Influencing factors on time of breastfeeding initiation among a national representative sample of women in India ()
1. INTRODUCTION
Breastfeeding has an important role in public health due to its numerous health benefits for children and mothers [1,2], for example, there is convincing evidence that breastfeeding has beneficial effects in the prevention of gastrointestinal infections, including diarrhoea [3-6], and otitis media [7,8]. Furthermore, studies have shown that it has proven beneficial for mothers in reducing risk of rheumatoid arthritis [9] as well as, to a certain extent, reducing risk of pre-menopausal breast cancer [10] and ovarian cancer [11-14].
It has been demonstrated that infants born in a particular ward where time of first suckling was earlier generated a higher incidence of breastfeeding [15]. Moreover, the first breast milk contains colostrum, which especially protects the infant against infections. A study carried out in Ghana demonstrated an increased risk of neonatal mortality if initiation of breastfeeding was delayed from 1 hour to day 7 [16]. The same study also showed that late initiation, defined as after day 1, was related with an increase of risk of neonatal death by 2.4 times [16]. Similar results were demonstrated in a study in Nepal, where a higher mortality was associated with later initiation of breastfeeding, defined as after 24 hours, compared to early initiation, defined as before 24 hours [17]. For this reason, WHO recommends breastfeeding to be initiated within 1 hour after giving birth [18]. Hence promoting and providing possibilities to initiate early breastfeeding is vital to reduce the risk of ill health for the infant. In India, according to statistics from International Baby Food Action Network (IBFAN), 24.5% mother initiated breastfeeding within 1 hour [19]. It is worthwhile to mention here that the neonatal mortality rate in India is 43 per 1000 live births, in comparison with for example Australia, which has 1 per 1000 live births [18].
Utilisation of health care, and particularly maternal health care, is vital for the health of mothers and infants [20,21]. It is important for pregnant women to receive antenatal care; the WHO recommends at least four visits or assessments of antenatal care [18]. Furthermore, it is highly encouraged that delivery occurs in a suitable and hygienic environment under the supervision of health professionals. As such, to reduce health risk of mothers and infants it is important that they receive sufficient care before, during and after delivery, including neonatal care such as breastfeeding. Unfortunately, there is a lack of utilisation of health care facilities in India [22]. Reasons for this vary but too far a distance to a facility, long waiting time and poor quality of healthcare are some of the reasons that have been found to impact upon this [23]. As such, availability of health care services for women giving birth is limited, especially for women living in rural areas, and may impact on possibilities of early initiation of breastfeeding.
Partner behaviours, such as controlling behaviour or violent behaviour, have several negative effects on women’s health behaviour such as contraceptive use, sanity, reproductive health issues and neonatal care [24,25]. Therefore, it may have a negative effect on breastfeeding initiation. There is a lack of studies focusing on controlling behaviour and the effect it may have on breastfeeding initiation. However, studies have shown that experience of abuse and violence affects breastfeeding [26-28]. For example, Lau and Chan [28] found that women who have not experienced violence from a partner during pregnancy were more likely to initiate breastfeeding compared to women who had experience of partner violence. Regrettably, prevalence of domestic violence or gender-based violence is quite high in India [29] and there is a fairly high social acceptance of gender-based violence [30]. It is therefore of importance to investigate what influence partner’s behaviour may have on breastfeeding initiation. Several studies have tried to explore influencing factors for the initiation of breastfeeding in different country contexts. In India, there is no such study using national representative samples.
As early initiation of breastfeeding is vital for the health of the child understanding barriers and reasons for not commencing early breastfeeding are important to increase our knowledge of these barriers and hence improve conditions and strategies to overcome these barriers. Early initiation of breastfeeding is also a contributing factor towards the achievement of the Millennium Development Goal of increased levels of child survival. WHO not only highlights the importance of increasing early initiation of breastfeeding but question why it has not received more attention [31]. Hence, the current study aims to examine factors influencing time of initiation of breastfeeding among women in India, using nationally representative samples. Health care utilisation related issues and partner behaviour were emphasized as predicting factors of breastfeeding initiation.
2. METHOD
Data from the Ministry of Health and Family Welfare of the Governments of India’s National Family Health Survey (NFHS) from 2005-2006 (NFHS-3) has been used in this study. A total of 124,385 women between the age of 15 - 49 from all 29 member states of India participated in the NFHS. In the present study a total of 35,795 female respondents are included. This is based on the number of women who reported that they had breastfed at least one child and represent 29% of the overall participating women in the NFHS.
2.1. NFHS Questionnaire
The questionnaire being used in the NFHS is focused upon information on health and family welfare issues. Data was collected via three different questionnaires, one for the household, one for women and one for men. It is the questionnaire for women that form the basis for the current study. The questionnaire for women contained details on background and demographics, reproductive history, family planning methods, fertility preferences, antenatal and delivery care, child care and nutrition, child and adult mortality, information regarding STDs, AIDS, marriage, sexual behaviour, empowerment and social indicators, domestic violence, use of health care. In regards of the present study, attention has been given to the sections on antenatal and delivery care, child care and nutrition and domestic violence.
2.2. NFHS Data Collection and Sampling
The data for the NFHS-3 was collected between December 2005 and August 2006. Sampling for the NFHS- 3 was based on the sampling design of probability proportional to size (PPS). The initial sample size was determined to comprise 1500 completed interviews in states with a population less than 5 million (based on the 2001 Census), 3000 completed interviews in states with 5 to 30 million and finally 4000 completed interviews in states with a population over 30 million. The only exception to this was in the largest state, Uttar Pradesh, where a fixed number of 10,000 completed interviews was determined. All of the completed interviews were with ever-married women (i.e. married at any time in their lives) between the age 15 and 49. In the rural areas, a two stage sample design was conducted where the first stage consisted of selecting Primary Sampling Units (PSUs), villages, using PPS and the second stage consisted of systematic selection of households within each PSU. In the urban areas a three-stage sample design was used instead due to larger wards. The first step consisted of selecting Primary Sampling Units (PSUs), municipal wards, using PPS, the second step involved random selection of census enumeration blocks (CEB) and finally the third stage consisted of randomly selecting households within each CEB. For more information on the details of the sampling design used in the NFHS-3 can be found in the final report of the NFHS-3 [32]. The NFHS- 3 fieldwork was conducted by 18 research organizations between December 2005 and August 2006.
2.3. Dependent Variables
Time of breastfeeding initiation was defined as when after birth the women commenced breastfeeding. Breastfeeding was initiated immediately (i.e. within one hour of the delivery) within 24 hours (i.e. after one hour to 24 hours) of the delivery or after 24 hours of the delivery. Breastfeeding for the latest child was included in the study.
2.4. Independent Variables
Demographic factors were defined as age, urban or rural residency, economic status, educational level, religion, caste or tribe. Age was categorized into seven groups (15 - 19, 20 - 24, 25 - 29, 30 - 34, 35 - 39, 40 - 44, 45 - 49; education was categorized into four groups (no education, primary, secondary, higher); religion was grouped into Hindu, Muslim, Christian and Others; and economic status was measured as the quintiles of all household economic assets and grouped into poorest, poorer, middle, richer and richest [23]. In India there are difference racial and ethnic minorities. Some of these groups are classified into scheduled caste, scheduled tribe, and other backward class (OBC) by the Indian Government as they are socially and economically disadvantaged. Belonging to one of these three categories grants the opportunity of positive discrimination in areas of education and employment [33].
Health care utilisation factors included place of delivery, pre-natal visit and delivery assistance. Place of delivery included home delivery, public hospital and private hospital delivery. Pre-natal visits of the respondents were categorized into three groups: 1) visit to doctor; 2) visit to nurse/midwife/auxiliary nurse midwife (ANM)/ lady health visitor (LHV); and 3) visit to trained birth attendants (TBA)/health persons (IIPS, 2007). Assistance during delivery was provided by 1) doctor; 2) nurse/ midwife/auxiliary nurse midwife (ANM)/lady health visitor (LHV); 3) trained birth attendants (TBA)/health persons; and 4) by the relatives or friends. These variables had yes/no answering options.
Husband’s/partner’s controlling behaviour was measured by six variables: Husband jealous if talking with other men; Husband accuses her of unfaithfulness; Does not permit her to meet her girlfriends; Husband tries to limit her contact with family; Husband insists on knowing where she is; and Husband doesn’t trust her with money. Violence against women was measured by whether respondent had experienced (during conjugal life) any emotional, physical and sexual violence by the husband/partner. These variables had yes/no answering options.
2.5. Statistical Analyses
The proportions and Chi-square tests were performed to explore the cross-relationships between dependent and independent variables. Dependent variables were breastfeeding initiation immediately, within 24 hours and after 24 hours. Independent variables were demographic factors, healthcare utilisation and husband’s controlling and violent behaviour. Multivariate logistic regressions were calculated to study the potential association between time of initiation of breastfeeding and subjects’ demographic status, healthcare utilisation and husband’s controlling behaviour and violence behaviour. Data were analysed using IBM SPSS. Two separate multivariate logistic regression analyses were run for two dependent variables: breastfeeding initiation within one hour (immediately) or not and within 24 hours or not. A significant level at p < 0.05 was employed in the analyses.
2.6. Ethical Issues
Informed consent was obtained from the participants prior to starting the survey, and the right to withdraw was emphasized throughout the survey. Ethical approval for the survey was obtained from the Institutional Review Board of Opinion Research Corporation (ORC), Macro International Incorporated, who was the main technical support provider for the whole survey.
3. RESULTS
Of the total amount of women participating in the study (n = 35,795), 39% of them lived in urban areas and 61% in rural areas. The level of education differed between the responding women with 38% of all women having no education, 14% having primary education, 39% secondary education and only 9% higher education. A majority of women were Hindu (74%) and the remaining women were either Muslim (13%) or belonging to other religion (13%). Most women either belonged to other backward class (34%) or general (32%), a minority of the women belonged to a scheduled caste (18%) or scheduled tribe (16%). Among all 35,795 women in the study, a total of 31.1% initiated breastfeeding within one hour and 68.6% initiated breastfeeding within first week.
3.1. Demographics
As seen in Table 1, women belonging to age groups 35 - 39 and 45 - 49 reported highest percentage of initiation of breastfeeding within one hour, 32.5% respectively 32.7%. The youngest women, belonging to age group 15 - 19, reported lowest percentage of initiation of breastfeeding within the first hour, 25.3%.
Of women belonging to a scheduled tribe 44.8% reported initiation of breastfeeding within one hour compared scheduled caste 26.8%, OBC 25.8% and finally general 31.6%. Regarding breastfeeding initiation after 24 hours 41.8% of women in the scheduled caste reported doing so and 42.7% of women belonging to OBC compared to 32.5% of general women and 22.9% of women belonging to a scheduled tribe. Scheduled caste women were less likely to initiate breastfeeding within one hour (OR = 0.86, CI = 0.77 - 0.96) as well as within 24 hours (OR = 0.86, CI = 0.77 - 0.96) compared to general. Same goes for other backward class, results showed that the women belonging to this class were less likely to initiate breastfeeding within one hour (OR = 0.77, CI = 0.71 - 0.84) and within 24 hours (OR = 0.79, CI = 0.72 - 0.87) than women belonging to general. Furthermore, women belonging to a scheduled tribe were 1.57 times more likely to initiate breastfeeding within the first hour and almost twice as likely (OR = 1.82, CI = 1.61 - 2.06) to initiate breastfeeding within 24 hours compared to general (Table 1).
In regard of educational level, 22.7% of women with no education initiated breastfeeding within one hour, 29.1% within 24 hours and 48.1% after 24 hours. Of women with primary education 33.2% initiated breastfeeding within one hour, 33.5% within 24 hours and 33.3% after 24 hours. Of women with secondary education 37.9% started breastfeeding within one hour, 35.9% within 24 hours and 26.2% after 24 hours. Of all women with higher education 37.1% of them stated initiation of breastfeeding within one hour, 37.2% within 24 hours and 25.7% after 24 hours. Women without education were less likely to initiate breastfeeding within one hour (OR = 0.54, CI = 0.45 - 0.64) and within 24 hours (OR = 0.58, CI = 0.48 - 0.71) compared to women with higher education. Difference was also noted between primary educational level and higher educational level, where women with primary education were less likely (OR = 0.73, CI = 0.60 - 0.87) to initiate breastfeeding within one hour, no significant results were obtained for initiation within 24 hours.
The results demonstrated that 22.8% of the poorest women initiated breastfeeding within one hour and 29% initiated within 24 hours and 48.2% initiated after 24 hours. The richest women however initiated breastfeeding within one hour more often (34.2%) and 37.5% after 24 hours and 28.3% after 24 hours. Poorest women were less likely to initiate early breastfeeding compared to richest women. However, women belonging to the second lowest wealth index (poorer) were more likely to initiated breastfeeding within one hour (OR = 1.25, CI = 1.07 - 1.45) compared to the richest women. Same results can be seen for middle income women, women in this category were even more likely to initiate breastfeeding within the first hour (OR = 1.35, CI = 1.18 - 1.54) compared to the richest women.
There were differences in time of breastfeeding depending on how many children the women ever gave birth to. Compared to four children or more, women with three children or less were more likely to initiate breastfeeding early. Women with only one child were most likely to initiate breastfeeding within one hour (OR = 1.24, CI = 1.12 - 1.36) as well as within 24 hours (OR = 1.38, CI = 1.24 - 1.52) compared to women with four children or more. More women living in urban areas started breastfeeding within one hour (33.3%) than women living in rural areas (30.1%). Urban women were less likely to initiate breastfeeding both within one hour (OR = 0.85, CI = 0.78 - 0.93) and within 24 hours (OR = 0.84, CI = 0.76 - 0.91) compared to rural women.
3.2. Health Care Utilisation Related Issues
More women who delivered their child in a public hospital initiated breastfeeding within one hour (41%) than women delivering in private hospital (32.5%) and home delivery (26.2%). Similarly, less women who delivered their child in a public hospital initiated breastfeeding after 24 hours (19.7%) than delivery in a private hospital (31.5%) and home delivery (45%). These results were also demonstrated with multiple regression where women who gave birth in a private hospital were less likely to initiate breastfeeding compared to public hospital as well as at home. The results demonstrated that women who gave birth in a private hospital were 0.67 (CI = 0.57 - 0.79) times less likely to initiate breastfeeding compared to when giving birth at home. Furthermore, the likelihood of initiating breastfeeding within 24 hours increased (OR = 1.63, CI = 1.39 - 1.92) when giving birth in a public hospital compared to at home (Table 2).
When it comes to prenatal visits, 36.6% of women who visited a doctor before birth started breastfeeding
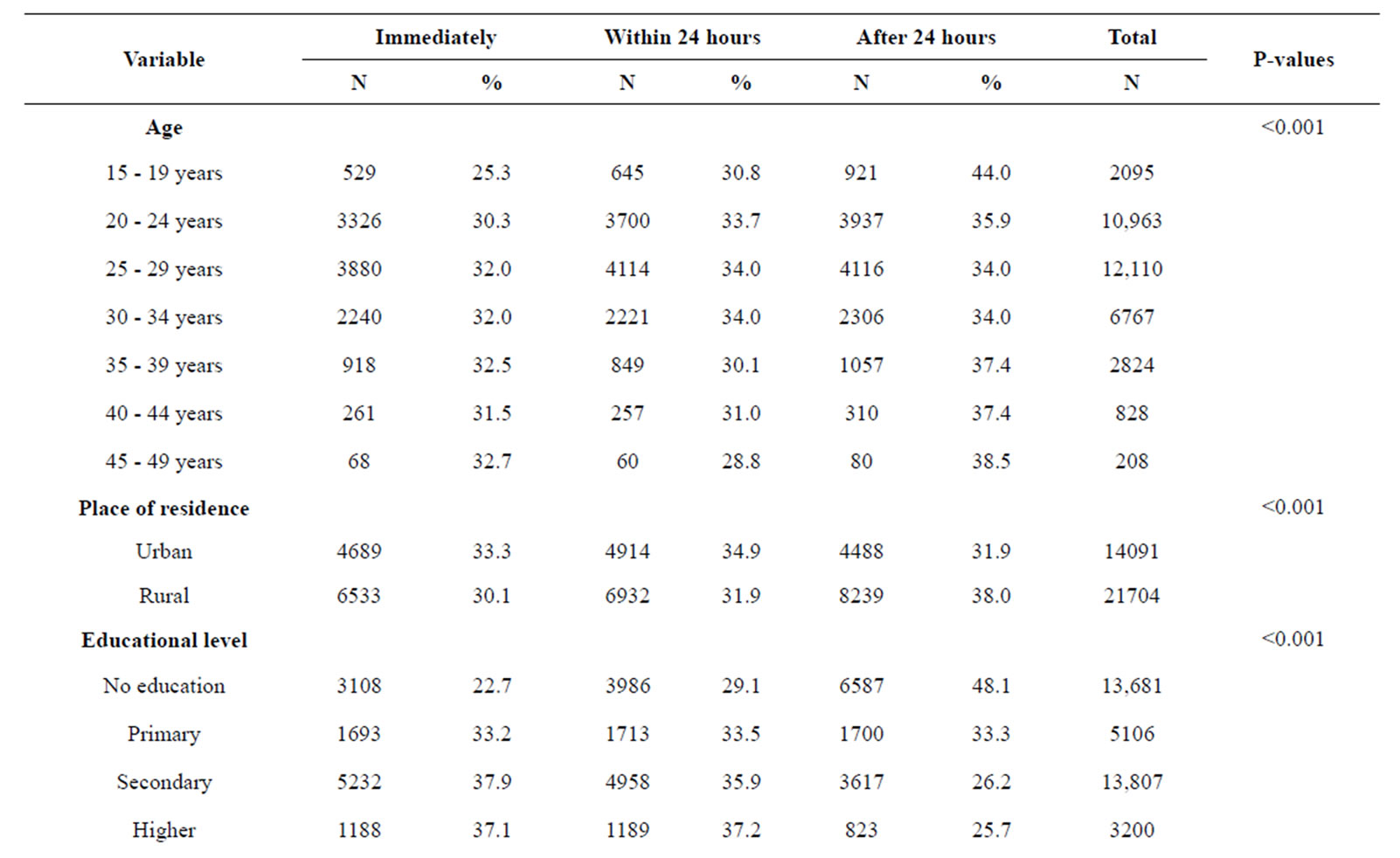
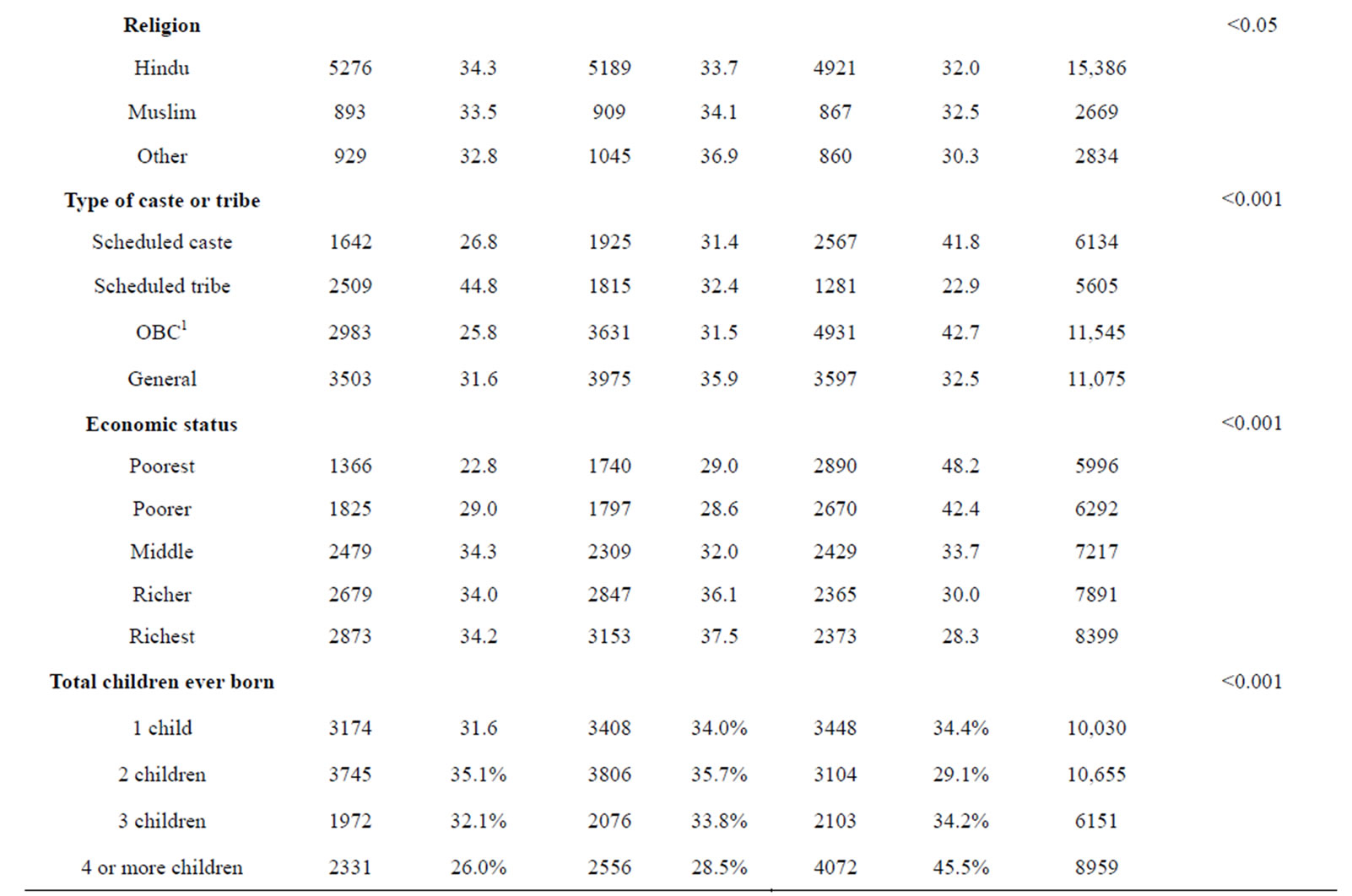
Table 1. Respondent’s demographics and their time of breastfeeding initiation.
1OBC = Other backward class.
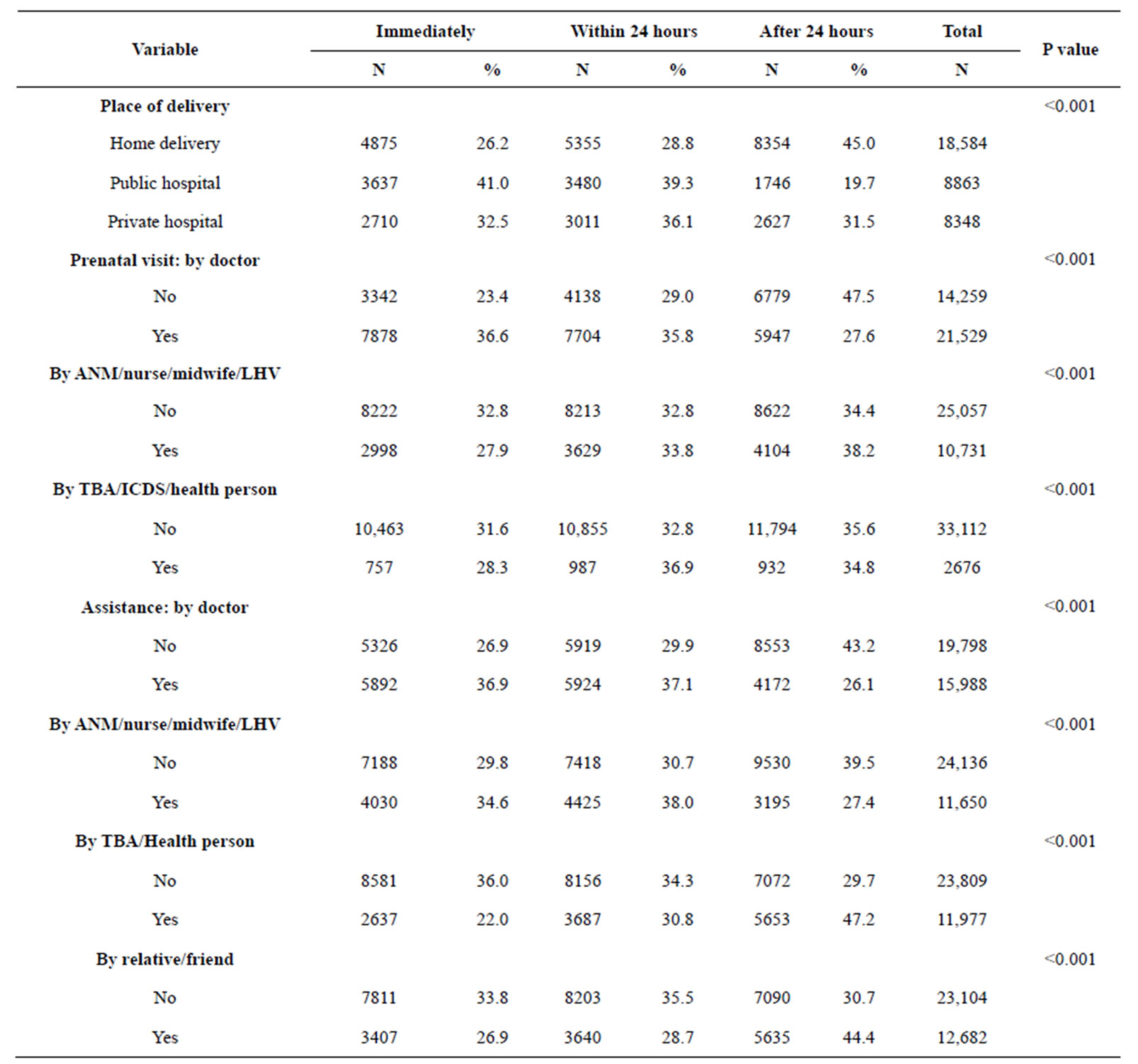
Table 2. Health care related issues and time of breastfeeding initiation.
ANM = Auxiliary nurse midwife; LHV = lady health visitor; TBA = Traditional Birth Attendant.
within one hour compared to 23.4% who did not visit a doctor. Of the women who did not see a doctor before birth 47.5% of them initiated breastfeeding after 24 hours. The findings of the multiple regression showed that women who had prenatal assessment by a doctor were 1.4 (CI = 1.27 - 1.54) times more likely to initiate breastfeeding within one hour as well as within 24 hours (OR = 1.40, CI = 1.27 - 1.54) compared to women not seeing a doctor. However, women who received a prenatal assessment by another health professional than a doctor, such as traditional birth attendant or personnel related to the integrated child development services, were only more likely to initiate breastfeeding within 24 hours (OR = 1.27, CI = 1.11 - 1.45) compared to women who did not receive this assessment. Furthermore, the findings demonstrated a difference between types of assistance during delivery. Women who received assistance by a nurse or midwife were less likely to initiate breastfeeding compared to women who did not get this assistance. Similar results were demonstrated for assistance by relative or a friend. Also, assistance during delivery of other personnel, such as traditional birth attendant or personnel related to the integrated child development services, were women who received such assistance were 0.57 (CI = 0.51 - 0.63) times less likely to initiate breastfeeding within one hour and 0.67 (CI = 0.61 - 0.75) times less likely within 24 hours compared to women who did not receive that assistance.
3.3. Husband’s Controlling and Violent Behavior
Of women reporting that their husband tries to limit their contact with the family 25.3% initiating breastfeeding within one hour compared to 32.8% of women who reported no such limitations from husband. Of women experiencing sexual violence, 24.9% initiating breastfeeding within one hour compared to 32.9% of women who did not report sexual violence (Table 3).
Women who reported their husband does not trust them with money, 27.4% of them initiated breastfeeding within one hour compared to 33.1% of women who did not report such matter. It was demonstrated with multiple regression that woman who had husband that did trust her with money was more likely to initiate breastfeeding within one hour (OR = 1.28, CI = 1.14 - 1.44) compared to woman whose husband did not trust her with money. Similarly, women who had husbands that did get jealous when they talked with other men were more likely to initiate breastfeeding within both 1 hour (OR = 1.21, CI = 1.10 - 1.34) and 24 hours (OR = 1.29, CI = 1.17 - 1.41).
Table 4 describes adjusted odds ratios (ORs), confi-