Are They Watching: Pedagogical Influence of Role Modeling on Student Competence, Confidence, and Clinical Reasoning ()
1. Introduction
The current pandemic has provoked a remapping of nursing curricula to ensure competent and safe practice in a timely manner. Globally, healthcare delivery services were already under pressure with an aging population worldwide [1]. The pandemic has increased the needs exponentially. Meeting such needs in a sustainable manner requires the capability to provide trained professionals who are work-ready without posing a risk to patients. Undergraduate nursing programs recognize the importance of competence in psychomotor skills but do report a lack of opportunity to practice during clinical training [2].
Immersive classrooms integrating simulation with expert role modeling have emerged over the past 20 years to prepare students to meet the challenges of increasingly complex clinical environments [3]. Simulation is an interactive teaching strategy which replicates essential aspects of reality so that reality can be better understood by students to encourage critical thinking [3]. Our team identified a gap in simulation educator development and discovered an educational scaffold which students embraced to improve their critical thinking and clinical judgment [4] [5]. We did not think they were really watching. However, students reported that they changed their practice based on what they observed as we role modeled caring for a deteriorating patient [6].
2. Background
Currently New Zealand requires 1100 - 1500 hours of clinical placement time for students to graduate from a three-year under-graduate nursing degree [7]. No simulation can be substituted for clinical hours at this time. One of the challenges with this requirement is that students are often sent to clinical sites where they observe practice that may not be up to required standards. Students may experience a sort of cognitive disequilibrium as they experience a difference in management of care in clinical settings verses what they are taught in the classroom. They can wonder, “Which way is the correct way?”.
There are certain aspects of undergraduate professional education which are caught rather than taught (e.g., end-of-life care, professionalism, communication styles). These aspects form part of what has been called the hidden curriculum [8]. This hidden curriculum is often delivered by implicit rather than explicit means. This implicit curriculum is as important as the explicit curriculum but may not be as visible [9]. Observational learning through role modeling is one part of implicit curriculum which has been proven effective with undergraduate nursing students [8]. Role modeling as an educational scaffold can help move students forward in their understanding, critical thinking, and behaviour when dealing with patients [10].
2.1. Constructivism
Constructivism is a learning theory espousing that people construct knowledge and meaning from their experiences [4]. Through constructivism the student creates meaning in a team-based collaborative learning environment. In this context the role of the educator changes from content expert to facilitator assisting students to construct their own learning [2] [11]. There is a direct link between constructivism and role-modeling in that through role-modeling students observe another performing a skill/behaviour and subsequently alter their own performance. The student moves from a passive stance as receiver of content knowledge, to an active participant in the learning process. Constructivist learning supports creative problem solving as the student assimilates new information/concepts. This research involves an immersive constructivist environment (a simulation) employing role-modeling by experienced nurses. Role modeling by experienced nurses, including nurse academics, is a key factor in the process of preparing undergraduate nursing students for practice, and may contribute to longevity in the workforce [12].
2.2. Simulation as a Teaching/Learning Platform
Simulation is an activity that represents real or potentially real-world activities, including hypothetical situations such as major disasters [13]. It is a learning platform which allows construction of new knowledge and subsequent integration into current knowledge [4]. As a means of developing professional competence, it stretches back over many centuries and emerges in many industries such as the military and aviation. Within nursing education, simulation may include a manikin that mimics the human body (e.g., respiration, heart rate) as it responds to student interventions. Simulation was used as a teaching/learning platform in this research with expert nurses’ role-modeling effective and professional behaviour in a deteriorating patient situation.
Simulation has been used as a teaching strategy in nursing education for decades [6] [14] [15]. Combining role modeling with simulation presents a unique opportunity to develop student knowledge, skills, and attitudes [16]. Role modeling is a form of observational learning which is a component of Bandura’s social learning theory [12] [17]. Bandura [17] theorized that individuals could learn by observing the behaviors of others and the reactions that these behaviors elicit. The combined strategies of role modeling, reflection, and debriefing can have a powerful influence on critical thinking and clinical judgment [3] [16].
2.3. Role Modeling as a Scaffold
Role modeling occurs when a behavior or skill is demonstrated and then duplicated by an observer [16]. It can act as an educational scaffold to move students progressively toward deeper understanding and greater independence in the learning process [6]. John Dewey, one of the earliest thinkers informing constructivism, explains that genuine education comes through experience, but that not all experiences are educative [18]. Dewey clarifies that observation is pivotal in habit alteration and modeling the expected performance to the students provides a pivot upon which to build a revised performance of their own. It is therefore important that all role-modeling used in educational platforms be not only correct in content but delivered in a manner which inspires students to improve their own performance. Role modeling must be educative.
Dewey [19] spoke of interacting with a ‘matured social medium,’ which in this research is the simulation facilitator, but could also be other students within the simulation setting (p. 90). It is through the role-modeling of the simulation facilitator that this scaffold is delivered. Student learning is constructed after observing the simulation facilitator role-model expected performance. This process involves new habit formation which Dewey deemed the heart of constructivist thought [19].
Through role modeling students are presented with a behavior or skill which is demonstrated and then duplicated by the student [20]. The student observes the modeling, attempts the behavior, and reflects. This process allows new knowledge to combine with current understandings. This weaving of new knowledge with current understandings brings a deeper level of thinking to students. This research aims to explore the effect of modeling within simulation to enhance problem solving and critical thinking with undergraduate nursing students.
3. Research Design
3.1. Action Research
This project employed action research which involves improving personal and social situations while explaining why these situations are beneficial [21]. This methodology involves a cycle of inquiry (observe, reflect, act, evaluate, modify next cycle) which assists undergraduate nursing students to consider a problem with subsequent critical evaluation of best solutions [3]. There were three action cycles—the first two were qualitative and descriptive in design with the third employing mixed methods. This form of practitioner research allows concurrent evaluation and resolution of issues as cycles unfold.
3.2. Research Aim
In one university in New Zealand, it was noted that some students were avoiding simulation sessions. When questioned they often reported that they did not like being asked to perform in settings where they were not guaranteed success. This study emerged as an investigation in how to improve the pedagogies ‘wrapped around’ simulation to improve critical thinking and problem-solving while also being inviting to students.
The research question for this project was, “How can pedagogical practices be improved when working with undergraduate students in simulation environments?” One practice employed was role modeling by expert nurses. The research aim was to determine the effect of role modeling embedded within simulation to influence critical thinking and judgment in undergraduate nursing students.
Approval for the study was gained from the University Human Ethics Committee and participants were recruited from all three years of a university undergraduate nursing degree. Inclusion criteria required participants be enrolled in the undergraduate nursing program at the time of data collection.
3.3. Data Collection
Data collection occurred over a 24-month period. Participants included 161 students, 35 clinical educators and two technicians. Multiple methods were employed including questionnaires, focus groups (Appendix A.1), technician interviews, pre- and post-simulation quizzes (Appendix A.2), and evaluation of student performance using the Lasater Clinical Judgment Rubric (LCJR) [22] [23]. Multiple methods yielded a broad range of evidence as to the effectiveness of simulation on clinical reasoning, content knowledge, satisfaction, and overall professional confidence [3] [4].
Focus groups, interviews, and questionnaires all facilitated discussion around current barriers and enablers influencing student learning in simulation. These groups met on the day following the simulated learning experience. The students were asked questions to gain clarification around role performance and most and least valuable aspects of the simulation such as, “Which role do you think was the most difficult and why?” Audio recordings were made of each focus group. Responses were transcribed verbatim and subsequently uploaded into NVivoTM where they were thematically coded with the research question in mind. The qualitative responses to the post-test questionnaire were transcribed, uploaded into NVivoTM and coded for themes. New ideas around simulation design emerged as student feedback continued to illuminate current practice.
3.4. Data Analysis
Cycle two of a three-cycle action research study included a questionnaire which was answered by 125 participants involved in a simulation. The comments were transcribed and thematically analyzed with the research question as a guiding inspiration. The themes captured aspects about the data in relation to the research question and represented some level of patterned response or meaning within the data set [24].
4. Results
4.1. Role-Modeling: Show Us How to Do It First
This research involved three action cycles, each informing the next in an action research methodology. Participants in the first cycle reported significant anxiety when attending simulation. The questionnaire within cycle two was answered by 125 participants who were asked what they most valued in the revised simulation which had been embedded with changes from the first action cycle. Students wanted to observe first and then make their own attempt. Research [19] has shown that observation is pivotal to learning new skills. Modeling the expected performance provides a pivot upon which students can build a revised performance of their own [16].
The highest valued intervention in this research (33% of coding for this question) was having the facilitator model (act out) the simulation showing how to perform each of the four roles. The students found this “picture” of the goal before them both informative and inspiring [3] [4]. Expert role modeling in simulation is a constructivist strategy which assists students in building a safe and relevant response to a deteriorating patient situation [2].
4.2. Let Us Learn One Role at a Time
Students in cycle one reported being overwhelmed and not knowing what they were supposed to be doing. They were confused as to what skills/thinking they need to be accessing. One option for reducing this feeling of being overwhelmed was to divide the students into roles. Each role is given boundaries and expectations, and the students are only required to perform one role. This strategy employed in the second action cycle proved effective in reducing student overload and panic, increasing student confidence, and managing the load on working memory. The data showed that students preferred working in roles as evidenced in the debriefing for group two:
You could just focus on one thing and not think of everything else. You do it well because you think, “this is what I need to do, and I know how to do it.” You feel more confident in your team as well—you’re not just standing there.
(Debriefing cycle two)
Feedback from cycle two students around the value of modeling is below:
The role play that the educator did in the middle was helpful to show us all the roles needed and assessments that needed to be done. Understanding what it was that I was supposed to do—having a demonstration of exactly what was expected was very helpful.
What I value from today’s simulation is how the educator demonstrated it to us before the simulation started. That helps with our self-confidence. Also, giving us feedback afterwards was helpful as she told us to believe in ourselves.
[The educator] gave us a role play and how to react appropriately. If I did not have a chance to watch the role play by [the educator], I think I would still be confused.
(Questionnaire responses, Cycle 2)
4.3. Gently Show Us What We Do Not Know And How to Apply That Information
Cycle three of this project involved with 21 students progressing through three scenarios in a repeated measures design. Students began with a pre-briefing clip which involved role-modeling by simulation facilitators. They were also given a pre- and post-simulation quiz followed by a focus group to debrief and gain an understanding around what aspects of the simulation were most valuable to their learning. Cycle three comments included:
We really thought the clips were great! I thought, “She can do it, so can I.” In some ways we were competing with you. We saw you and I thought, “I want to do better than them.”
I watched you acting it out and I thought, “Yeah, I haven’t done that, and I should have done that.” You doing it was setting a standard, a role model.
With the paediatric simulation I noticed when [my partner] and I did it the first time we went for the IM injection first. When we watched the model clip, we noticed you did the nebuliser first. That made sense as it [the adrenaline nebuliser] acts faster in the lungs than the IM injection. So, we changed that order of medications in our repeat performance because that made sense.
(Focus group cycle three)
The student making the final comment had learned by watching a model clip that the order of medication administration mattered in the croup scenario. The student had developed a sense of salience for clinical situations involving respiratory compromise. Teaching for a sense of salience requires that the educator present experiential learning opportunities using a strategy called situated teaching [25] [26]. This teaching involves coaching the student through what is salient (most notable and significant) about a specific clinical situation. The facilitator must guide students to apply their knowledge to refine their actions. Ultimately, if this process is occurring regularly and in a safe environment, students will begin to develop clinical imagination and the skills of clinical reasoning [27] [28].
5. Discussion
As shown in Figure 1, this study identified three key contributors to student learning gained from role modeling: 1) improvement in professional competence (e.g., management of situation as well as emotional responses); 2) improvement in clinical reasoning and judgment regarding patient situations; and 3) improvement in professional confidence to manage clinical situations.
![]()
Figure 1. Effects of role modeling on student learning.
5.1. Role Modeling Professional Competence
Professional competence involves students’ ability to transfer and apply knowledge to relevant situations in a safe manner [29]. It includes various aspects like skill performance (e.g., intravenous lines, vital signs, assessment skills, CPR, etc.) effective communication, and working within a team. Role modeling of these various professional competencies allows students to view a clinical expert performing in the role. This performance provides a kind of snapshot of what is expected which can be both inspirational and educational.
Cycle two of this research involved the facilitator role modeling all four nursing roles within the simulation (i.e., assessment of patient, vital signs, communicating via ISBAR, medication administration). This was done as an educational scaffold to move students more gently into a deteriorating patient scenario. It is common for new or less experienced nurses to “freeze” and not know what is required in a clinically deteriorating situation. Students may appear light a “rabbit in headlights” in these unfamiliar simulations. This commonality is not only unsafe for the patient but can prove devastating for the nurse involved [20].
This research used a role modeling video in the pre-briefing of the simulation which had a positive impact on the development of a variety of nursing skills and competencies [3]. Use of an expert role modeling video has been shown to improve student professional competence thus improving patient safety [2]. The benefit of using a video is that it can be viewed multiple times. This maximizes facilitator time and becomes a reliable and trustworthy educational scaffold.
Students in this research reported that being able to maintain one role within a team was more manageable than trying to cope with the entire situation [3] [4]. Furthermore, designing roles within the simulation allowed students to gain competence in managing one small piece of the overall situation.
Working memory allows the processing of about seven single elements or pieces of information that need to be stored, manipulated, or learned at one time [30]. Limiting the student to one role makes their management of the situation more likely. This design enables students to practice their skills and begin to learn how it feels to be a nurse—a part of professional identity [31].
5.2. Role Modeling Clinical Reasoning and Judgment
The literature shows that verbalisation of thinking by expert nurses is an important part of student learning [25]. In actual clinical situations, expert nurses may simply act out of trained expertise, and not express the thoughts behind their actions. In such situations, observing students are unable to grasp the clinical judgment and critical thinking of the expert clinician [32].
It has been noted [30] that during complex learning situations, the amount of information required to be processed simultaneously can either underload or overload the amount of working memory one holds. Role modeling of expected behaviours allows students to view the required performance, observe the clinical reasoning unfolding, and ultimately view the nurse expert making the appropriate clinical judgment [2]. New understandings are then woven into long-term memory [33].
5.3. Role Modeling Professional Confidence
Professional confidence involves the nurse accepting responsibility for their actions while potentially, through reflection and debriefing, understanding more about themselves [34] [35]. Students are more likely to challenge themselves and develop critical thinking as they have more confidence in their abilities [29]. Student confidence leads to a deeper understanding of information and a higher level of thinking [9].
Professional confidence was role modeled in this research as each position (role) was acted out for the students. Facilitators acted confidently, demonstrated skills competently, and communicated a handover using the ISBAR communication tool. Students felt this modeling set a standard which they were at times compelled to compete with. Role modeling when used as an educational scaffold can promote student engagement [16].
6. Limitations
Due to time constraints only three role modeling videos were produced. There are many other deteriorating patient scenarios which could be explored. Further research is needed to understand which types of deteriorating patient scenarios are most difficult for students to manage. Additionally, further research into which aspects of the modeling videos were most educative to students would be helpful to embed these into future videos.
7. Conclusion
In this study, the use of an expert role modeling video as a prebriefing educational scaffold strengthened undergraduate nursing student professional competence, clinical reasoning and judgment, and professional confidence. These abilities are essential to provide safe and competent care, and to encourage professional identity/development in undergraduate nurses. Future research may include exploring the effect of multiple viewings of the expert role modeling videos before students come to simulation experiences to gain an understanding on the influence of this scaffold on automation and long-term memory. Additional research is warranted in the area how to provide students with role modeling in many different deteriorating patient situations to ensure patients are receiving competent care in all settings.
Appendices
A.1. Student Evaluation of Simulation Experience (Cycle 2)
1) How did you feel about coming to this simulation event today?
Please rank your simulation experience PRIOR to today’s simulation on the
scale below:
(Negative feelings) 1………2………3………4………5 (Positive feelings)
Words that describe your feelings about previous simulation experiences:
2) What did you value most in today’s simulation experience?
3) What could educators/clinical educators do better?
4) What hindered your learning today?
5) If the world was perfect, what would you design into a simulation
experience?
6) How do you feel about today’s learning experience?
(Negative feelings) 1………2………3………4………5 (Positive feelings)
Words that describe your feelings:
7) Is there anything else you want to add to this discussion that has not
already been asked/commented on?
A.2. Pre- and Post-Test—Hypovolaemic Shock Scenario (Cycle Three)
1) What is the cause of hypovolaemic shock?
a) A lack of adrenaline in the body
b) The body experiences a stressing event
c) A loss of extracellular fluid volume which exceeds fluid intake
d) A loss of intracellular fluid volume which causes cellular dehydration
2) Which one of the following signs might NOT indicate hypovolemic shock?
a) A decreased appetite
b) Weak, rapid pulse and hypotension
c) Cool, clammy skin
d) Tachypnoea
e) Reduced urine output
3) Which interventions would NOT BE APPROPRIATE in managing
hypovolaemic shock in a client who has undergone spinal anaesthesia?
a) Elevate the legs
b) Notify the registered nurse and/or physician immediately
c) Establish IV access
d) Check vital signs frequently
4) What kind of position does reverse Trendelenburg indicate?
a) Sitting upright at a 90-degree angle
b) Lying flat in bed with knees elevated
c) Lying in a supine position
d) Lying with lower extremities lower than the head and neck
5) Which of the following lab values is NOT relevant for a client experiencing
hypovolaemic shock?
a) Serum urea and creatinine
b) Serum CO2 levels
c) Haematocrit
d) K+ and Na+ levels
6) Which of the following would NOT be appropriate in the management of a
client with hypovolaemic shock?
a) Elevate the head of the bed to ensure proper respiratory pattern
b) Maximise oxygen delivery
c) Control further fluid loss
d) Implement fluid resuscitation procedures
7) What aspects of the abdominal assessment would be abnormal in the case
of a bowel obstruction?
a) Palpation—the abdomen will not be soft to palpation
b) Percussion—the percussion note would not be tympanic
c) Inspection—there would be visual changes
d) Auscultation—there would not be normal bowel sounds
e) All the above would be abnormal
8) Which of the following conditions would NOT cause hypovolaemic shock?
a) Burns
b) Diarrhoea
c) Excessive perspiration
d) Seizures
e) Vomiting
9) When communicating using the ISBAR format, what does the “S” stand
for?
a) S stands for “substance”—which substance is present in their blood?
b) S stands for “situation”—what is the situation of your patient?
c) S stands for “standard”—which standard nursing diagnosis are you
concerned about?
d) S stands for “serum concentration”—what is the serum concentration of
CO2 in their blood?
10) What of the following is a true statement?
a) Cardiogenic shock involves neurotransmitters
b) Hypovolaemic shock is about fluid volume in the body
c) Septic shock involves a kind of electrolyte shift in the body
d) Cardiogenic shock is always fatal
In addition to the above 10 post-test questions, please take five minutes to
answer the following reflective questions:
1) How satisfied were you with this simulated suite?
Not very helpful 1-------- 2-------- 3 -------- 4 -------- 5 Very helpful
How did the suite of scenarios affect your knowledge base in dealing with
deteriorating situations?
Not very helpful 1 -------- 2-------- 3 -------- 4 -------- 5 Very helpful
How did participating in this suite of scenarios affect your confidence in
dealing with deteriorating client situations?
Not very helpful 1 -------- 2 -------- 3 -------- 4 -------- 5 Very helpful
How did participating in this suite of scenarios affect your ability to work in a
team?
Not very helpful 1 -------- 2 -------- 3 -------- 4 -------- 5 Very helpful
2) Which role did you play in this scenario, and was it harder or easier than
the other roles? Please tell why below.
a) Recorder of data and calling ISBAR report
b) Assessment of relevant system and medications
c) Vital signs repeatedly and securing airway and oxygen devices
3) Which role do you think is hardest to master and why?
4) What was the least valuable aspect of your learning today? What changes
would you make?
5) If the world were perfect and you could have whatever you desired, how
would you alter what happened today to maximise your learning in
simulation?
A.3. Pre- and Post-Test: Acute Coronary Syndrome
1) What is the purpose of aspirin given early on in an acute coronary event?
a) To decrease the chest pain
b) To protect the lining of the stomach
c) To help with headaches
d) To decrease platelet aggregation
2) What does the ventricular tachycardia protocol require as a first action?
a) Check for pulse
b) Check for responsiveness
c) Deliver shock
d) Place IV
3) What tests can be diagnostic of ischemia in the cardiac wall?
a) CT scan
b) ECG
c) Troponin-T
d) MRI
4) The two main factors influencing blood pressure are:
a) CO & SVR
b) Heart rate and SVR
c) Kidney function & heart rate
d) SVR and kidney function
5) What is the formula for calculating mean arterial pressure (MAP)?
a) Systolic + Diastolic/2
b) Diastolic + heart rate/3
c) Heart rate/Diastolic
d) Systolic + 2(Diastolic)/3
6) What is the minimum MAP required to perfuse vital organs?
a) 10 mm Hg
b) 50 mm Hg
c) 120 mm Hg
d) 70 mm Hg
7) What is the medication used specifically to dilate coronary arteries in angina?
a) Labetalol
b) Cardizem
c) Nitroglycerin
d) Aspirin
8) When a person is experiencing angina chest pain, what is happening on a
cellular level?
a) There is excess acid in their stomach causing irritation
b) The cardiac muscle is becoming ischaemic and dying
c) Their airways are becoming constricted decreasing oxygen availability
d) Plaques are forming in their coronary arteries
9) What is the rhythm below?
a) Sinus Rhythm
b) First degree AV block
c) Ventricular tachycardia
d) Atrial fibrillation
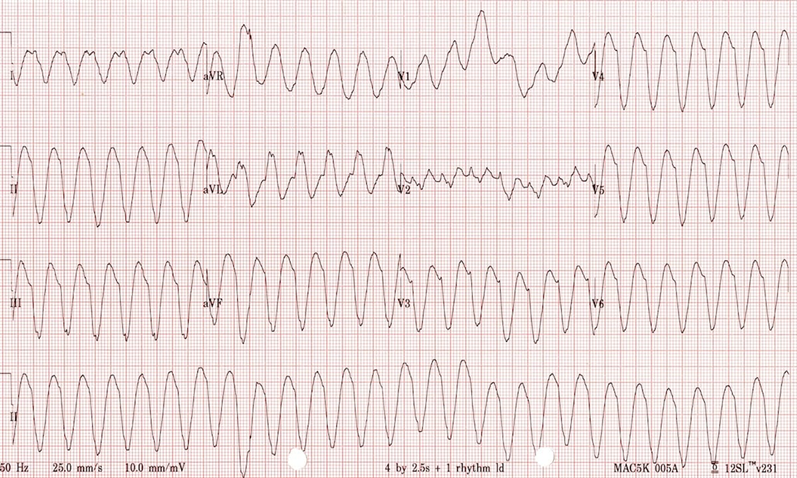
10) What is the first and best intervention used to convert this rhythm to one which is compatible with life?
a) Adrenaline 1 mg IV push
b) Adrenaline 1 mg down intubation tube
c) Shock
d) CPR 30 compressions: 2 breaths
In addition to the above 10 post-test questions, please take five minutes to
answer the following reflective questions:
1) How satisfied were you with this simulated suite?
Not very helpful 1-------- 2 -------- 3 -------- 4 -------- 5 Very helpful
How did the suite of scenarios affect your knowledge base in dealing with
deteriorating situations?
Not very helpful 1 -------- 2 -------- 3 -------- 4 -------- 5 Very helpful
How did participating in this suite of scenarios affect your confidence in
dealing with deteriorating client situations?
Not very helpful 1 -------- 2 -------- 3 -------- 4 -------- 5 Very helpful
How did participating in this suite of scenarios affect your ability to work in a
team?
Not very helpful 1 -------- 2 -------- 3 -------- 4 -------- 5 Very helpful
2) Which role did you play in this scenario, and was it harder or easier than
the other roles? Please tell why below.
a) Recorder of data and calling ISBAR report
b) Assessment of relevant system and medications
c) Vital signs repeatedly and securing airway and oxygen devices
3) Which role do you think is hardest to master and why?
4) What was the least valuable aspect of your learning today? What changes
would you make?
5) If the world were perfect and you could have whatever you desired, how
would you alter what happened today to maximise your learning in simulation?