1. Introduction
Postpartum hemorrhage (PPH) is defined as blood loss of ≥500 ml after vaginal delivery or ≥1000 ml after caesarean section. Major PPH can be divided into moderate at 1000 - 2000 ml or severe at over 2000 ml. Severe PPH is also defined as a fall in hemoglobin of ≥40 g/l or the need for transfusion of 4 or more units of red blood cells (RBC) [1] . Massive PPH has been described as bleeds of more than 2500 ml and is associated with significant morbidity, even in resource-rich countries, including admission to high dependency and intensive care and emergency hysterectomy (6% - 8% of cases) [2] . PPH is a major cause of maternal morbidity and mortality. Worldwide PPH accounts for at least 30% of all maternal deaths [3] . Death from PPH occurs in about 1 per 1000 deliveries in low-resource countries compared with 1 in 100,000 deliveries in higher-resource countries [4] . PPH is estimated to occur in between 1% and 5% of deliveries [1] [5] , but incidence estimates vary by definition. Globally, Calvert et al. reported PPH prevalence at 10.8% (95% CI: 9.6 - 12.1) in a systematic review and meta-analysis, with wide regional variation ranging from 7.2% (95% CI: 6.3 - 8.1) in Oceana to 25.7% (95% CI: 13.9 - 39.7) in Africa [6] . In our article, we have 130 patients out of a total of 7705 deliveries with a rate of 1.7% compared to the rates described in the literature [1] [5] [7] . This kind of accident is one of the biggest emergencies in obstetrics that we can predict only in some specific cases, but usually, we are caught unaware. So to avoid a maternal, fetal or both disastrous evolution, we have to be able to act quickly and effectively, for these reasons we have developed two new surgical techniques.
2. Surgical Management of PPH
Failed medical and mechanical approaches to management of PPH warrant surgical exploration [8] . The surgical approach differs by delivery method, suspected etiology and clinical status [9] . The surgeon must decide if a laparotomy in case of vaginal delivery after a quick and a careful exploration of the lower genital tract or re-laparotomy after cesarean section, to identify the cause of PPH and make the decision of a conservative or a radical treatment. Placement of uterine compression sutures in a suspender fashion to promote uterine contractility may be a useful initial attempt at bleeding cessation while preserving fertility. Compression sutures should be used as a first step in surgical management when hemorrhage is a result of atony. The most described uterine compression sutures are B-Lynch procedure or Cho suture, carried out if a hysterotomy has been performed (delivery via cesarean section) and Hayman suture in the absence of a hysterotomy (vaginal delivery), is technically less challenging than vessel ligation and results in less morbidity than a hysterectomy [8] . Alternatively, the uterine or the internal iliac arteries can be ligated bilaterally to temporarily decrease blood perfusion to the uterus. While ligation of the internal iliac arteries was once more common, uterine artery ligation is now favored for ease of identification and higher success rates (80% - 96%) [10] .
In the same purpose, we have elaborated two techniques, the first one can be considered as compressive suture, we called it “uterine isthmic plicature or A-Loutfi procedure” and the second technique is a wide lateral uterine vascular ligation named B-Loutfi procedure.
-Uterine Isthmic Picture (Loutfi-A procedure).
Description of the Uterine Isthmic Plicature (A-Loutfi procedure):
This technique consists of performing a large compressive suture, performed after doing the hysterorrhaphy. In fact, we use a delayed absorbable multifilament suture, that crosses the anterior uterine wall (out-in) from the upper side to the lower one of the right edge of the cesarean section scar, then we pull the multifilament to the other edge and we insert the curved needle from the lower side (out-in) to the upper side (in-out) of the left edge of the hysterorrhaphy by crossing the anterior uterine wall only, so as we don’t affect the uterine cavity integrity. At the end we tie a knot at the middle of the superior part of the hysterorrhaphy as shown in Figure 1 and Picture 1. It helps so tightening the
![]()
Figure 1. Diagram describing the first technique.
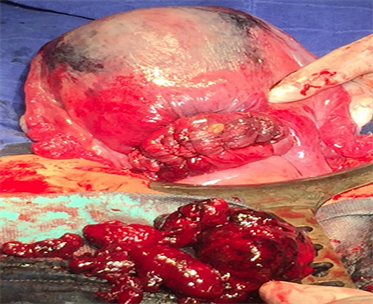
Picture 1. Photo showing the appearance of the uterus after performing the first technique.
weakest part of the uterus: the lower segment. The weakness of this segment is due to its distention at the end of pregnancy. At the same time, this anterior uterus wall “tie” helps narrow the uterine arteries lumen by tracting both left and right uterine arteries medially and also it helps lifting the anterior wall of the uterus and at the same time narrowing the uterine cavity. The merit of this technique in comparison with other compressive suturing techniques as Cho’s multiple square suture, B-Lynch “Brace” suture, Hayman suture, Matsubara-Yano suture and many others described in literature [11] - [19] is that: it preserves the integrity of the uterine cavity, it’s easy to perform with an average time estimated at 3 minutes (4 - 5 minutes) and until the writing of this article we have not observed any complication at all. We usually decide to use this technique in moderate cases of postpartum hemorrhage and we are going to show in base of statistics its usefulness.
-Wide lateral uterine vascular ligation (B-Loutfi procedure).
Description of the wide lateral uterine vascular ligation.
(B-Loutfi procedure):
This procedure consists of performing a large vascular ligation. Technically, we begin by inserting the needle in the posterior face of the uterus 2 cm medially to the lateral border, 1 cm under the insertion of the utero-sacral ligament, after the needle crosses both layers of the uterus, we take it out anteriorly to join the upper part of the broad ligament just above the medial fallopian artery that we can identify by transparency, as shown in Figure 2 and Picture 2. The difference with other uterine vascular ligation is that we ligate in one suture: the uterine artery, the uterosacral ligament, the round ligament and all the lateral uterine vascular ramifications. With this large ligation we suppress widely the uterus blood affluence while preserving the Fallopian tube. All this in an average time of 5 min (4 - 6 min).
![]()
Figure 2. Diagram describing the 2nd technique.
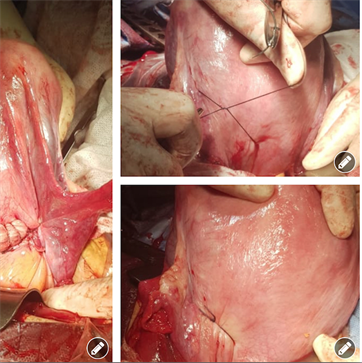
Picture 2. Assembly of 3 photos, showing the appearance of the uterus after the completion of the 2nd technique.
Both techniques are easy to reproduce and to learn and can be a solution for the problem reported by Pierre-Emmanuel Bouet: “An alarmingly high number of French senior residents in Obstetrics and Gynecology report that they have not acquired the sufficient surgical skills during their training to be able to perform the surgeries required for the management of postpartum hemorrhage” [20] .
3. Results
130 patients presented a postpartum hemorrhage treated surgically out of a total of 7705 patients that we delivered during a period of one year (2018-2019) with a rate of 1.7% comparable to literature [1] [5] [7] [21] .
We separated our patients into two distinguished groups: A and B.
- Group A: we have performed the first technique on the 90/130 patients (69%) with a hemodynamic stabilization and an immediate stop of hemorrhage. These patients have been followed for their pregnancies at our hospital and have been admitted from the beginning of their labor till they delivered. 70 patients (54%) of this group delivered normally after what they presented uterus atony. 20 patients (15%) did have a cesarean section, with 12 intervention for fetopelvic disproportion, 5 for fetal malposition and 3 operations for multiple pregnancies. The mean blood loss in the 70 patients that presented a secondary postpartum hemorrhage after delivering normally was 750 ml (700 - 800), with a hemoglobin average at 11 g/dl (10 - 12 g/dl) and because the treatment was quick and efficient, we have been obliged to perform a blood transfusion in only 10 patients because their hemoglobin at admission ranged between 10 and 11 g/dl (2 packed red blood cells). For the 20 patients who delivered by cesarean section in this A-Group, the hemoglobin average was 10.5 g/dl (9.6 - 11.4 g/dl). The blood loss ranged between 1.2 L to 2.3 L and we decided the success of the first technique on the basis of hemodynamic parameters stabilization. We decided blood transfusion in only 3 patients (multiple pregnancies, because of their hemoglobin at admission: 9 - 10 g/dl). We decided to transfuse 3 packed red blood cells.
- Group B: this group includes 40/130 patients (31%), all these patients were transferred to us from other hospital structures because we are in a referral hospital. With 37 patients who benefited of the combination of the two techniques (A-Loutfi procedure and B-Loutfi procedure) as already mentioned above, because they arrived with a severe post partum hemorrhage, showing signs of hemorrhagic shock on admission and the first procedure has not been sufficient because of persistence of hemodynamic parameters instability, so we have been obliged after only 10 minutes to add the second procedure. Both techniques were efficient and stabilized the patients with no need to transfer them to the intensive care unit. But we must specify that we
Transfused 22 patients with 4 packed red blood cells and 4 fresh frozen plasma, because they have been admitted with signs of shock. In 15 patients we transfused 02 packed red blood cells and 2 fresh frozen plasma, because their intake hemoglobin ranged between (6 - 8 g/dl). 02 patients were presenting clinical symptoms of uterine rupture on their arrival, confirmed when laparotomized and because they presented complicated cases of uterine rupture, we performed subtotal hysterectomy. The last patient was presenting on admission a disseminated intravascular coagulation, confirmed biologically later and in spite of performing the uterine isthmic plication combined to the wide lateral uterine vascular ligation we have been obliged to do the subtotal hysterectomy and transfer her to the intensive care where she benefited from transfusion of 07 packed red blood, 10 fresh frozen plasma, 10 concentrated platelets and the second day in intensive care unit she presented an acute renal failure, so she beneficiated from renal dialysis sessions.
4. Discussion
The results of our study allow us to note, that our conservative techniques helped saving life of 127/130 (98%) patients with uterus preservation, Concerning the 3 remaining patients, 2 of them were presenting complicated uterine rupture and the last one was presenting disseminated intravascular coagulation, so we have been obliged to perform a subtotal hysterectomy. Our rate is well ahead of other vascular ligation and uterine plication as reported in literature by J. B. Haumontéal and all [22] : “Conservative surgical treatment has a 70% efficacy to stop hemorrhage whatever treatment used (vascular ligature or hemostatic brace suturing)” and Salvat Jilateral [23] who reported that, bilateral ligation

Picture 3. Two uterine vaginal ultrasounds showing the absence of isthmocele.
of the hypogastric artery can provide success in 66% of cases. Other articles reported rates less than our as Hüseyin Cengiz and all [24] : “Organ preserving surgery methods were utilized in all the patients with a success rate 78.9%”. In addition to the absence of any of the complications described in literature [11] - [19] , we noted during the follow-up, another benefit, which is the absence of isthmocoel in all patients with a median follow-up of 12 months, as shown in Picture 3.
5. Conclusions
We can conclude that with a success rate of 98% our easy techniques are indeed efficient, not expensive and not requiring large logistics. We can also add that with an average follow-up of 12 months, we haven't seen any of the usual complications expected in such techniques as: hematometry, amenorrhea, necrosis or dehiscence and even no isthmocoel. Another study is underway for a longer follow-up period.
We must emphasize that the management of postpartum hemorrhage is not only dependent on one or two surgical techniques, but above all, on a quick diagnosis, as well as a good responsiveness of the whole care team.