Neurodevelopmental Outcomes of Extremely Premature Infants with Extremely Low and Very Low Birth Weight at Three Years of Age: A Retrospective Study ()
1. Introduction
Extremely preterm infants (EPT), less than 28 weeks’ gestation, are at high risk of morbidity and death. Despite advances in neonatal care, the rates of severe neonatal morbidity and infant mortality increase with decreasing gestational age, birth weight and structural brain changes [1] [2] [3] [4] . In a population-based study, Anderson and colleagues determined that twenty-eight percent of all extremely premature infants died within the first year of life. Among infants born at 22-, 23-, and 24-weeks gestational age, survival to one year of age was 6%, 27%, and 60%, respectively and increased significantly for each 1-week increase in gestational age, from 78% at 25 weeks to 94% at 28 weeks [1] .
In 2018, Pascal, Govaert, Oostra, Naulaers, Ortibus and Van Den Broeck reported findings of a meta-analytic review of the neurodevelopmental outcomes in very preterm (VPT) and very low birthweight (VLBW) infants born over the past decade. Very premature infants are those born from 28 to 31 weeks gestational age and very low birth weight infants are those weighing less than 1500 grams or 3.3 lbs. Pascal et al. estimated that preterm births occur in 11.1% of all worldwide deliveries. Ten percent of those deliveries are very preterm infants and 5% of those deliveries are extremely preterm infants born prior to 28 weeks gestation. Worldwide, these births represent almost 15 million infants annually [4] [5] [6] .
In the United States (U.S.), approximately 10% of all births are preterm and there is an increase in survival of the smallest and sickest infants. The incidence of major neonatal morbidities such as sepsis, periventricular leukomalacia (PVL), intraventricular hemorrhage (IVH), bronchopulmonary dysplasia (BPD) or chronic lung disease (CLD), retinopathy of prematurity (ROP), and necrotizing enterocolitis (NEC), is relatively unchanged, despite ever evolving and less invasive medical strategies [7] . Premature infants are at substantial risk for poor neurodevelopmental outcomes including cognitive delays, motor dysfunction, cerebral palsy, sensory impairments and significant lifelong disabilities [8] . Growing evidence proposes that gestational age (GA) may be conceptualized as a continuum in which births prior to 28 weeks gestation represent the severe end of a spectrum of developmental adversity and health outcomes. A systematic review and meta-analysis focusing on neurodevelopmental outcomes of infants born at 22 weeks to 25 weeks gestation demonstrated that the most observed neurodevelopmental disability is cognitive impairment followed by cerebral palsy, with vision and hearing deficits occurring less frequently [9] .
The spectrum of neurologic injury in EPT infants has shifted to include a broader range of outcomes than has been represented in the literature. The U.S. Neonatal Research Network (NRN) delineated the full spectrum of neurologic abnormalities in a large cohort (2113) of infants with a mean gestational age of 25 weeks and a mean birthweight of 760 grams. At three years of age, evaluations using the Bayley Scales of Infant and Toddler Development, 3rd Edition (Bayley III), [10] [11] indicated that neurologic exams of 1247 (59%) infants were typical. Nineteen percent (401 infants) were suspected abnormal, and 22% (465 infants) were clearly abnormal; 11% of the cohort were lost to follow-up. This study indicated a shift toward an increase in milder neurocognitive impairment among preterm survivors with a decrease in severe cerebral palsy (CP). The overall prevalence of CP in this cohort decreased from 16% to 9% during the study period, reflecting dynamic shifts in outcomes over time [12] .
In a review of neurodevelopmental outcomes in VPT and VLBW infants, the pooled prevalence of cognitive and motor delays, evaluated with developmental assessments, was estimated at 16.9% for cognitive delays and 20.6% for motor delays. A pooled prevalence of CP estimated prevalence to be 6.8% and found that decreasing gestational age (GA) and birth weight (BW) resulted in higher prevalence rates. Mild delays were more frequent than moderate to severe delays [4] .
Approximately 50% of preterm infant’s experience difficulties in executive functioning, learning, and behavior, often requiring special education services and supports [13] . Infants born with a BW less than 1500 grams, have an 11.6% increased risk of being diagnosed with intellectual disabilities, in comparison to full term infants [14] . Children born prematurely often experience difficulties in understanding language, and in reading comprehension. They experience difficulties with visual perceptual abilities, graphomotor skills, visual memory, complex language, and abstract reasoning which often results in grade retention and provision of special education services [15] . Major morbidities of prematurity have improved; however, there is now a population of individuals born prematurely who have a “hidden disability”. This population is easily misdiagnosed as functioning on the autism spectrum with higher positive screens seen in children with lower gestational ages at birth.
2. Methods
Institutional Review Board (IRB) approval (Project Number: 151017061) was secured to conduct this retrospective study evaluating the contributing factors leading to suboptimal long-term neurodevelopmental outcomes including, but not limited to, cerebral palsy, sensorineural disorders and developmental delay or disability. Relevant clinical details (BW; GA; CLD; congenital heart disease; IVH; hypoxic-ischemic encephalopathy (HIE); conditions requiring nitric oxide; intensive and lengthy medical interventions) during the initial hospital stay and through three years of age were obtained by reviewing medical, developmental, and diagnostic records of extremely preterm infants born 23 weeks to 27- and 6/7-weeks’ gestation, very preterm infants 28 weeks to 33- and 6/7-weeks’ gestation and those with hypoxic ischemic encephalopathy (HIE) born at 34 to 40 weeks gestation.
During the study period, 144 infants born in 2011 through 2015 and attending the Neonatal Developmental Follow-Up Clinic from August 2012 through December 2019, were evaluated using the Test of Infant Motor Performance (TIMP), at or prior to 4 months corrected age and the Bayley Scales of Infant Toddler development (BSID-III), at approximately 3, 6, 9, 12, 18, 24, 30 and 36 months. Twenty-two (15%) were lost to follow-up and one child passed away. This cohort included four sets of triplets and eight sets of twins. Forty-two percent were Hispanic and 58% were non-Hispanic. Seventy-three of these infants were born between 23 weeks and 27- and 6/7-weeks’ gestation. This article reports on the longitudinal data gathered on these extremely preterm infants.
2.1. Bayley-III Descriptive Classifications for Composite Scores
The Bayley Scales of Infant and Toddler Development, 3rd edition (BSID-III) is a norm referenced and standardized neurobehavioral assessment developed to help identify children with developmental delay or disabilities who may require intervention services (Bayley, 1969, 1993, 2005) [10] [11] . The BSID-III is widely used in research studies on the developmental outcomes of infants and toddlers from birth through 42 months and evaluates cognitive, language, and motor skill development. The BSID-III also includes social-emotional and adaptive behavior questionnaires; however, these were excluded from this study.
BSID-III Composite Scores are a transformation of a distribution of scores and have a given mean and standard deviation (SD). This transformation allows for a measurement in units of standard deviation of how far an individual’s score is from the mean. BSID-III composite scores are based on various sums of subtest scaled scores for Language and Motor and composite equivalents for scaled scores from the Cognitive domain.
The composite scores are scaled to a metric with a range of 40 to 160, a mean of 100, and a SD of 15. A score of 100 on any of the composites defines average performance of a given age group, and scores of 85 and 115 are 1 SD below and above the mean, respectively. Level of Performance is described as follows: 130 and Above—Very Superior; 120 - 129—Superior; 110 - 119—High Average; 90 - 109—Average; 80 - 89—Low Average; 70 - 79—Borderline; and 69 and below—Extremely Low.
2.2. Inclusion and Exclusion Criteria
Preterm and medically compromised infants born and hospitalized in the Banner Diamond Children’s University Medical Center Newborn Intensive Care Unit (NICU), formerly known as University of Arizona Medical Center and University of Arizona Health Network, from January 1, 2012 through December 30, 2015 and then followed through the Neonatal Developmental Follow-Up Clinic through three years of age were included in this retrospective study. All participants completed visits at the Follow-Up Clinic by December 31, 2019.
Infants and toddlers lost to follow-up (15%) were excluded from data analysis as were those whose BSID-III evaluations were not completed between 8 to 12 months, 15 to 18 months, or 24 to 36 months. Infants who missed one or all of these assessment time points were not included in this study. The exclusion criteria and loss to follow-up reduced the study size of infants 23 to 27- and 6/7-weeks’ gestation to 30 participants.
2.3. Data Abstraction
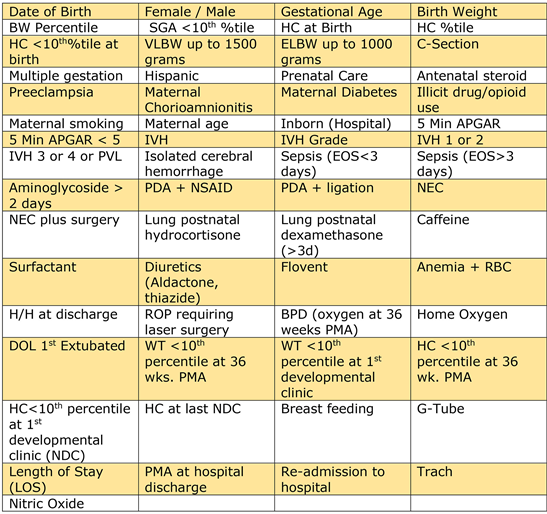
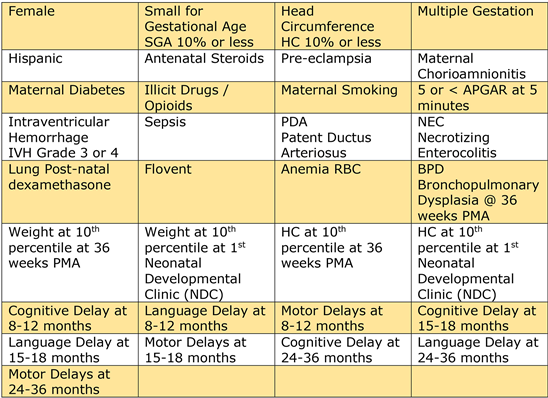
An Excel data collection sheet was developed to extract all relevant medical and diagnostic records. Sixty-one independent variables were collected along with BSID-III composite scores for Cognitive, Receptive and Expressive Language, Total Language, Fine and Gross Motor and Total Motor at 8 to 12 months, 15 to 18 months, and 24 to 36 months. Variables were marked as Yes/No for “present” or “absent” on the Excel spreadsheet after all medical data were collected. The list of study variables is included in Appendix A.
2.4. Statistical Analysis
Initially, all “Yes”/“No” variables (Appendix B) were analyzed against the 15-month to 18 month and 24-to-36-month BSID-III Scaled Scores for Cognitive Delay, Language Delay and Motor Delay with Pearson Chi-Square test. In most cases, no significant relationship was found. A more sophisticated analyses was conducted to determine any significant correlation between medical and birth variables and BSID-III scaled scores.
Following the Pearson Chi-Square analysis, predictor variables (birthweight, head circumference, chronic lung disease, antenatal steroids, multiple gestation, and length of stay) were identified for analysis with outcome variables (cognition, total language, total motor) using a MANOVA. Marginal effects on several predictor variables were found with several outcome variables. To analyze the effect of several continuous covariates Multiple Regression Analysis was used to analyze the data. Following the Multiple Regression Analysis, a Stepwise Multiple Regression was conducted to determine the model of best fit. All statistical analyses were carried out with SPSS 28, commonly used statistical analytic software.
3. Results
The Pearson Chi-Square test did not find a statistically significant relationship between any of the 60 independent variables and a diagnosis of Delay in Cognitive, Total Language or Total Motor Skill development. The Pearson Chi-Square test did reveal that 50% (15 of 30 toddlers) of the ELBW infants had no developmental delay and 50% had language delay with 43% having a mild delay and <1% having moderate delay. Analysis of the VLBW group of 18 infants and toddlers, found that 7 had no language delay while 11 had language delay with 6 having mild delay and one with moderate delay. No significant correlations were found between birth weight, gestational age, head circumference, or intraventricular hemorrhage and risk of language delay [9] .
3.1. Manova
Multivariate (repeated) measures were conducted to analyze change across time within subjects. These complex analyses were conducted to check consistency with replication of the data. Analysis of the results of the Bayley III were conducted at three different time period (8 - 12 months, 15 - 18 months, 24 - 36 months) to look at change over time. Developmental domains evaluated using the Bayley-III include Cognitive, Total Language and Total Motor. To determine the effect of change over time within subjects, a statistically significant among centroids was observed (Wilk’s Lambda = 0.660, F (6, 108) = 4.149, p = 0.001). The fairly robust results gleaned from the t-test and ANOVA showed homogeneity of covariance.
Sphericity was assumed for the univariate tests since those tests were not significant (all probabilities were greater than 0.2); Neither Cognitive nor Total Motor measures were significant, however, Total Language was highly significant in change over time, F (2, 56) = 8.786, p < 0.001. Data were analyzed, using a Post Hoc test (Pairwise Comparison) for Total Language. Total Language showed significant changes between the first evaluation and the second. Results were consistent between the second and third evaluations. See Figure 1.
![]()
Figure 1. Mean scores over time for cognitive, language, motor.
Correlations were found at the p < 0.05 significance between GA and Total Language; BW and Cognition; and LOS and poorer motor development. Gestational age and Birth Weight correlated highly with Length of Stay at the p < 0.01 significance. Variables were considered statistically significant at a p-value < 0.05.
3.2. Multiple Regression Analysis
Initially, regressions were completed to see how well variables would correlate. For each of the outcome variables, all 61 predictor variables were added. Many variables were not significant, possibly due to multicollinearity. Following this analysis, the continuous covariates to be considered in a multiple regression analysis were filtered to select the variables with the strongest relationships. All variables whose simple correlation with the outcome variables were significant at the 0.05 level were considered as covariates in the multiple regression analysis. The filtered predictor variables included GA, BW, LOS, BPD and HC at the 10th percentile at the first clinical visit. The outcome variables included Scaled Scores from the BSID-III for Cognition, Total Language and Total Motor.
A second set of regressions used a Stepwise approach in which only one variable in each regression passed the criterion for entering the equation. In this analysis, BW correlates the most with low cognitive scores. We also found that LOS, or the longer an infant remained in the NICU, the poorer the Total Language Scaled Scores at 8 to 12 months, 15 to 18 months, and 24 to 36 months. Results indicate that increased BW results in improved Total Language regardless of LOS. Birth weight is the greatest predictor of poor motor scores and is significant at the 0.07 level (Table 1, Table 2).
While our statistical analysis did not reveal significant p-values, it did demonstrate that some predictor variables impact neurodevelopmental outcomes in cognitive, language and motor skill development.
![]()
Table 1. F-Statistics for cognitive, total language, total motor ANOVAa.
a. Dependent Variable: Cognitive; b. Predictors: (Constant) Birth Weight.
a. Dependent Variable: Total Language; b. Predictors: (Constant) Length of Stay.
a. Dependent Variable: Total Motor; b. Predictors: (Constant) Birth Weight.
![]()
Table 2. t-Statistics for cognitive, total language, total motor.
a. Dependent Variable: Cognitive; b. Predictors in the Model (Constant) Birth Weight.
a. Dependent Variable: Total Language; b. Predictors in the Model (Constant) Length of Stay.
a. Dependent Variable: Total Motor; b. Predictors in the Model (Constant) Birth Weight.
4. Discussion
The preterm infant is a challenging population to study and generalize outcomes due to the complexity and diversity of the population as well as treatment and interventions that vary across the lifetime of the individual. It is known that premature birth can impact neurodevelopmental outcomes adversely and can lead to difficulties throughout life and in social, employment, and health realms once these individuals reach adulthood. Premature infants are more likely to repeat one or more grades, more likely to require special education services, and more likely to leave school early. Seventy-four to eight-two percent graduate from high school and only 30% to 32% matriculate to college. As adolescents and adults, premature individuals do not perceive themselves as different from their peers behaviorally or emotionally; yet they rate themselves lower in scholastic, athletic, romantic and job competency measures [16] .
Major morbidities of prematurity have improved over time with less severity of disability; however, there is now a population of individuals born prematurely who have a “hidden disability”. This population is easily misdiagnosed as functioning on the autism spectrum with higher positive screens seen in children with lower gestational ages at birth. Several studies have reported reduced social interactions and risk-taking behaviors in VPT and VLBW adolescents and higher introversion, autistic features and neuroticism that may reinforce some of the social difficulties in this population [15] .
Neonatal intensive care has improved over the last few decades with improvements in integrative care and the adoption of neuroprotective developmental care in NICUs around the globe. Altimier and Phillips have identified seven core neuroprotective components that should be incorporated into NICU care [17] . These components include a healing environment, partnering with parents/caregivers, positioning, and handling, safeguarding sleep, reducing pain and stress, protecting skin, and optimizing nutrition. These measures, along with newer researched based interventions, can improve neurodevelopmental outcomes in extremely preterm, very preterm, and late preterm infants receiving care in the NICU. The NICU at Banner Diamond Children’s University Medical Center has integrated these concepts into the treatment and care of the most fragile of infants. All nurses are educated on developmental care and interventions, there is a core Developmental Team with Newborn Individualized Developmental Care Assessment and Plan (NIDCAP) certified individuals to carry out interventions; and there is a robust multidisciplinary team of subspecialized Physical Therapists, Occupational Therapists, and Respiratory Therapists to support the plans for each infant.
Moreover, The National Institute of Child Health and Human Development recommends developmental follow-up, including ongoing developmental assessment and intervention, for all infants with a birth weight of 1000 grams or less with assessment of their socioeconomic status, family resources, growth, neurologic status, behavior, and language [12] . Newborn developmental follow-up clinics provide an important resource for optimizing care of these specialized and often complicated children by identification of neurodevelopmental status, deviations of growth and behavior and referring these high-risk children to appropriate resources in their community. This NICU also has a long standing developmental follow up clinic that assesses up to twenty NICU graduates per week.
This retrospective study was performed to discern potential associations between gestational ages (GA), birthweight (BW), neurologic sequelae, maternal age, and other risk factors on cognitive, language and motor delays when evaluated at 8 to12 months, 15 to 18 months, and 24 to 36 months. Data were obtained by reviewing medical, developmental, and diagnostic records of extremely preterm infants born 23 weeks to 27- and 6/7-weeks’ gestation. The same medical and developmental records were reviewed for preterm infants 28 weeks to 33- and 6/7-weeks’ gestation and those with HIE born at 34 to 40 weeks gestation. This article only reports on the extremely preterm infants born 23 weeks to 27- and 6/7-weeks’ gestation.
In addition to the emphasis on specific gestational ages, this retrospective study focused on infants and toddlers who spent time in a NICU and participated for three years in neonatal developmental follow-up clinic prior to the SARS-CoV-2 pandemic. Each infant and toddler attending the neonatal developmental follow-up clinic was evaluated every six months, initially using the Test of Infant Motor Performance (TIMP) prior to 4 months adjusted age and the Bayley -III up to three years of age. Clinicians discussed the results of the evaluation with parents and caregivers, provided parent support and education on developmental activities to enhance skill development, shared resources, and initiated referrals for early intervention and other services and supports when indicated.
The meta-analytic review conducted by Pascal et al. found that one out of six VPT infants and one out of five VLBW infants, had a cognitive or motor delay as assessed with the Bayley or other developmental scales at two years corrected age. Pascal et al reported that decreasing birthweight and gestational age led to a higher prevalence of cognitive and motor delays and cerebral palsy [4] .
Findings from this retrospective study found significance between birth weight and low cognitive scores. Additionally, the longer an infant remained in the NICU, the poorer the Total Language Scaled Scores at 8 to 12 months, 15 to 18 months, and 24 to 36 months were based on results of the BSID-III. Correlations were also found between GA and Total Language. Birth weight was the greatest predictor of poor motor scores.
Language delay was most prevalent among the ELBW group with 50% of children having some type of delay, though most had mild delay (43%) and no children had severe delay. No significant associations between previously reported risk factors for language delay and outcomes were noted in this population. Overall, these findings suggest that intensive multidisciplinary therapy following NICU discharge may ameliorate some of the neurologic injury sustained in ELBW and VLBW infants.
Concerns have been raised about assessing cognitive and language development with the BSID-III [18] [19] [20] [21] . Reports highlight the potential underestimation of developmental delays by the Bayley III Scales of Infant and Toddler Development. However, it has not yet been determined whether the Bayley III underestimates developmental delay or whether the earlier version, the Bayley II, overestimated it.
Abnormalities or deviations cannot be explained by any single protective or risk factor; however, the quality of the intensive care, home environment and participation in a developmental follow-up clinic every six months for three years may have played a critical role in the trajectory or recovery, growth, and development of these extremely and very preterm infants. There is room for further analysis of other cohorts of infants from this NICU population that may help establish outcome patterns that were not yet found in this single population analysis. The same data for infants born between 28 - 38 weeks’ gestation as well as infants with HIE has yet to be analyzed. Analysis of the data from these individual groups will further elucidate any consistent patterns in outcomes that can be tied back to protective or risk factors that may be specific to this NICU environment and developmental follow up clinic.
Acknowledgements
Neonatologists and Pediatricians who cared for these infants in the NICU and evaluated them in the Neonatal Developmental Follow-Up Clinic from 2011 through 2019 include: Drs. Alan Bedrick, Mohammed Bader, Ranjit Kylathu, Joseph Livingston, Karen Davenport, and Graciela Wilcox. NNP, Cynthia Garcia and Neonatal Physical Therapists Nichole Lensing and Mary Beth Hoffmeyer along with Authors Jacob and McGrath conducted diagnostic evaluations, provided parent education, referral, and support services.
Appendix A. Medical and Demographic Data Collected
Appendix B. “YES”_“NO” Variables
Abbreviations
ADHD—Attention Deficit Hyperactivity Disorder
BPD—Bronchopulmonary Dysphagia
BSID-III—Bayley Scales of Infant and Toddler Development (3rd Edition)
BW—Birth Weight
CHD—Congenital Heart Defect
CLD—Chronic Lung Disease
CP—Cerebral Palsy
ELBW—Extremely Low Birth Weight
EPT—Extremely Preterm
GA—Gestational Age
HC—Head Circumference
HIE—Hypoxic Ischemic Encephalopathy
IVH—Intraventricular Hemorrhage
LOS—Length of Stay
NEC—Necrotizing Enterocolitis
NICU—Neonatal Intensive Care Unit
PVL—Periventricular Leukomalacia
ROP—Retinopathy of Prematurity
SD—Standard Deviation
TIMP—Test of Infant Motor Performance
VLBW—Very Low Birth Weight
VPT—Very Preterm