Acute Type A Aortic Dissection—Replacement of Ascending Aorta, Aortic Arch and Antegrade Stenting of the Descending Thoracic Aorta Using the Thoraflex™ Hybrid Plexus Device (Terumo Aortic)—“Frozen Elephant Trunk”: The Plymouth Way! ()
1. Introduction: Background
Acute Type A Aortic Dissection (AAAD)—Stanford Classification—remains a catastrophic event with a high surgical mortality. Based on Data from The International Registry of Acute aortic Dissection (IRAD) the mortality of patients treated surgically was 26% and for those managed medically was 58% [1].
Traditionally Acute type A Aortic dissection has been treated by a conservative replacement of the ascending aorta with or without Aortic root surgery. However, a number of patients re-present in the years following their emergency surgery with aneurysmal dilatation of the false lumen, particularly in the distal arch and proximal descending aorta. This is a difficult problem to manage. Our unit has therefore moved towards total arch replacement in concert with replacement of the ascending aorta in patients presenting with Acute type A Aortic dissection. The advent of the ThoraflexTM Hybrid Plexus Device has made this a more feasible proposition. We have refined the implantation technique to suit its deployment under these challenging circumstances. We describe below our technique, which has now been utilized in over 30 patients with acute Type A dissection in our unit.
2. Surgical Technique of FET
The surgical steps of the technique are described below as the following:
· Surgical incisions—Initiation of cardiopulmonary by-pass (either femoral or right axillary), venting of the Left ventricle with a transmitral vent via the right superior pulmonary vein.
· Cooling to 20 degrees Celsius, dissection of aortic arch plus supra aortic branches.
· End to side graft extension of the left subclavian artery.
· Preparations for antegrade continuous cerebral perfusion
· Initiation of cardioplegic arrest prior to circulatory arrest, with semi continuous antegrade cardioplegia delivery thereafter.
· Corporal Circulatory arrest at 20 degrees Celsius
· Antegrade deployment of the stent graft into the descending Aorta. Completion of Distal suture line.
· Recommencing antegrade corporal by-pass perfusion through the side branch of the graft while maintaining 1) antegrade cerebral perfusion via the left carotid and the innominate artery and 2) cardiolplegia administration through the coronary ostia.
· Sequential anastomoses of the left common carotid and innominate arteries to their respective graft side branches, whilst maintaining antegrade cerebral perfusion throughout.
· Anastomosis of the extension of the left subclavian artery with the most distal branch of the main Thoraflex graft.
· Rewarming while performing the proximal part (root and ascending aortic surgery as required).
3. Operative Technique
3.1. Team Brief and Surgical Incisions—Initiation of Cardiopulmonary Bypass
Operative plans are carefully discussed with the theatre team before commencing the operation. The anaesthetist will wish to set up both right radial and left femoral arterial monitoring lines. Cerebral oximetry recorders are applied. The perfusionist will need to cut in an additional “y-line” to their arterial return for the cerebral circuit. The prosthesis is chosen; the stent portion diameter being based on careful consideration of the descending aortic landing zone. In the setting of the acute dissection we do not upsize at all.
Draping of the patient must facilitate access to the right axillary artery, the side of the neck and the femoral arteries.
Depending on the urgency and pathology of the procedure, access for arterial return may be to the femoral artery or to the right axillary artery. Generally we do choose the femoral artery if the patient is unstable.
A median sternotomy with extension along the medial border of the left sternocleidomastoid muscle is routinely performed. Venous return is achieved via a 2 stage venous cannula through the right atrium. Cooling towards 20 degrees is initiated. A left ventricular vent is inserted via the right superior pulmonary vein.
3.2. Cooling, Dissection of Aortic Arch Plus Supra Aortic Branches and Addressing the Left Subclavian (Figures 1-3)
Dissection of the innominate (brachiocephalic) vein, innominate, left common carotid and left subclavian arteries proceeds while the patient is being cooled. We do not divide the innominate vein in our center but are aware that others do so routinely. Meticulous haemostasis is maintained at every stage. A generous neck incision greatly aids the deeper dissection towards the left subclavian artery.
Our attention is turned to the left subclavian artery itself. Although deeply placed, it is usually surprisingly mobile. After placing a sling around it, the vessel can often be displaced advantageously towards the surgeon with gentle traction, facilitating exclusion of a suitable length from its origin, enabling grafting with the 5 cm long extension graft. This is usually “harvested” from the 8 mm distal side limb of the Thoraflex prosthesis.
The anastomosis is performed by first clamping the SCA origin flush with the arch. A more distal clamp is then applied. This can be angled by the assistant if required to further help display the artery. After making a small incision with a
![]()
Figure 1. Dissection of aortic arch plus supra aortic branches.
![]()
Figure 2. Addressing the left subclavian.
![]()
Figure 3. Addressing the left subclavian.
size 11 blade at least 1 cm distal to the proximal clamp, the 4 mm punch is used repeatedly to make a suitable anastomotic site. An end to side anastomosis to the extension graft is then performed with 5/0 Prolene. The distal clamp is then removed to de-air the graft, which is then left clamped for later use. The origin of the native subclavian artery is now ligated flush with the arch with a heavy suture. If the surgeon choose to proceed to ligation later on, once the extension has been joined to the Thoraflex prosthesis we should make sure that subclavian artery remains clamped during antegrade cerebral perfusion.
3.3. Preparations for Total Circulatory Arrest (Figure 4)
Small cannulae (Medtronic DLP 14 Ga 7 Fr and 5 Fr) are now placed into the innominate and left common carotid arteries. We use cardioplegia cannulae placed through 5/0 Prolene purse strings. These are placed as far from the respective origins as feasible (3 cm should suffice). Great care must be taken, especially with the LCCA, not to inadvertently puncture the posterior wall during placement. Partially withdrawing the introducer-stylette can help here, thus reducing the distance needed to pass the cannula portion into the lumen. If the origins are dissected, more distal dissection is required to access a non-dissected portion of the arterial wall.
The cerebral perfusion line is now de-aired and connected to the two cannulae through a y-piece.
Once the target temperature has been reached (20 degrees Celsius), flow is reduced to a quarter prior to cross-clamping the ascending Aorta. Ascending aorta is clamped and opened proximally. Cardioplegia is then administered directly into the coronary ostia via ostial cannulae which are held in place with 4/0 purse strings. Cardioplegia is thereafter run semi-continuously into them for the duration of the arrest period.
Antegrade perfusion is now commenced into the innominate and left common carotid arteries, as their origins are clamped. Only now can corporal arrest
![]()
Figure 4. Preparation for antegrade cerebral perfusion.
begin. Note, at no stage has air gained access to the origins of the innominate or left common carotid arteries. The clamp on the ascending aorta is removed and the arch resected to zone two (just proximal to the origin of the left subclavian artery).
3.4. Antegrade Deployment of the Stent Graft of the Descending Aorta and Distal Suture-Line (Figure 5)
The Thoraflex prosthesis is then gently curved and deployed under direct vision into the true lumen of the distal arch and descending aorta. We are aware that some teams wish to confirm the identity of the true lumen with a pre-placed guidewire from the femoral artery but this has not been our practice. The “skirt” is then sewn to the aortic rim with 4/0 Prolene, incorporating a strip of Teflon felt if necessary.
3.5. Recommencing Antegade Cardiopulmonary By-Pass through the Side Branch of the Graft While Maintaining Antegrade Cerebral Perfusion via the Left Carotid and the Innominate Artery
Once the distal (zone two) anastomosis is complete, we proceed to de-air the descending aorta with slow and gradual retrograde perfusion from the femoral cannula (if utilized initially). The arterial return is simply moved to the anterior side branch of the prosthesis and antegrade perfusion is slowly commenced. De-airing continues through the proximal limb and side branches of the Thoraflex graft. The side branches are sequentially clamped, as is the proximal end of the graft, as full corporeal perfusion is re-commenced. Antegrade cerebral perfusion via the left carotid and the innominate artery cannulae continues uninterrupted.
At this stage, the zone two anastomosis is carefully inspected for leaks. Additional sutures are easily placed, on reduced pump flow as required.
![]()
Figure 5. Preparations for stent graft deployment.
3.6. Connecting the Left Common Carotid and Innominate Arteries to the Middle and Proximal Side Branches of the Thoraflex Graft While Maintaining Antegrade Cerebral Perfusion (Figure 6)
The LCCA and innominate arteries are now anastomosed to their respective graft side branches, with 5/0 Prolene. These anastomoses are performed proximal to the perfusion catheters, between clamps, thereby maintaining antegrade perfusion throughout. Each graft is de-aired and then perfused from the Thoraflex graft in turn. The antegrade cerbral perfusion cannulae can now be removed as antegrade perfusion continues, now directly from the Thoraflex graft.
3.7. Anastomosis of the Graft Extension of the Left Subclavian with the Most Distal Branch of the Main Thoraflex Graft (Figure 7, Figure 8)
5/0 Prolene is again used to perform an end to end anastomosis between the LSCA graft extension and the most distal branch of the Thoraflex graft. The graft is de-aired and opened. All anastomoses are carefully inspected for haemostasis.
![]()
Figure 6. Completion of the anastomosis of the supra-aortic branches (Left carotid and Innominate artery).
![]()
Figure 7. End to end anastomosis of the graft extension of the left subclavian.
3.8. Rewarming While Performing the Proximal Part (Ascending Aorta, Root, Graft to Graft etc.)
Re-warming will already have been commenced as the arch anastomoses are being performed. The target temperature at this stage will depend on plans for the aortic root. If no further interventions are required, re-warming towards normothermia is initiated. In acute dissections, re-suspension of the aortic valve with plegetted 4/0 Prolene sutures across the tips of the commissures is usually required, but extensive root procedures (valve-sparing or full root replacements) are not uncommon. A separate proximal graft is usually anastomosed to the sinotubular junction. This facilitates fashioning of a kink-free ascending aortic angle by bevelling the two grafts before anastomosis. Attempting to join the proximal limb of the Thoraflex graft directly to the STJ will otherwise almost certainly result in an unsightly fold across the back wall.
Finally, de-airing of the heart and proximal graft is performed prior to release of the cross clamp from the Thoraflex proximal limb. Haemostasis is performed as the patient is brought up to normothermia. An additional period at normal temperature on bypass is employed to reduce aftercooling following weaning from bypass.
4. Discussion
The management of acute Stanford Type A Aortic Dissection (AAAD) is currently under review. Untreated, the condition carries a high risk of early mortality; from tamponade, coronary artery compromise or torrential aortic regurgitation. Operative mortality is also significant, varying between 2.8% to 47.6% in different centers as is concluded in Gavin Murphy’s meta-analysis [2].
In most cardiac centers, the surgical management of AAAD comprises the replacement of just the ascending aorta, with or without aortic root repair or replacement. While the primary tear is often in the ascending aorta, the dissection commonly propagates up to and beyond the aortic bifurcation. Consequently, such patients surviving the initial operative procedure remain at risk from aneurysmal dilatation of the false lumen, often in the distal arch and aortic isthmus. Pochettino and colleagues state: “This ‘proximal’ strategy leaves most patients with a patent residual ‘type B’ dissection which leads to greater than 30% distal reoperations or re-interventions for dissecting aneurysm” [3]. In the series of Rilski et al. (multicentre analysis) among the survivors of type A Aortic dissection 36% of the patients required Aortic re-intervention distally to the ascending graft in a follow up period of 15 to 52 months [4].
Our own experience supports this. Whilst the re-intervention rate is not as high as 30% in our own population of AAAD patients, these re-interventions are technically challenging and carry both a large burden of morbidity for the patient and a sizeable impact on the cardiac surgical unit.
“The distal problem” has led groups from Japan and elsewhere, to suggest total arch replacement [5] from the outset in patients presenting with De Bakey Type 1 AAAD—or even more aggressively—utilising the “elephant trunk technique” [6], first introduced by Borst and colleagues in 1983 [7].
Kato was the first to describe the use of a graft with an integrated distal stent portion as an amendment to the conventional floating elephant trunk procedure in 1996 [8].
Karck coined the term “frozen elephant trunk” (FET) in 2003 [9], referring to the fact that the expanding stent portion within the proximal descending aorta is constrained from movement by its radial force against the aortic intimal surface. It is this radial force which, gently applied, can lead to the obliteration and thrombosis of the false lumen throughout the length of the stented portion. Whether or not this subsequently leads to complete remodelling of the more distal dissected aorta remains to be seen, and no doubt depends on the presence of distal communications between the true and false lumens.
Early results suggest that the FET technique is associated with satisfactory outcomes in terms of hospital mortality (10.0%), stroke (4.8%) and spinal cord injury (4.3%). High rates of partial/complete thrombosis of the persistent false lumen (88.9%) have been reported [10].
The advent of the hybrid devices now available for arch replacement and stent exclusion of the proximal descending aorta (FET) has opened the way for reproducible and safer extended repair of AAAD. The zone 2 anastomosis is relatively straightforward and haemostatic thanks to the obliteration of the false lumen downstream. Our method of continuous antegrade cerebral perfusion while this anastomosis is being performed limits the insult to the brain. The difficulties commonly associated with the left subclavian anastomosis have been largely overcome by our adaptation to an end-to-side anastomosis during the cooling phase. Our total operating time is not dissimilar to that for the traditional ascending aortic replacement for the same condition and the corporeal arrest time is often shorter. We are not suggesting that it is any less challenging but it offers the advantage of a complete repair, with a lower likelihood of later re-interventions.
5. Conclusions
The main goal of our approach has been to produce a reproducible and safe method to extend the treatment of AAAD to exclude the pathology within the arch and proximal descending aorta. In addition, it leaves a safe landing zone for future stent graft extension should that be required.
The results of AAAD surgery have remained modest at best, with a sizeable proportion of survivors needing subsequent major interventions. We agree with Roselli et al. [11] that the FET combines the advantages of open aortic surgery— completely resecting and replacing the dissected aortic arch, with the advantages of the endovascular approach—in covering the intimal tears with the stented portion of the graft. Not only does it prioritize flow into the true lumen within the descending aorta but it appears to encourage thrombosis of the false lumen there too.
We believe that our operative technique is a systematic and straight forward approach that should be reproducible in any aortic surgeon’s hands and—assuming that is being applied consistently—can facilitate the training of less experienced surgeons in the complex field of aortic arch surgery.
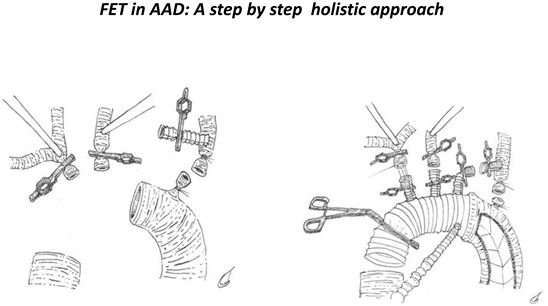
Graphical Abstract
Acknowledgements
Artist credit: Illustrations by Charlie Bonning.