studies, does not eliminate the chance of bias. The survey was not distributed to gastroenterologists nationwide but rather an assessment of Wisconsin gastroenterologists; thus, one should be cognizant about generalizing the findings to the gastroenterologist population.
The meta-analysis performs three subgroup analyses to determine the effect of mediator variables. A small number of patients enrolled in subgroup analyses means these studies are at risk of lacking adequate power, preventing the possible detection of significant differences. When studies were categorized based on the relapse and control definition, no subgroup analysis illustrated a significant efficacy of a probiotic intervention in relapse reduction; therefore, mediator variables could have contributed enough heterogeneity to impact the efficacious results of the original meta-analysis. Previous meta-analyses have not conducted a subgroup analysis comparing the efficiency of multi-strain probiotic intervention against single-species products, so the results of this paper add to the literature by providing support for not only the use of probiotics but specifically those of the multi-strain variation. The multi-strain subgroup illustrated statistical significance; however, while the RR favored multi-stain over single, subgroup differences demonstrated no statistical significance. Gastroenterologists’ observations of probiotics in their practices augment the conclusion that probiotic blends have additional efficacy. Florajen and VSL #3, both probiotic blends, possessed the highest reported reduction in abdominal pain and diarrhea and the highest ability to increase general well-being for CD patients. No RCTs investigating the probiotic Florajen for the treatment of CD exist; nonetheless, gastroenterologists in the survey identified Florajen as provoking the most significant symptom resolution. This observed effect identifies a possible facet for researchers to explore and, if proven efficacious in the clinical setting, could present a safer, more affordable alternative to maintaining remission in CD patients.
This innovative research facilitates opportunities to replicate and advance probiotic findings. Next-generation probiotics are manipulated microorganisms that function as delivery vehicles facilitating treatment in situ, diagnostic tools detecting inflammation biomarkers, or biotherapeutics altering one’s microbiota. Engineered probiotics programmed to destroy harmful bacteria and replenish healthy ones could resolve CD patients’ dysbiosis: an imbalance of commensal and pathogenic bacteria. Their ability to restore a patient’s microbial homeostasis not only amplifies effectiveness in curbing common complications of current therapies but also is a promising cure. Though early in the preclinical phase, engineered probiotics have successfully suppressed intestinal inflammation, reduced fibrosis, and restored a balanced gut microbiome in mouse models of DSS-induced colitis [44] . Nevertheless, more research is needed to assess the safety and efficacy of engineered probiotics in humans. To be effective, RCTs should measure indicators of microbiome restoration: reduction in pro-inflammatory cytokine expression or increases in fecal short-chain fatty acids. Engineered probiotics could offer the same symptom and recurrence benefits as the probiotics analysis in this review but also induce remission by improving intestinal epithelium integrity.
Appendix
Appendix 1. Probiotic and Crohn’s Survey Supplement
Probiotic Usage and Recommendations for Crohn’s Disease: A Survey Study of Gastroenterologists and Practitioners Treating Crohn’s Disease
Relevant Definitions:
Probiotics: live microorganisms able to survive gastric acid and bile to reach small intestine and the colon where they potentially yield health benefits and therapeutic activities for the consumer.
● Originally derived from cultured foods, especially milk products, these protective bacteria and yeast include the lactic acid bacteria, Lactobacillus and Bifidobacterium, a nonpathogenic E. coli strain (E. coli Nissle 1917), Saccharomyces boulardii, Clostridium butyricum, and Streptococcus salivarius subspecies thermophilus
For the purposes of this survey, think about your patients and your prescribing or practice recommendations over the last one year.
1) Select the category that best defines your practice:
☐ General Gastroenterology
☐ Gastrointestinal Surgery
☐ Gastroenterology with specialty in IBD
☐ Family Practice/Internal Medicine
☐ Advanced Practice Provider
☐ Other (please specify)
________________________________________________________________
2) Describe your practice setting:
☐ Academic Medicine
☐ Private Practice
☐ Group/Hospital
☐ Other (please specify)
________________________________________________________________
3) How long have you been practicing?
☐ <5 years
☐ 5 - 10 years
☐ 10 - 20 years
☐ >20 years
4) Please select the commercially available probiotics you are aware of:
☐ Florajen Products: blend of Lactobacillus acidophilus, Lactobacillus rhamnosus, and Bifidobacterium
☐ Align: Bifidobacterium Infantis 35264
☐ VSL#3: blend of 8 probiotic bacteria
☐ Culturelle: Lactobacillus GG
☐ Mutaflor: E. coli Nissle 1917
☐ Fortified Yogurt: DanActive/Yakult/Lifeway/etc
☐ Florastor: Saccharomyces boulardii lyo
☐ Flora-Q: blend of 4 probiotic bacteria
☐ Other (please specify)
________________________________________________________________
5) How familiar are you with the current literature surrounding the efficacy of probiotic therapy to treat Crohn’s Disease and its symptoms?
☐ Extremely familiar ☐ Fairly familiar
☐ Somewhat familiar ☐ Not at all familiar
6) Do you believe probiotics are safe?
☐ Yes
☐ No
☐ I don’t know
7) Do you believe that probiotics are efficacious in treating Crohn’s Disease or its symptoms?
☐ Always ☐ Usually
☐ Sometimes ☐ Rarely
☐ Never
8) Do you believe that probiotics have a role in treating Crohn’s or alleviating certain symptoms of Crohn’s?
☐ Yes
☐ No
9) Please select the roles that you believe could be beneficial mechanics of probiotics?
☐ Lower concentration of pro-inflammatory cytokines in the intestinal mucosa
☐ Lower relapse rate
☐ Supplement conventional therapies
☐ Stabilize intestinal integrity
☐ Improvement in symptoms (diarrhea and abdominal pain)
☐ Improve malnutrition associated with Crohn’s Disease
10) What percent of your patients are taking probiotics?
11) Of your patients taking probiotics, what percent are doing so based on your recommendation?
12) Have you ever recommended probiotics for treatment of Crohn’s Disease?
☐ Yes
☐ No
13) Please select the symptoms that your patients taking probiotics for Crohn’s have seen reduction in?
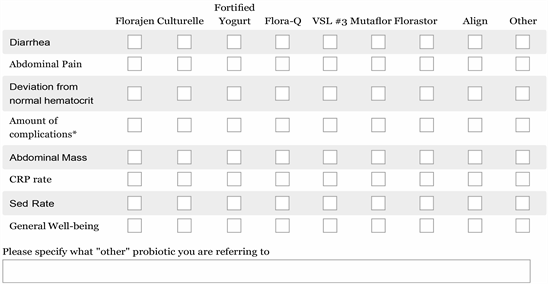
*Complications include but are not limited to Arthralgias/arthritis, Iritis/uveitis, erythema nodosum, pyoderma gangrenosum, aphthous ulcerations, anal fissure, anal fistula, or anal abscess, other fistula, fever/temperature > 100˚F/37.8˚C past week, intestinal obstruction
14) If you do NOT recommend probiotics for the treatment of Crohn’s Disease or symptom complexes please choose a reason from among the following choices:
☐ Current lack of familiarity with the literature on probiotics
☐ Feel there is not enough evidence to support their routine use in clinical practice
☐ Believe the efficacy of probiotics to treat gastrointestinal symptoms is inferior to, or does not provide additional benefit over, standard therapeutics
☐ Other (please specify)
________________________________________________________________
15) If you would like the results of the study emailed to you after responses are analyzed, please provide your email below. Thank you for taking the time to complete the survey!
________________________________________________________________
Appendix 2. Characteristics of Included Studies