Gestational TSH Levels and Their Association with Obstetric and Neonatal Outcomes in Lebanon: A National Observational Retrospective Study ()
1. Introduction
Pregnancy is a period characterized by a physiological stress on the mother and the fetus. If this stress is intensified by existing comorbidities or developed complications, then the adverse consequences can be tremendous. The last report on maternal mortality by the World Health Organization (WHO) shows that in 2017, about 295,000 women died during and following pregnancy and childbirth, and that the majority of these cases occurred in low-income countries and could have been prevented [1] . The complications that occur during pregnancy impact both maternal and fetal health and can be due to preexisting health conditions or disorders caused by hormonal or body changes during pregnancy. The most common complications include gestational diabetes, hypertension, preeclampsia, placental abruption, low or excess amniotic fluid, which might lead in severe cases to pre-term labor, miscarriage, or stillbirth. Thyroid disorders are common during pregnancy [2] , in particular hypothyroidism that remains easy to treat and should therefore be detected at early stages of the pregnancy to prevent the associated burden on the mother and fetus [3] . Thyroid hormones, triiodothyronine (T3) and thyroxine (T4) play a crucial role in ensuring normal pregnancy and fetal development [4] . Until the maturation of the fetal thyroid gland by weeks 18 - 20 of gestation, thyroid hormones are supplied to the fetus via placental transfer of maternal T4 [5] . These hormones are finely regulated by the thyroid-stimulating hormone (TSH) secreted by the pituitary gland and in turn regulated by T3 and T4 via a negative feedback loop [6] . Hypothyroidism is characterized by an elevated concentration of TSH with low or normal concentrations of free T4 [7] , whereas hyperthyroidism can be pathologic or gestational but is less common [5] . During pregnancy, demand on thyroid hormones, and consequently TSH production, increases. Therefore any alteration in this context may be as detrimental for fetal development as for delivery outcome [6] . Yet, the euthyroid definition and the determination of a normal TSH range during pregnancy are still debated [8] [9] [10] . The association between overt hypothyroidism, obstetric complications and disturbances in neuropsychological development of the offspring has been well described [4] [6] .
In this study, we aim at describing the TSH levels and measurement time-points in pregnant women in Lebanon. We also explore the effect of prior comorbidities on TSH levels and their impact on gestational complications and pregnancy outcomes.
2. Materials and Methods
2.1. Study Design and Participants
This is a national, observational, retrospective study evaluating the levels of gestational TSH in a cohort of pregnant women in Lebanon and investigating the correlation with comorbidities, pregnancy complications, and neonatal characteristics. Enrolled subjects were all pregnant women who visited the obstetrics clinic of Dr. Abi Tayeh at Hôtel-Dieu de France University Hospital, Beirut, Lebanon, from 01 September 2017 until 31 August 2018, as part of their routine follow-up and have a TSH level record. This study was approved by the Ethics Committee of the Saint Joseph University in Beirut (USJ) (CEHDF 1636). All participants signed an informed consent prior to their inclusion in the study to allow the investigator to access the data retrospectively and enter them into his database.
2.2. Data Collection
Data were extracted from participants’ clinic files, collected on a Microsoft Excel worksheet, and cleaned by an independent operator. Collected data included participants’ age, weight, TSH measurement time and value, comorbidities, pregnancy complications and outcome, as well as the neonatal characteristics of the babies. In this report, TSH levels were considered normal between 0.1 and 2.5 mUI/L in the first trimester of pregnancy, between 0.2 and 3.0 mUI/L in the second trimester, between 0.3 and 3.0 mUI/L in the third trimester, and between 0.26 and 3.0 mUI/L during the post-partum period [11] . Treatment was initiated as soon as abnormal TSH levels were detected in any participant. In line with the WHO reports, a birth weight below 2.5 Kg was considered “low”, whereas “very low” and “extremely low” birth weights were those lower than 1.5 Kg and 1.0 Kg, respectively [12] .
2.3. Statistical Considerations
Descriptive statistics were performed using SAS 9.4 (SAS Institute Inc., Cary, North Carolina, USA). Quantitative variables were summarized as follows: number of observed values, number of missing data, mean, and standard deviation. Qualitative variables were summarized using the number of observed values, the number of missing data, and percentages. Chi-square or Fisher’s Z transformation was used for the Pearson and Spearman correlation coefficient. One-way analysis of variance (ANOVA) was used for the association of categorical variables. To evaluate statistical significance, a Student t-test or a Wilcoxon/Mann-Whitney test was used depending on the normality of the data for quantitative variables, and a Chi-square or Fisher’s exact test was used depending on the expected counts for qualitative variables.
3. Results
3.1. Participants
A total of 419 women were enrolled in the study. Participants’ age ranged from 21 to 44 years with a mean of 32.8 ± 3.8 years. Their weight ranged from 42 to 109 Kg with a mean of 63.4 ± 11.8 Kg. Among all participating women, 48 (11.5%) reported at least one comorbidity prior to their pregnancy. The most occurring comorbidity was the antiphospholipid syndrome (47.9%), followed by thrombophilia (35.4%) and hypothyroidism (20.8%).
3.2. Pregnancy Outcomes
At least one complication was reported for 77 out of 419 (18.4%) of the study participants. Complications reported for more than 3% of them are shown in Figure 1.
The majority of participants for whom the data is available (353 out of 403 [87.6%]) delivered a full-term baby while only 20 (5.0%) had an abortion. On average, the duration of pregnancy for study participants was 38.0 ± 1.2 weeks.
3.3. Baby Characteristics
Over the study period, 381 out of 398 participants (95.7%) gave birth to single babies, while 4.3% had twins. The total number of babies born within this study was 415. The average weight at birth was 3.05 ± 0.45 Kg. Two babies had a very low birth weight and only one baby had an extremely low birth weight. The distribution of newborn babies across birth weight categories, their gender and breastfeeding status are shown in Figure 2.
3.4. Primary Analysis
The primary objective of this observational study was to describe TSH levels of
![]()
Figure 1. Complications and outcomes of pregnancy in study population. (a) Distribution of the 77 participants who reported at least one complication during pregnancy. (b) Percentage of a total of 403 participants having full-term babies, pre-term babies, or an abortion.
participating women along their pregnancy period. Measurements were recorded at the first, second, third trimester of pregnancy, and post-partum. Only one participant had TSH levels at all four study time points. Most of the 419 participants (243) had their TSH levels measured during the first trimester of pregnancy, followed by 183 at post-partum, 109 during the second trimester and 39 during the third trimester. The average value of TSH for all participants was within the normal range at all study time-points, and ranged from 0.0 to 25.4 mUI/L with a mean of 2.0 ± 1.9 mUI/L during the first trimester, from 1.7 to 2.1 mUI/L with a mean of 1.9 ± 1.0 mUI/L during the second trimester, from 1.6 to 2.3 mUI/L with a mean of 1.9 ± 1.1 mUI/L during the third trimester, and from 1.4 to 1.7 mUI/L with a mean of 1.6 ± 0.8 mUI/L at the post-partum period; this difference was statistically significant (P = 0.018). Study participants were then classified into categories of low, normal, and high TSH for all four time-points. The distribution of participants to the different TSH categories is shown in Figure 3. Most high TSH levels were observed during the first trimester of pregnancy.
![]()
Figure 2. Characteristics of newborns. Most babies were born with normal birth weight, and very few (1.5%) had a higher-than-average birth weight. Female and male babies were born at an almost equal rate. The large majority of babies were breastfed, either exclusively (234 [65.7%]) or together with baby formula (80 [22.5%]).
![]()
Figure 3. Distribution of participants in the different TSH categories. Throughout the pregnancy duration and in the post-partum period, the vast majority of women had normal TSH levels. Elevated TSH levels were more frequent during the first trimester, and least frequent in the post-partum period.
Further analysis showed no correlation between TSH levels at any of the considered time-points and pregnancy outcomes. There was no significant difference between women delivering pre-term or full-term babies, or those who had an abortion, with respect to their TSH levels (Table 1).
Similarly, women who had twins did not have statistically different TSH values compared to those who had single babies. However, the only significant difference was noted in the gestational term; 93.2% of women delivering single babies completed their full term, compared to 68.8% of women delivering twins (P = 0.005) (Table 2).
3.5. Secondary Analysis
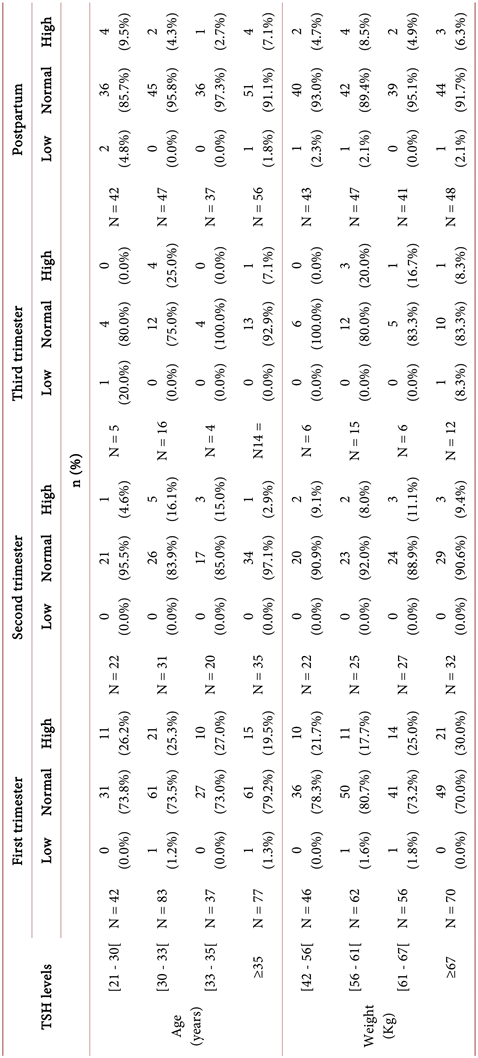
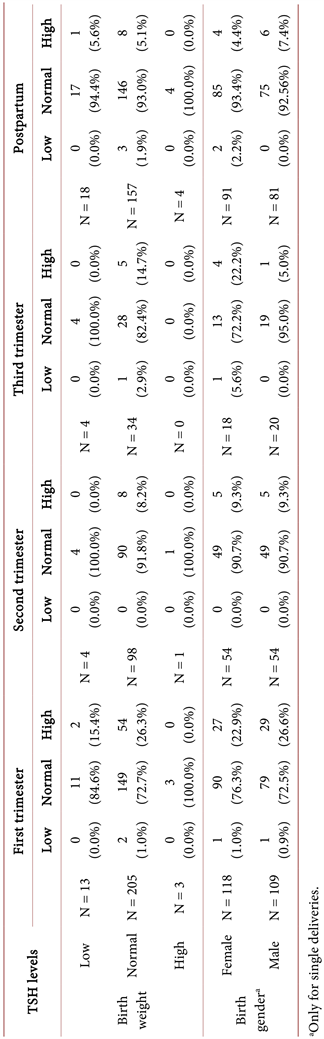
TSH levels were then analyzed in the different participant age and weight subgroups. Data showed that neither women’s age nor their weight seemed to affect TSH levels at any of the four-study time-point s (Table 3).
TSH levels were also not affected by comorbidities prior to pregnancy. Abnormal levels of TSH did not seem to be associated with complications since women having low, normal, or high TSH levels did not show a statistical difference in the occurrence of pregnancy complications, at any of the study time-points (Table 4).
We then tried to investigate the effect of gestational TSH levels on the neonatal characteristics of babies. There was no correlation between birth weights or gender and maternal TSH levels at any of the study time-points (Table 5).
![]()
Table 1. Pregnancy outcome according to TSH levels throughout the pregnancy.
![]()
Table 2. Pregnancy outcomes according to type of delivery.
Table 3. TSH levels according to women’s age and weight.
![]()
Table 4. Pregnancy complications according to TSH levels throughout pregnancy.
Similarly, TSH levels have not affected the ability of women to breastfeed and there was no significant difference in gestational or post-partum TSH levels in women who exclusively breastfed, breastfed with formula supplementation, or exclusively used formula.
4. Discussion
The present observational retrospective study investigated TSH levels during the course of pregnancy in Lebanese women. Reported comorbidities in this study were in line with their general prevalence, of around 10% for thrombophilia [13] , 12% for thyroid conditions [14] , and 0.002% for APS [15] . Moreover, a high prevalence of thrombophilia was reported in women with recurrent fetal loss [16] , highlighting the necessity to screen for this condition to allow appropriate medical control.
Table 5. Association between maternal TSH levels and birth’s weight and gender throughout pregnancy.
Although 18.4% of participants reported gestational complications, the majority delivered full-term babies and the average birth weight of newborns was within the normal range. This underscores an appropriate management of pregnant women, particularly in the presence of prior comorbidity and gestational complications.
The average value of TSH was significantly different across pregnancy trimesters and in the post-partum period, which was expected considering that the normal range for TSH is not constant in the different pregnancy periods [17] . Average TSH value for all participants was within the normal range and most participants (58%) had TSH levels reported during the first trimester of pregnancy. Although experts agree that women at high risk, such as older women or those with a family history of thyroid diseases, should be screened, there is no general consensus to screen all women particularly those who are at low risk [8] . However, the great risk of hypothyroidism in pregnancy is known, so performing a routine TSH screening for all pregnant women can be argued, especially given the relative ease of TSH measurement [8] , allowing better identification of the participants’ risk groups and consequently more appropriate care. According to the guidelines, the most advantageous time to measure TSH levels would be at the earliest, which seems to occur before pregnancy or during the first trimester, particularly in women who present other comorbidity or complications [18] . This is in agreement with results from this study, which showed that the management of thyroid dysfunction during pregnancy is aligned with the general guidelines.
Finally, there was no clear correlation between aberrant values of TSH and the presence of comorbidity, the onset of complications, pregnancy outcomes, or neonatal characteristics. This finding is in disagreement with the well-proven results in the literature showing a negative effect of hypo- and hyperthyroidism on pregnancy, leading to abortion, intrauterine fetal death, preterm delivery, preeclampsia, and other adverse outcomes [19] [20] . In this study, women who showed abnormal TSH levels were treated immediately, which prevented the presentation of symptoms related to abnormal levels of TSH. The divergence of our results from the literature with regards to the negative impact high TSH levels have on pregnancy course and outcome can also be argued by the study’s effective size. The relatively low number of participants did not allow for a numerically significant amount of complications to be able to draw statistically solid conclusions. In addition, TSH levels were not available at all time-points, rendering impossible the evaluation of TSH levels throughout pregnancy and their possible correlation with gestational complications or neonatal outcomes. A larger cohort of participants encompassing several obstetric clinics and being monitored on a more regular basis, as well as retrospective analyses of participants who developed pregnancy or neonatal complications and who were not treated for thyroid disorders, might allow us to better correlate the modulation of gestational TSH values with the course and outcomes of pregnancy and the neonatal characteristics. We would also better reflect the routine practice of obstetricians in terms of thyroid function monitoring during pregnancy in Lebanon.
5. Conclusion
This study highlights satisfactory routine practice in the management of thyroid disorders in pregnancy and underscores the need for routine TSH screening for all pregnant women.
Acknowledgements
Technical assistance was provided by the contract research organization KBP-Biomak, Lebanon, for the analysis of the data and the writing of the manuscript. This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.