Combining a Low-Cost Bio-Simulator and Single Use or Disposable Bronchoscope: A Platform for Remote Training ()
1. Introduction
As a result of the COVID (Corona Virus Disease)-19 pandemic, interest in simulation including remote simulation learning and telemedicine has increased.
In 2014, the American Institute of Medicine (IOM) highlighted the need for a transition from experience based training without outcome and safety assessment to proficiency based training as the main target of development of undergraduate and graduate medical training [1]. Thereafter, the American College of Chest Physicians (ACCP) released a statement on the current state of bronchoscopy with suggestions for the future. The first recommendation was that professional societies should move from a volume-based system to skill acquisition and knowledge based competency assessment for pulmonary trainees [2]. They suggested that simulation should be integrated into a structured bronchoscopy teaching curriculum.
Simulators range from low fidelity devices similar to mannequins used in cardio-pulmonary resuscitation training to high fidelity simulators similar to flight simulators used in pilot training. Neither is without cost and the ACCP suggest that high fidelity simulators should be offered in regional simulator centres which should be accessible to all training bodies [2]. However, access to simulators should be available daily for trainees and this is not typically feasible beyond larger academic centres or cities. Traditional bio-simulators using porcine lungs are usually prohibited in hospitals and prevent on-site training [3]. The era of 3D printing allows the manufacture of silicone models printed from airways segmented from high resolution CT scans, but again access to this technology is limited in the western world, not to mention third world countries [4].
Healthcare providers have adapted learning and teaching methods and the use of remote learning is becoming common [5]. Technology has assisted in making remote simulation and tele-simulation accessible.
The COVID-19 pandemic has limited further opportunities for training with a reduction in access to endoscopy units for trainees and reduced elective procedures [6] [7] [8]. However, the COVID-19 pandemic has also lead to the rapid introduction of single use flexible bronchoscopes (SUFB) to many hospitals with endorsement by national and international bodies [6] [9]. SUFBs provides institutions the opportunity to purchase cheap bronchoscopes for training which can be stored in our pulmonary fellows office, which is where a simulator needs to be set up for optimal training [8] [9].
The lack of availability of a cheap bio-simulator lead to our group developing ALFIETM, an Airway Low Fidelity including Endobronchial Ultrasound (EBUS) bio-simulator made from predominately recyclable materials found in any household or hardware store.
We therefore designed a protocol to test whether a combination of ALFIETM and SUFB would differentiate novices (residents) from trainees with more experience in bronchoscopy (fellows) using a modified validated bronchoscopy Skills and Tasks Assessment Tool (BSTAT) (see Supplementary Material FigureS1) [10] [11] and whether training on ALFIETM-SUFB would improve performance.
![]()
Figure 1. ALFIETM-SUFB simulation. (a) Single use Broncoflex® Vortex (2.8 mm channel) scope. (b) ALFIETM contents. Testing strawberry as pseudo-peri-bronchial node including recyclable toilet rolls which allow movement of airway with pressure on inside wall, universal waste pipe with 90-degree angle mimicking oropharynx angle, pipe insulating lagging with pliability mimicking airway, recyclable coffee cup holder allowing movement and pliability and recycled outer plastic box. (c) Trainee performing endobronchial biopsy using children’s modelling compound (Play Doh®) as a pseudo endobronchial tumour.
2. Methodology
2.1. Statement of Ethics
With informed consent (including to take and publish videos and photos) and institutional board ethical approval (UCC-ECM 4 (e) 2021), trainees were invited to attend bronchoscopy simulation on ALFIE bio-simulator.
2.2. Study Design
2.2.1. Scopes
A single use Broncoflex® Vortex (2.8 mm channel) scope was used (Figure 1(a)). Standard Boston Scientific® brush and biopsy forceps were used for sampling.
2.2.2. ALFIETM Bio-Simulator Construction
ALFIETM was created using common house-hold products and products available in a local hard-ware store (Figure 1(b)). The use of recycled or recyclable materials was a primary objective.
Materials used included:
1) A recycled plastic box with a hole drilled on side.
2) A standard 90-degree drainage pipe.
3) Pipe lagging.
4) Recycled toilet rolls.
5) Recycled coffee cup holder.
Various organic materials were tested as a pseudo-tumour as well as children’s’ modelling compound (Play Doh®). For biopsy and brushing, Play-Doh® or the inside of an orange peel provided low simple low-cost options.
2.2.3. ALFIETM Simulation Training and B-STAT Testing (Video 1 and 2)
A modified B-TAT tool was used (Supplementary Material FigureS1) including a 9-point score for posture, hand position and equipment safety, a 5-point score for centring scope in midline, a 5-point score for avoiding airway trauma (judged by scraping the scope across the inside surface of the bio-simulator), and 5 points each for pseudo-tumour biopsy and brushing (Figure1(c)) [11] [12]. Thus, a total score out of 29 was calculated (Supplementary Material FigureS1).
Two faculty carried out modified B-STAT tests. Faculty were blinded to pre-training scores when scoring modified B-STAT test post training. Trainees were tested individually before and after training on ALFIETM.
Training consisted of 30 minutes of hands-on training using SUFB with ALFIETM bio-simulator.
This included a display of proper scope handling, a detailed description of the scope handle and functions, a display of body position when entering the distal airway beyond carina and how to perform endobronchial biopsy and techniques for transbronchial needle sampling using online video tools (https://www.bronchoscopy.org).
Average and standard deviation scores were calculated. Unpaired student t-test was used to compare continuous data in a normal distribution with two-tailed p values established.
Other data collected including year of training, bronchoscopy experience and courses attended.
3. Results
18 consecutive trainees were enrolled (Figure 2) including 14 residents (no prior scope experience or bronchoscopy course and 4 Fellows (1 - 4 years respiratory training with 2/4 having attended international bronchoscopy training courses).
3.1. Residents
Residents showed a statistically significant improvement in modified B-STAT
![]()
Figure 2. Vertical chevron diagram depicting B-STAT testing points and ALFIETM training.
![]()
Figure 3. Modified B-STAT Scores pre- and post-ALFIETM training for residents (n = 14), fellows (n = 4) and total group (n = 18). Average scores and 95% confidence intervals for standard deviation are depicted.
after training (p = 0.0001 (95% confidence intervals (CI) 4.73 - 10.27)) (Figure 3). All 14/14 residents improved with training (Videos 1-2, Supplemental Materials).
3.2. Fellows
Although all 4 fellows improved with training, the results were not significant (p = 0.0638 (95% CI-6.67 - 13.17) (Figure 3).
3.3. Overall Group
There was a significant improvement in modified B-STAT score after training in the total group (p = 0.0001 (95% CI 5.37 - 8.62) (Figure 3).
3.4. Comparing Residents and Fellows
Fellows outperformed residents in scope handling before training ((p = 0.0025 (95% CI 13.12 - 12.17) and after training on ALFIETM bio-simulator ((p = 0.0144 (95% CI 1.18 - 9.24) (Figure 3).
4. Discussion
The impact of COVID-19 pandemic on training should not be underestimated [8]. In our institution trainees were not allowed enter the endoscopy unit to reduce foot fall, reduce risk of COVID-19 to trainee, reduce procedure times and use of personal protective equipment (PPE). Traditional training of bronchoscopy in the endoscopy unit is associated with increased procedure time and complications [13]. Therefore, competency based training including simulators is recommended as a core component for training [1]. Although lacking the opportunity for anatomical learning, low fidelity simulators using actual bronchoscopes and biopsy tools is the perfect safe environment for teaching scope handling and biopsy technique. Indeed, pseudo-anatomical training is feasible with ALFIETM bio-simulator based on standard airway anatomy, branching and reducing the diameter of pipe lagging used. The development of low cost simulators is not novel however a simulator made of recyclable materials or materials found in a hardware store providing the opportunity for EBUS-TBNA and transbronchial biopsy and needle aspiration to our knowledge is [14] [15] [16]. It is also feasible to 3D print a mould based on CT segmentation of airway anatomy [17] and use this to build anatomically correct model using pipe lagging. High fidelity simulators provide proper anatomical training however high-fidelity simulators in bronchoscopy are hindered by lack of proper haptic feedback as they do not use real scopes and biopsy instruments used in the endoscopy unit. Low fidelity simulators in general trade anatomical training with the use of real instruments allowing proper device and tactile training. ALFIETM-SUFB is no different. Airway mimics can include progressive reduction in size of pipe lagging. We found that our model created “improper” anatomy possibly reflecting a post-surgical airway did not hamper technical training but may actually improve skills. Thus, in our opinion, our model posed enough challenge to identify the trainees’ skills in scope manoeuvre. That is, a pristine airway without any obstacle may lead to less opportunities for scope handling teaching. Low fidelity simulators have the advantage of permitting positioning at the point of training in the fellow’s office or endoscopy unit and thus allowing trouble shooting of real bronchoscopic situations.
Training thus far with ALFIETM bio-simulator has included bronchoscopic biopsy, brushing, TBNA and cryobiopsy (we find the inside of an orange peel excellent for biopsy). Meat can also be used as can playdough which allow cautery in an iteration made solely from solid plastic piping. Foreign body retrieval can also be demonstrated. Standard intubation mannequin heads can be added to further model the upper airway allowing rigid bronchoscopy training.
In parallel with an exponential growth in the clinical use of SUFBs [9], they provide a cheap and mobile platform for bronchoscopic training. Prior to the COVID-19 pandemic, there was gathering evidence that if patient ready reusable bronchoscopes were examined properly, most will harbour human DNA and protein and in one study over half harboured disease causing infection [18]. In parallel, there is a global drive to switch from reusable to single use devices and endoscopy related infections have been identified as a high risk procedure for patients [19] [20]. Scope related infection occurs as a result of bronchoscopy in at least 2.5% of all procedures [21]. The possibility of spreading COVID-19 related to reusable bronchoscopes to both staff and patients has also been raised [22]. SUFBs have the advantage of sterility, mobility, ease of use, no requirement for cleaning staff and are ideal for training and research [9].
To date, commercially available SUFBs have modified copyrighted cable heads for attachment to proprietary screens. Companies state that this is required by health regulation authorities due to a requirement for sterilising equipment. Making an SUFB available with an adaptor for a standard High-Definition Multimedia Interface (HDMI) port or a standard HDMI head would allow the use of SUFBs in a remote home training kit. However, the problem with availability of such connectivity is the possibility of not using the appropriate approved monitor for clinical use which clearly has sterility and quality issues.
In our study, ALFIETM-SUFB combination differentiated novices from those with more experience and training on ALFIETM-SUFB was associated with a significant improvement in performance on a modified BSTAT assessment. Although not significant probably due to low numbers, all fellows showed improvement after training. It was also our observation that this training provided valuable interaction between our department and residents who enjoyed training and received feedback on their procedural skills.
Training on low fidelity simulators is in line with recommendations for simulation training from ACCP and IOM [1] [2]. Not every trainee learns bronchoscopy at the same rate as demonstrated by CUSUM analysis [23] and low fidelity simulators such as ALFIETM bio-simulator allows repeated training and thus sustained proficiency. Across all skill sets, simulation-based training in bronchoscopy has been shown to be more efficient than traditional apprenticeship models [24]. However, simulation alone is not enough to make a trainee proficient in bronchoscopy. Simulation standards have been published detailing proper planning for simulation training [25]. Certification in bronchoscopy skills such as endobronchial ultrasound guided transbronchial needle aspiration (EBUS-TBNA) or other skills requires a comprehensive program including theory, simulation and clinical training and supervised training in the trainees own institution. A limitation which our study shares with most simulation research in medical procedures is that our outcome of improved performance on simulator does not demonstrate the impact of training on patient care [26]. The European Respiratory Society has developed such a program for EBUS-TBNA and simulation training which is based on a validated score with metrics followed by videos of trainees performance in actual clinical cases allowing the setting of a pass-fail mark [25]. Mastery learning is now endorsed by leading societies and is likely to become a gold standard for procedure training [26].
Limitations to our study also include smaller numbers of trainees tested, however even this small cohort was associated with significant improvements in scope performance. We used modified BSTAT tool which has not been properly validated with ALFIETM bio-simulator, however this tool differentiated novices from trainees with more expertise. Repeat testing would improve validity. Thus, the training received was in such a feasibility study and is in no way a replacement of standardised training such as the ERS certification. Reliability estimates for the data derived from B-STAT pre and post-test would also improve validity.
As stated already 3D-printed airways are an option but not to every bronchoscopy program globally. Our current model did not include upper airway anatomy simulation, which also is a disadvantage of some high-fidelity simulators, however standard intubation manakin heads can be added. Another limitation is not using multi-centre testing and this will be considered in future evaluation. A novice/intermediate/expert group may be a better test of discrimination and will be considered in future testing. We included a mix of first year and senior fellows in the more experienced group. The number of fellows per hospital in Ireland is far less than in many other countries and a multi-centre study was not feasible due to the requirement of reducing foot-fall between hospitals during COVID-19 pandemic. The COVID-19 pandemic limited access to faculty for assessment. Our 30 minute training may also have been too brief, a follow-up assessment would also evaluate for learning decay. However, in our country residents and fellows rotate between cities and COVID restrictions, isolation and infection made it too difficult to re-train and test the study population. The ERS formal training protocol in EBUS-TBNA provides an excellent framework for retraining and assessment [25].
5. Conclusion
In conclusion, we have designed a low-cost bio-simulator which can be used for bronchoscopy training using predominately recyclable materials and an SUFB scope. The combination of ALFIETM-SUFB provides a potential platform for remote training in bronchoscopy if SUFB companies make scopes with standard HDMI heads and connectivity.
Supplemental Materials
Video 1: Resident performing endobronchial biopsy sample using ALFIETM-SUFB.
Video 2: Endobronchial view of resident performing endobronchial biopsy of pseudo-tumour made from children’s’ modelling compound (Play Doh®).
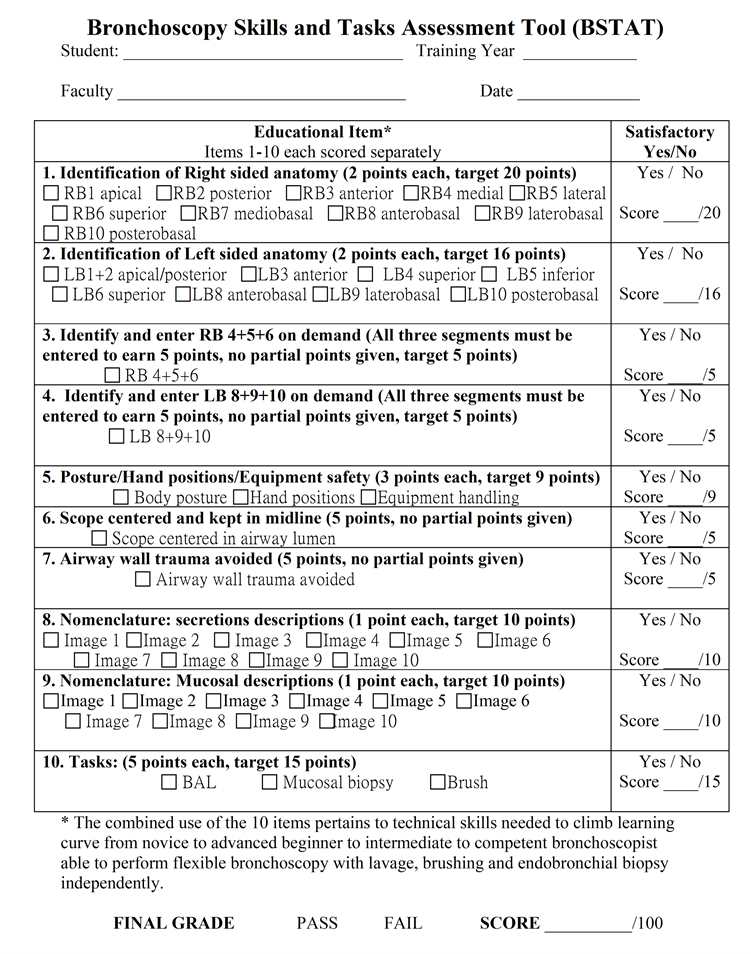
Supplementary Material FigureS1. B-STAT: Bronchoscopy Skills and Tasks Assessment Tool (13). Red box indicates questions used for 19-point assessment of posture, scope handling and airway trauma. Blue box indicates questions used for biopsy and brush assessment.
Reprinted with permission of the American Thoracic Society.
Copyright © 2021 Bronchoscopy.org. All rights reserved.