Development of a Six Sigma Infrastructure for Trabeculectomy Process ()
1. Introduction
Glaucoma is one of the leading causes of irreversible blindness throughout the world. World Health Organiza- tion (WHO) has stated that glaucoma accounts for blindness in 5.1 million people or 13.5% of the global blind- ness, i.e. behind cataracts and trachoma at 15.8 million and 5.9 million persons, or 41.8% and 15.5% of global blindness, respectively [1] . Glaucoma has become the second most common cause of bilateral blindness world- wide. In the US, it is the second leading cause of blindness and the most frequent cause of blindness (5.6%) among African-Americans, according to the US Department of Commerce’s Bureau of the Census 1990 pro- vided by the National Society to prevent blindness in 1993 [1] . Even though it is known to be more commonly afflicting older adults, it may occur in all segments of society with significant health and economic consequences, making it a major health problem [2] .
Trabeculectomy, the most commonly performed glaucoma filtering procedure, is performed when medical treatment or laser therapy or both fails to reduce IOP from a level that has been associated with progressive vis- ual filed loss or optic nerve damage. It is indicated when target intraocular pressure (IOP) is not achieved or when the neural tissue or visual function is progressively lost despite maximally tolerated medical or laser ther- apies. The filtering surgery is performed at the surgical limbus where the peripheral cornea meets the sclera ex- ternally. Ineffectiveness, intolerance, and poor compliance with medical therapy yield the decision for surgical intervention [3] .
Trabeculectomy is performed as an ambulatory procedure unless general medical care requires medical ad- mission [4] . The purpose of the treatment is to maintain visual function and prevent further loss. Although many factors may contribute to glaucomatous optic neuropathy, reduction of IOP remains the primary therapeutic goal. Medical treatment and laser or incisional surgery to lower IOP prevents additional visual field loss in most pa- tients with primary open-angle glaucoma [5] [6] .
Although glaucoma filtering surgery risks are usually limited to those of local anesthetics and ocular compli- cations, knowledge of general medical conditions such as diabetes, hypertension, cardiac status, and anticoagu- lant use, is important [4] .
Intraoperative complications may be related to anesthesia, corneal traction suture, conjunctiva and scleral flap [4] . Many postoperative complications such as hypotony and shallow anterior chamber also occur as a direct re- sult of poor surgical technique involving scleral flap dissection, inner block removal or conjunctival closure [4] . However, complications are not limited to the immediate postoperative period. Longterm changes in the bleb may predispose to leaks, blebitis and endophtalmitis [7] - [11] . To minimize complications and enhance surgical success, attention should be paid to each step of the procedure. Therefore, complications must be detected early in order to initiate adequate preventative and therapeutic measures.
Once the blindness of glaucoma has occurred, there is no known treatment that will restore the lost vision. In nearly all cases, however, blindness from glaucoma is preventable [12] . This prevention requires early detection and proper treatment. Detection depends on the ability to recognize the early clinical manifestations of the vari- ous glaucoma types [12] . Approporiate treatment requires an understanding of the pathogenic mechanisms in- volved, as well as a detailed knowledge of the drugs and operations that are used to control the IOP [12] . Thus, postoperative trabeculectomy care is as important as the procedure itself in determining the outcome. Anterior chamber depth, IOP level and bleb characteristics are important determinants of aqueous humor outflow through the fistula. Modulation of the postoperative inflammation and wound healing process may also affect the success [13] .
The use of Six Sigma, as a quality improvement method, can be employed in order to eliminate complications encountered during and after ophthalmic surgeries [14] . Originally initiated by Motorola, Honeywell and Gener- al Electric [15] , Six Sigma is a powerful performance improvement tool that is changing the face of modern healthcare delivery [16] . Although it was initially introduced in manufacturing processes, it is being imple- mented in diagnostic imaging processes [17] - [19] , emergency room [20] , paramedic backup [21] , laboratory [22] , cataract surgery [14] , radiology [23] , surgical site infections [24] , Intra Lase surgery [25] , LASIK surgery [26] , strabismus surgery [27] , intravitreal injections [28] , cataract surgery in patients with pseudoexfoliation syndrome [29] , pars plana vitrectomy [30] phacoemulsification cataract surgery [31] , and stent placement [32] as a cost-effective way to improve quality, performance and productivity.
A Six Sigma process produces 3.4 defective parts per million opportunities (DPMO) [33] . Being a method that eliminates errors, Six Sigma makes use of a structured methodology called DMAIC to find the main causes behind problems and to reach near perfect processes [34] . DMAIC is useful to analyse and modify complicated time-sensitive healthcare processes involving multiple specialists and treatment areas by identifying and remov- ing root causes of errors or complications and thus minimizing healthcare process variability [16] [33] .
In this study, a Six Sigma infrastructure was developed for a public eye care centre in order to reduce the number of complications and thus, improve the outcomes of their trabeculectomy surgeries. In addition, sigma level of each type of complication are calculated and reported.
2. Method: Application of Six Sigma’s DMAIC for Trabeculectomy Surgery
When the eye care centre decided that Six Sigma was the best way to achieve their goals, a surgical team was assembled and trained in the methodology. Committed and consistent leadership to overcome the complications was assured by this team. They firstly generated a SIPOC (Supplier, Input, Process, Output and Customer) Table for the process (Table 1). To achieve the performance objective, the surgical team first determined by brains- torming the CTQ factors, i.e. the factors that may have an influence on the objective.
The surgical team determined the metrics to measure existing process. The metrics to be chosen for a Six Sigma study were:
1) Total number of surgeries performed in the eye care centre,
2) Number of complications.
Data were collected for a period of ten years. In this period, surgeries were performed on 253 eyes. Complica- tions experienced (Table 2) had been noted as they occurred. The surgical team identified ten types of complica- tions and classified them as when (i.e. intraoperatively and/or postoperatively), and how soon they occur, i.e. acute, sub-acute and/or chronic (Table 4). Then, sources (Table 3) and root-causes (Table 4) of these complica- tions are tabulated by type.
![]()
Table 1. SIPOC table for trabeculectomy surgery.
![]()
Table 2. Complications experienced.
![]()
Table 4. Root-causes of complications.
3. Analysis
The surgical team analysed the occurrence frequency of each complication and related them with the root-causes. (Table 4 and Table 5). The analysis revealed that hyptony (Type III), shallow anterior chamber (Type IV) and hyphema (Type V) were the three most frequently occurring complications in the trabeculectomy surgeries (Ta- ble 5). Then, they classified the CTQs as “vital few factors” and “trivial many factors” according to how fre- quent they caused the complications. The “vital few” factors, i.e. the factors that had the most impact on the success of surgery were determined to be the patient’s eye anatomy and ophthalmic surgeon’s experience. The other factors, i.e. quality of the surgical equipment, quality and type of suture, and experience of staff were the “trivial many”.
![]()
Table 5. Frequencies, DPMOs and sigma levels.
To measure the current sigma level of a complication, surgical team calculated the current DPMO and sigma levels for each complication type (Table 5). For this, two distinct datasets are required: total number of trabecu- lectomy surgeries performed (A) and total number of complications occurred (B). Then, the DPMO can be cal- culated from Equation (1) as follows:
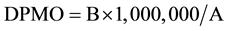 (1)
(1)
Normal distribution underlies Six Sigma’s statistical assumptions [14] . An empirically-based 1.5 sigma shift is introduced into the calculation. A higher sigma level indicates a lower rate of complications and a more efficient process [14] .
The highest sigma level was obtained for expulsive haemorrhage (Type II) and retinal detachment (Type XII). The lowest sigma level was found to belong to hypotony (Type III). Having sigma levels lower than 4.00; all types of complications except haemorrhage (Type II) and retinal detachment (Type XII) needed to be signifi- cantly reduced.
The process sigma level, calculated from the arithmetic average of sigma levels of twelve complications, was found to be 3.1391.
4. Discussion
Risk assessment of the surgery was achieved by the Failure Mode and Effect Analysis (FMEA). Utilization of the FMEA involved break down the process into individual steps: potential failure modes (i.e. complications), severity score, probability score, hazard score, criticality and detection, so that the surgery team could look at key drivers in the process based on the past experience.
Occurrence trends and consequences of complications over a 10-year period had been monitored and recorded. Surgical team prioritized the complications according to how serious their consequences were (i.e. severity score); how frequently they occurred (i.e. probability score) and how easily they could be detected. Hazard analysis was employed in order to identify failure modes and their causes and effects. The surgery team deter- mined the severity of each complication and assigned scores for them. The severity of each complication was scored from 1 to 4 (Table 6).
For each complication type, the hazard score was calculated by multiplying the severity score with the proba- bility score. Consequently, an FMEA table was drawn (Table 7). Among the complications, hypotony (Type III) yielded the highest hazard score. Haemorrhage (Type II) and retinal detachment (Type XII) were almost equally hazardous complications. According to FMEA, both were the least hazardous complications.
Corrective Action Plan
The surgical team developed preventive measures for each type of complication in order to bring the overall surgery process under control (See the Appendix). By brainstorming on the mechanisms underlying the compli- cations, they implemented the following corrective action plan to reduce and/or eliminate other complications.
5. Conclusions
In this study, authors found that twelve types of complications were encountered in the eye care centre while performing trabeculectomy surgeries. The analysis showed that these complications had occurred either intra- operatively or postoperatively. Postoperative complications were almost always related to the events that had occurred during the surgery. The process sigma level of the overall process (i.e. trabeculectomy surgeries per- formed in 10-years) was measured to be 3.1391.
It was found that patient’s eye anatomy and surgeon’s experience were the vital few CTQ factors that had the most impact on the success of surgeries. Many complications were related to the learning curve associated with the technique used in the procedure. These complication rates were reduced as surgeons gained experience and were trained on how to identify, minimize or eliminate the sources and root-causes of the complications. These lections of quality and type of suture are also essential. Staff should be trained to gain more experience on the surgery.
To conclude, the risks associated with trabeculectomy can be minimized by taking the necessary preventative measures with appropriate preoperative, intraoperative and postoperative care.
Appendix
NOTES
*Corresponding author.