The Effect of Aging on Pelvic Floor Pressure Measurements in Nulliparous Women ()
1. Introduction
Age is an established risk factor for both pelvic organ prolapse (POP) and urinary incontinence [1] [2] [3] [4]. Both of these onerous ailments are linked to pelvic floor muscles’ (PFM) function: PFM strength negatively correlates with risk of POP [1] and its strengthening is found to improve symptoms of urinary incontinence [5]. Levator ani muscle is the main muscle of the pelvic floor: the Puborectalis part pulls the pelvic structures ventrally and cranially and decreases the levator hiatus area to prevent prolapse of the pelvic organs [4] [6] - [11]. Pubococcygeus and Iliococcygeus parts assist in achieving urinary and fecal continence. Resting levator ani activity depends on the load placed on it; but the resting tone of the levator ani muscles in healthy women is constant tension until prompted to relax during urination, defecation, and intercourse. The levator ani muscles co-activate with the abdominal muscles and the diaphragm to resist the rise in intra-abdominal pressure (Valsalva maneuver) which may lead to vaginal prolapse, urinary and fecal incontinence [12].
Assessment of PFM contractility is a potential clinical tool to assess pelvic organ prolapse symptoms [13]. Vaginal manometry has been used in the past as a method to assess PFM strength [14] [15] [16] due to its acceptable inter-rater reliability of at least 90% [16] [17]. The vagina is surrounded by PFMs like a funnel [18]. Therefore, 3D vaginal manometry can be useful in measuring the PFM pressure; it can show the vaginal high pressure zone, which represents vaginal constrictor function. 3D vaginal manometry can also measure the elevator function of pelvic floor using the cranial movement of the posterior pressure cluster [19]. We hypothesized that increased pelvic floor symptoms are associated with increased vaginal manometry measurements. Our main goal in this study was to investigate the correlation between age and 3-D vaginal manometry parameters in nulliparous women. Our secondary goal was to correlate changes in vaginal manometry to sexual function, prolapse and urinary status. We used the detailed Pelvic Floor Distress Inventory (PFDI-20) to assess patients’ pelvic floor function, Pelvic floor impact questionnaire (PFIQ-7) to assess the patient’s quality of life [20], and Female Sexual Function Index (FSFI) to assess the quality of sexual activity [21].
2. Methods
This was a cross-sectional study approved by the Institutional Review Board of Inova Health System in Falls Church, Virginia. The study recruited only nulliparous women through INOVA system-wide advertising via Inova Net webpage and Inova Health System “Five-in-Five” email. The sample size was small as this was a pilot study with seed grant funding available through Inova Health System. The patients were dichotomized into two groups; young 18 - 40 years and old 52 - 85 years. Participants signed an informed consent before participating in the study; the consent document informed participants that the study would not diagnose or treat any injuries or anomalies in any way. Recruitment took place between March 2017 and December 2017. Exclusion criteria included a history of prior incontinence or prolapse surgery, a diagnosis of reproductive anomalies, prior pelvic radiation, or inability to complete written questionnaires. The following variables were obtained at the study visit: age, height, weight, body Mass Index (BMI), race, and ethnicity and history of chronic medical illness. All participants then completed Pelvic Floor Distress Inventory (PFDI-20), Pelvic floor impact questionnaire (PFIQ-7), and Female Sexual Function Inventory (FSFI) (Appendix 1). The PFDI-20 questionnaire we used was the validated form that constitutes three sections: pelvic organ prolapse distress inventory (POPDI-6), colorectal-anal distress inventory (CRADI-8), and urinary distress inventory (UDI-6). UDI-6 was additionally analyzed separately as a reliable indicator of bladder function. The questionnaires are standard to the field of urogynecology. After finishing the questionnaires, participants underwent 3-D endovaginal manometry by the senior author (SAS), who was blinded to the questionnaire scores. The device used was a ManoScan™ ESO high resolution 3D manometry system (Medtronic plc, Minneapolis, MN). The device’s probe was 10 mm in diameter with 64mm pressure sensitive length. The 256 transducers on the surface of the probe formed continuous grid in both axial and circumferential directions, each transducer being 4 mm long (axially) and 2 mm wide (circumferentially). Pressure measurements from all transducers were recorded digitally and displayed on a personal computer as color plots. In vitro testing has revealed that an externally applied pressure on each transducer does not influence the output of the adjacent transducer and pressure recordings have an accuracy of 5mm Hg.
The probe was placed in the vagina in such a fashion that the entire vaginal high pressure zone was captured; the most cranial part of the probe recorded abdominal pressure and the most caudal part measures the atmospheric pressures. The circular orientation of the probe in relation to the anterior midline, posterior midline, and left lateral and right lateral orientation of the vagina were noted (Figure 1). This methodology has been previously reported for evaluation of vaginal high pressure zone [19].
1) Subject completely relaxed her pelvic floor muscles (resting pressure).
2) Subject was told to contract the pelvic floor muscles as if obstructing urination or defecation, similar to Kegel exercises (squeezing pressure).
3) Subject was told to push as in trying to defecate (Valsalva pressure).
Maximum pressure was recorded twice for each conditions and average of the two measurements was calculated.
Statistical analyses: Absence or presence of sexual activity was analyzed separately as a dichotomous variable. FSFI-19 scores were evaluated only for those who were sexually active as an indicator of the “quality” of sexual activity. We used two-sample t-test to assess mean differences in the young versus the older participants. Chi-squared test was used to analyze dichotomous data in the two groups. In a separate analysis, the two groups were merged and logistic and linear regression analysis was used to assess correlations. A 95% confidence interval (CI)
![]()
Figure 1. 3-Dimensional vaginal manometry plot during Valsalva maneuver of an older participant (left) compared to a younger one (right). The arrows areas are the posterior and the anterior wall in which higher pressure (red color) was generated in the older patient compared with the younger (blue-green color).
was applied and a p-value of less than 0.05 was considered significant for all analyses. Analysis of co-variances (ANCOVA) was used to adjust for potential confounding factors in group studies. Multiple regression analysis was used to adjust confounding factors in regression models. All statistical analyses were performed using Stata/IC version 14.2 (StataCorp LLC, Texas).
3. Results
Twelve young pre-menopausal and ten older post-menopausal (defined as amenorrhea for more than a year) patients were recruited. The manometry of three participants recruited into the young group showed negative or zero results because of equipment error and these were excluded. Those were considered incorrect measurements and were excluded. The young group had a mean age of 28.6 years (95% CI 24.3 - 32.9) and the older group had a mean age of 61.8 years (95% CI 55.8 - 67.8). All participants in the older group were postmenopausal, all young participants were premenopausal. BMI was significantly higher in the older group: 24.2 vs. 30.9, p = 0.026 and was positively correlated with menopausal status (OR = 1.194, p = 0.034). None of the participants were on hormone replacement therapy. There were no significant differences between the two groups in terms of race (white vs. non-white), and presence of chronic medical conditions.
Manometry results: No significant differences between the manometry measurements were found between two groups at rest and squeezing. During Valsalva, however, the pressures measured at the anterior, posterior, and left walls of the vagina were greater among the older group (p = 0.015 0.028, 0.024, and 0.022, respectively) (Table 1). After correction for BMI using ANCOVA, the difference remained significant (corrected p = 0.021 0.033 and 0.030, respectively).
![]()
Table 1. Comparison of the pressure measurements in young vs. old group. Means, standard deviations (SD), median and p-values (calculated using t-test) of each group are presented. Pressures are reported in mmHg and are rounded to nearest integer due to device accuracy of 5 mmHg. Zeros without a decimal are absolute zeros. BMI = Body Mass Index (kg/m2), PFDI-20 = Pelvic Floor Disability Index (range 0 - 300), POPDI = Pelvic Organ Prolapse Distress Inventory (range 0 - 100), CADI = Colorectal Anal Distress Inventory (range 0 - 100), UDI-6 = Urinary Distress Inventory (range 0 - 100).
Pelvic floor function assessment: PFDI-20 score was significantly higher in the older group: mean 51.7 (95% CI 23.6 - 79.7) versus 4.0 (95% CI 0.0 - 13.3), p = 0.001. Regarding the bladder function evaluated by the UDI-6 part of the PFDI-20, we found that UDI-6 score was also higher among the older group 28.3 (95% CI 9.7 - 47.0) versus 2.8 (95% CI 0.0 - 9.2), p = 0.006. All young participants scored zero in their PFIQ-7 while the older participants averaged 31 (out of 300) (Table 1). ANCOVA analysis revealed significant difference in PFDI-20 and UDI-6 scores after correction for BMI (BMI was defined as an ordinal independent variable): corrected p = 0.001 and 0.005, respectively. Fewer participants in the older group were sexually active, 8/9 (89%) young participants were sexually active vs only 6/10 (60%) older participants (p = 0.153). Mean FSFI-19 score was not significantly different between the two groups after excluding those who were not sexually active.
Logistic and linear regression analysis: The two groups were merged for logistic and linear regression analysis of age versus other variables. Age was not correlated with BMI, race, or history of chronic medical illness. Sexual activity (as reported via the FSFI question: sexually active/not active) was negatively correlated with age (OR = 0.92, p = 0.029). FSFI score did not correlate with age. Age positively correlated with PFDI-20 scores (r2 = 0.327, p = 0.010) and UDI-6 scores (r2 = 0.252, p = 0.029). Age was correlated with sum of Valsalva pressures of all four vaginal walls (r2 = 0.256, p = 0.027) (Table 2). Moreover, linear regression analysis revealed a positive trend between PFDI-20 scores and the sum Valsalva pressure measurements (r2 = 0.202, p-value = 0.0616).
4. Discussion
The increased Valsalva pressure in older subjects is possibly due to increased conduction of intraabdominal pressure to the pelvic organs while performing Valsalva. Valsalva pressure is mostly generated by abdominal wall and diaphragm
![]()
Table 2. Logistic and linear regression analyses using age as a predictor (independent variable). Pressures are reported in mmHg and are rounded to nearest integer due to device accuracy of 5 mmHg. OR or r2 = Odds ratio (OR) is reported for binary data and R-squared (r2) is reported for linear data, β = standardized coefficient, BMI = Body Mass Index (kg/m2), PFDI-20 = Pelvic Floor Disability Index (range 0 - 300), POPDI = Pelvic Organ Prolapse Distress Inventory (range 0 - 100), CADI = Colorectal Anal Distress Inventory (range 0 - 100), UDI-6 = Urinary Distress Inventory (range 0 - 100).
muscles and conducted through pelvic floor muscles, pelvic floor and vaginal soft tissues to the manometry transducers. An increase in the Valsalva pressure by aging as found in this study, might indicate impaired function of PFM or changes in the pelvic floor soft tissues elasticity (or both). Resting and squeezing pressures were not significantly changed by age in our set of nulliparous women. Since we attribute resting and squeezing pressures to the strength of the levator ani muscles, we can conclude that those two measurements are slightly but not significantly decreased with aging and in the absence of a history of vaginal deliveries. We can therefore assume that changes in the Valsalva pressure are not due to declined PFM function, rather due to change in pelvic soft tissue elasticity (Figure 2).
Age was also significantly correlated with urinary and prolapse symptoms assessed by the PFDI-20 and quality of life as seen according to the PFIQ-7 scores; a coefficient of 1.2 means that for every year increase in age there will be about 1.2 point increases in the PFDI-20 score. This is particularly interesting because all of our participants were nulliparous; therefore, the significant decrease in PFM ability to resist intraabdominal pressure could not be attributed to the levator ani damage caused by childbirth.
All older patients in our group analysis were post-menopausal while all of the younger patients were pre-menopausal. Therefore, menopausal status might be one of the etiologies contributing to the observed changes in the pelvic floor. By design, in this study we chose patients who were dichotomized by age and menopausal status. We did not enroll the intermediary premenopausal group that could have confounded our findings. Because the study was small and we did not look at serum hormone levels we were unable to separate the effects of aging from that of hormonal changes. Further, we cannot comment on subject’s hormonal status since post-menopausal status was made based on patient’s history.
![]()
Figure 2. This funnel model, illustrates the transmission of the abdominal pressure to the Levator Ani Muscle (LAM) and vaginal walls during Valsalva. The pressure is transmitted and absorbed firstly at the Delaney’s Levels I and II supports, and afterwards, in the LAM and the vaginal walls. (A) Illustrates the normal pelvic floor in a young woman with intact levels I/II. (B) illustrates weakened the sagged connective tissues (Level I/II) in an older woman, so that less pressure is supported partially via those levels and more pressure in the transmitted to probe (P). USL: Utero-Sacral Ligament, LAM: Levator Ani Muscle.
Our two groups were significantly different in BMI; however, using ANCOVA and multiple regression tests, demonstrated that PFDI-20, UDI-6, and PFIQ-7 scores were significantly higher among the older group after correction for BMI (BMI was defined as an ordinal independent variable): corrected p = 0.001, 0.005, and 0.005 respectively. The fact that correction for BMI had little effect on p-values corroborates previous studies. It is interesting to mention that BMI was not significantly correlated with age; however, it was significantly correlated with menopausal status. We cannot suggest that increase in BMI is the result of hormonal changes and not aging since we did not measure hormonal levels objectively.
Age was negatively correlated with sexual activity as shown by logistic regression analysis. However quality of sexual life (FSFI) was not significantly correlated with age. This could possibly mean that older women in our set of participants were less likely to be sexually active but those who were active had similar quality of sexual life.
Strengths of this study included the prospective nature of the recruitment of the participants from a community-dwelling population, with a special nulliparous history. The limitations to our study include small sample sizes for each category due to the limit in our institutional seed funding. Future larger sample size studies may assist to fortify our conclusions.
5. Conclusion
In conclusion; in this study of young nulliparous versus older post-menopausal women, despite not having pelvic organ prolapse, the older women had higher pelvic organ prolapse and urinary symptoms bother associated with higher Valsalva pressures.
Acknowledgements
This study was funded by an INOVA seed Grant.
Dr. Alshiek was funded by a research scholar grant from International Continence Society.
The authors received no assistance from any individuals or companies for preparation of this manuscript.
Dr. Jalalizadeh was a self-funded research scholar volunteer who performed the statistical analysis.
This paper was presented in 2018 ICS and 2018 AUGS summits.
Pelvic Floor Distress Inventory—Short Form 20
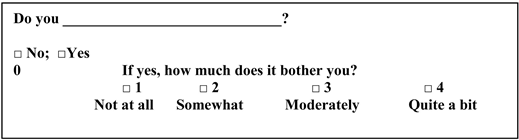
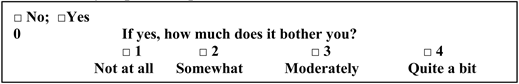
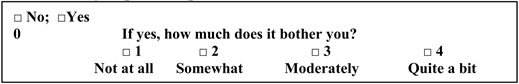
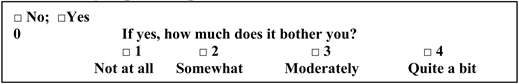
Instructions: Please answer all of the questions in the following survey. These questions will ask you if you have certain bowel, bladder, or pelvic symptoms and, if you do, how much they bother you Answer these by putting an X in the appropriate box or boxes. While answering these questions, please consider your symptoms over the last 3 months.
All items use the following format with a response scale from 0 to 4.
Pelvic Organ Prolapse Distress Inventory 6 (POPDI-6)
1) Usually experience pressure in the lower abdomen?
2) Usually experience heaviness or dullness in the pelvic area?
3) Usually have a bulge or something falling out that you can see or feel in your vaginal area?
4) Ever have to push on the vagina or around the rectum to have or complete a bowel movement?
5) Usually experience a feeling of incomplete bladder emptying?
6) Ever have to push up on a bulge in the vaginal area with your fingers to start or complete urination?
How long have you had the above symptoms? _______ months, ______ years
What has made these symptoms better: _______________________________
What has made these symptoms worse: _______________________________
Colorectal-Anal Distress Inventory 8 (CRADI-8):
Frequency of stool: _______ per day _______ per week _______ per month
Laxatives? Suppositories? Enemas?
7) Feel you need to (circle one or more):
strain too hard to have a bowel movement, press inside the vagina to have a bowel movement, press on the perineum to have a bowel movement, manually disimpact
8) Feel you have not completely emptied your bowels at the end of a bowel movement?
9) Usually lose stool beyond your control if your stool is well formed?
10) Usually lose stool beyond your control if your stool is loose?
11) Usually lose gas from the rectum beyond your control?
12) Usually have pain when you pass your stool?
13) Experience a strong sense of urgency and have to rush to the bathroom to have a bowel movement?
14) Does part of your bowel ever pass through the anus and bulge outside during or after a bowel movement?
![]()
How long have you had the above symptoms? _______ months, ______ years
What has made these symptoms better: _______________________________
What has made these symptoms worse: _______________________________
Urinary Distress Inventory 6 (UDI-6):
Frequency of urination: _______ per day _______ per night
FREQUENCY OF INCONTINENCE: ________ times/day or every _______ hours, up to pee ________ times/night
15) Usually experience frequent urination?
![]()
16) Usually experience urine leakage associated with a feeling of urgency, that is, a strong sensation associated with (Please circle one or more):
Running to bathroom, leakage before pulling pants down, running water, putting a key in a door, sexual intercourse
![]()
17) Usually experience urine leakage related to (Circle one or more) coughing, sneezing, laughing, standing up or walking?
![]()
18) Usually experience small amounts of urine leakage (that is, drops)?
![]()
19) Usually experience urinary (Circle one or more) hesitency, straining to void, poor flow, intermittent stream, post-micturation dribble, difficulty emptying your bladder
![]()
20) Usually experience pain or discomfort in the (Circle one or more) lower abdomen, genital region, bladder, urethra?
![]()
How long have you had the above symptoms? _______ months, ______ years
What has made these symptoms better: _______________________________
What has made these symptoms worse: _______________________________
PREVIOUS TREATMENT? NO YES: (Describe)
Detrol, Ditropan, Vesicare, Enablex, Sanctura Other:
Previous Bladder infections No Yes ________ in past year
Previous kidney infections No Yes
History of kidney stones or urinary bladder stones? No Yes
FOR OFFICE USE:
Scale scores: Obtain the mean value of all of the answered items within the corresponding scale (possible value 0 to 4) and then multiply by 25 to obtain the scale score (range 0 to 100). Missing items are dealt with by using the mean from answered items only.
PFDI – 20 Summary Score: Add the scores from the 3 scales together to obtain the summary score (range 0 to 300).
Pelvic Floor Impact Questionnaire—Short Form 7
Instructions: Some women find that bladder, bowel, or vaginal symptoms affect their activities, relationships, and feelings. For each question place an X in the response that best describes how much your activities, relationships, or feelings have been affected by your bladder, bowel, or vaginal symptoms or conditions over the last 3 months. Please make sure you mark an answer in all 3 columns for each question.
FOR OFFICE USE:
Scoring the PFIQ – 7:
All of the items use the following response scale:
0, Not at all; 1, somewhat; 2, moderately; 3, quite a bit
Scales:
Urinary Impact Questionnaire (UIQ-7): 7 items under column heading “Bladder or urine.”
Colorectal-Anal Impact Questionnaire (CRAIQ-7): 7 items under column heading “Bowel or rectum.”
Pelvic Organ Prolapse Impact Questionnaire (POPIQ-7): 7 items under column heading “Pelvis or vagina.”
Scale scores: Obtain the mean value for all of the answered items within the corresponding scale (possible value 0 to 3) and then multiply by (100/3) to obtain the scale score (range 0 to 100). Missing items are dealt with by using the mean from answered items only.
PFIQ-7 Summary Score: Add the scores from the 3 scales together to obtain the summary score (0 to 300).
Questions Related to Your Sexual Health and Function
In answering the following questions, the terms below apply:
Sexual activity includes caressing, foreplay, masturbation and vaginal intercourse
Sexual intercourse is defined as penile penetration (entry) of the vagina
Sexual stimulation includes situations like foreplay with a partner, self-stimulation (masturbation), oral stimulation, or sexual fantasy.
Sexual desire or interest is a feeling that includes wanting to have a sexual experience, feeling receptive to a partner’s sexual initiation, and thinking or fantasizing about having sex.
FSFI SCORING APPENDIX
Are you sexually active: Yes No
If yes,
Do you feel vaginal pain with superficial penetration, deep penetration, all the time.
Do you feel bladder pain with superficial penetration, deep penetration, all the time.
Please answer the following questions if you perceive that you need help with sexual functioning
FOR OFFICE USE:
The individual domain scores and full scale (overall) score of the FSFI can be derived from the computational formula outline in the table below. For individual domain scores, add the scores of the individual items that comprise the domain and multiply the sum by the domain factor (see below). Add the six domain scores to obtain the full scale score. It should be noted that within the individual domains, a domain score of zero indicates that the subject reported having no sexual activity during the past month. Subject scores can be entered in the right-hand column.