Evaluation of Length of Hospital Stay Joining Educational Programs for Type 2 Diabetes Mellitus Patients: Can We Control Medical Costs in Japan? ()
1. Introduction
The growing incidence of diabetes has become both a medical and financial concern in Japan. In fiscal year 2011, the medical costs for diabetes were estimated at 1215 billion yen or 3.1% of Japan’s total medical expenditure (38,585 billion yen) [1] . However, this concern is not limited to Japan. In fact, studies have reported that the number of diabetes patients worldwide has increased from 153 million in 1980 to 347 million in 2008 [2] . More recently, the American Diabetes Association [3] estimated the total cost of diagnosed diabetes in the United States at $245 billion in 2012, comprising $176 billion as direct medical costs and $69 billion from reduced productivity. In Australia, the proportion of individuals with diabetes increased from 1.5% of the total population in 1989-1990 to 4.1% in 2007-2008; diabetes accounted for 2% of total medical expenses and one out of every 25 cases requiring hospitalization in 2009-2010 [4] .
This study analyzes the length of stay (LOS) in Japanese hospitals for type 2 diabetes mellitus (hereafter, diabetic) patients who participated in educational programs (hereafter, educational hospitalization) to identify factors affecting their LOS. Type 2 diabetic patients represent more than 90% of diabetic patients in Japan. The diagnostic indicator is insufficient insulin resulting from reduced insulin secretion; however, the causes of the disease are still unknown [5] . Diabetes is the only disease that qualifies for educational hospitalization in Japan. Educational programs largely focus on lifestyle improvement guidance, such as improved diet and exercises, rather than medical treatment. Healy et al. [6] analyzed inpatient diabetes education (IDE) in an American hospital and concluded that “Formal IDE was independently associated with a lower frequency of all-cause hospital readmission within 30 days; this relationship was attenuated by 180 days.” LOS significantly influences medical costs associated with educational hospitalization. A problem currently faced in the Japanese medical system is the prolonged average length of stay (ALOS). In 2009 [7] , ALOS with diabetes as first-listed diagnosis was 5.0 days in the United States, whereas the present study reports that the ALOS of diabetes patients in Japan was 18.3 days.
Reducing ALOS can benefit the Japanese society in two ways. First is a reduction in the direct cost of hospitalization, given that nearly one-third type 2 diabetic patients participate in educational hospitalization programs in our dataset. Second is the indirect benefit of the prevention and good management of diabetes. Kudo et al. [8] reviewed 2,120,170 records of acute patients and found that 1) type 2 diabetes was observed in 11.4% patients, and 9.9% had diabetes as a comorbidity; 2) total LOS in a hospital for all diabetic patients was 33,468,152 bed days (i.e., 13.9% of total bed days); and 3) patients with type 2 diabetes as a comorbidity had prolonged LOS― the median LOS with and without diabetes was 9 and 13 days, respectively. Ncube-Zulu and Danckwerts [9] analyzed data for 407 patients with and without diabetes in South Africa and derived similar results―the average total hospitalization cost per patient was significantly higher and ALOS was longer for patients with diabetes than those without. Inoue et al. [10] also pointed out the risk of cancer in diabetic patients. In addition, various authors suggested that comorbid diabetes prolongs LOS and increases the risk of fatality due to hyperglycaemia [11] , chronic obstructive pulmonary disease [12] , foot disease [13] , fracture of the femur [14] , spinal surgery [15] , and cardiovascular diseases [16] . Hence, the true cost of diabetes is probably much higher than the direct one. Simply put, reducing LOS lowers costs incurred by diabetic patients and allows more patients to join educational programs aimed at helping patients prevent and control diabetes. This, in turn, could reduce the overall medical expenses in Japan.
However, not many studies have been conducted on the LOS of patients with diabetes in Japan. Although Mutou et al. [17] analyzed data for such patients under the age of 18, they did not use an econometric model. As mentioned, LOS accounts for a large portion of medical costs incurred during educational hospitalization. Thus, another major objective of this study is to evaluate whether hospitals influence patients’ LOS. If there are significant differences in ALOS among hospitals, ALOS can be reduced by improving educational programs in hospitals with prolonged ALOS. However, LOS may also depend on patients’ conditions. Hospitals with many patients requiring special care are likely to report prolonged ALOS. Therefore, it is necessary to control for patient characteristics using an econometric model. Sohmiya et al. [18] analyzed LOS by conducting a regression analysis on data for 313 patients, although their study was restricted to one hospital.
In April 2003, Japan introduced a new medical inclusive payment system based on the diagnosis procedure combination (DPC). The system is now called the DPC/per diem payment system (PDPS) [19] . As of April 2014, 1585 hospitals with a total of 492,206 beds were included in DPC/PDPS (hereafter, DPC hospitals) [20] . In June 2013, Japan reported a total of 7483 general hospitals with 897,749 beds [21] , of which DPC hospitals accounted for 21% and 55%, respectively. For details on DPC and DPC/PDPS, see Nawata et al. [22] . Presently, medical information on DPC hospitals is computerized, making it possible to use large-scale datasets. However, the effective use of these datasets has become an increasing concern [23] .
This study analyzed educational hospitalization LOS for diabetic patients using data for 991 patients from 28 Red Cross hospitals in 2008. To do so, we first adopted the Box-Cox [24] transformation model (hereafter, BC model). Next, drawing on previous studies, we tested the assumption that the maximum likelihood estimator (hereafter, BC MLE) under the normality assumption is a consistent estimator [25] -[28] , followed by an analysis of the LOS using the method confirmed by the tests. Finally, we analyzed hospital and regional factors that might affect LOS.
2. Box-Cox (BC) Model
2.1. BC Model and BC Maximum Likelihood Estimator
We used the BC model to analyze the LOS of diabetic patients:
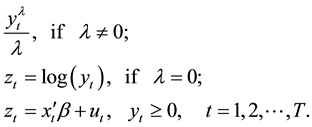 (1)
(1)
where  is LOS,
is LOS,  is the transformation parameter, and
is the transformation parameter, and  and
and  are the k-th dimensional vectors of the explanatory variables and coefficients, respectively. Let
are the k-th dimensional vectors of the explanatory variables and coefficients, respectively. Let  be the probability density function of the standard normal assumption. BC MLE is obtained by maximizing the likelihood function given by
be the probability density function of the standard normal assumption. BC MLE is obtained by maximizing the likelihood function given by
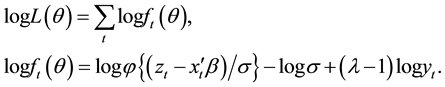 (2)
(2)
where  is the variance of
is the variance of  and
and . BC MLE is consistent and efficient if the error terms
. BC MLE is consistent and efficient if the error terms
are homoscedastic and the “small ” assumption [27] [29] is satisfied. Under these assumptions, the asymp-
” assumption [27] [29] is satisfied. Under these assumptions, the asymp-
totic distribution of BC MLE, 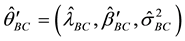 , is obtained by
, is obtained by
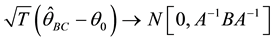 (3)
(3)
where  is the true parameter value of
is the true parameter value of ,
, 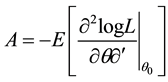 ,
, ![]() , and
, and![]() .
.
2.2. Testing the “Small σ” Assumption
We suppose that the error terms are homoscedastic. Nawata [25] considered the roots of the equations:
![]() (4)
(4)
![]() is obtained by approximating
is obtained by approximating![]() . If the first and third moments of
. If the first and third moments of ![]() are zero, the estimator obtained from Equation (4) (hereafter, the N-estimator) is consistent. Let
are zero, the estimator obtained from Equation (4) (hereafter, the N-estimator) is consistent. Let ![]() be the N-estimator. Its asymptotic distribution is given by
be the N-estimator. Its asymptotic distribution is given by
![]() (5)
(5)
where![]() ,
, ![]() , and
, and![]() ,
,
Since ![]() under the small
under the small ![]() assumption,
assumption, ![]() and thus,
and thus,
![]() (6)
(6)
where ![]() is the (1, 1) element of
is the (1, 1) element of![]() . We apply the Hausman test [30] to verify the small
. We apply the Hausman test [30] to verify the small ![]() assumption by using
assumption by using ![]() as the test statistic, where
as the test statistic, where ![]() is the estimator of
is the estimator of ![]() [27] . Note that no element of
[27] . Note that no element of ![]() can be used in the Hausman test [31] .
can be used in the Hausman test [31] .
2.3. Testing the Assumption of Homoscedasticity
BC MLE and the N-estimator would not be consistent under heteroscedasticity even if the small ![]() assumption were satisfied; therefore, it is also necessary to test the assumption of homoscedasticity as well. Nawata [26] [28] proposed an estimator that is consistent even under heteroscedasticity if
assumption were satisfied; therefore, it is also necessary to test the assumption of homoscedasticity as well. Nawata [26] [28] proposed an estimator that is consistent even under heteroscedasticity if ![]() and
and![]() . The estimator is obtained by the roots of the equations:
. The estimator is obtained by the roots of the equations:
![]() (7)
(7)
where![]() . The estimator obtained from Equation (7) (hereafter, robust estimator) is consistent even under heteroscedasticity. The asymptotic distribution of the robust estimator,
. The estimator obtained from Equation (7) (hereafter, robust estimator) is consistent even under heteroscedasticity. The asymptotic distribution of the robust estimator, ![]() , is given by
, is given by
![]() , (8)
, (8)
where![]() ,
, ![]() ,
, ![]() ,
,![]() , and
, and![]() .
.
Therefore, the second test can be conducted as follows [32] :
1) If the small ![]() assumption is accepted, BC MLE and the robust estimator are compared. Under the assumption of homoscedsticity,
assumption is accepted, BC MLE and the robust estimator are compared. Under the assumption of homoscedsticity,
![]() , (9)
, (9)
where![]() ,
, ![]() and
and ![]() are the first rows of
are the first rows of![]() ,
, ![]() and
and![]() , respectively, and
, respectively, and![]() .
.
BC MLE is used if the assumption of homoscedasticity is accepted, and robust estimator otherwise.
2) If the small ![]() assumption is rejected, the N-estimator and the robust estimator are compared. The
assumption is rejected, the N-estimator and the robust estimator are compared. The
asymptotic distribution of ![]() is given by
is given by
![]()
![]() , (10)
, (10)
where![]() . The N-estimator is used if the assumption of homoscedasticity is accepted, and
. The N-estimator is used if the assumption of homoscedasticity is accepted, and
the robust estimator otherwise. Unlike the previous test, estimating the variances in Equations (9) and (10) is often difficult. However, since
![]() , (11)
, (11)
we can perform the second test without the rather complicated calculation of matrices.
3. Evaluation of Educational Hospitalization LOS
3.1. Data
In this section, we analyze LOS for educational hospitalization of type 2 diabetic patients. The DPC code for these patients was 100070xxxxxx0x. In the case of diabetes mellitus, two DPC codes were assigned, 100070xxxxxx0x and 100070xxxxxx1x. Periods I and II and the specific hospitalization period were defined by DPC/PDPS as 8, 16, and 29 days, respectively. Medical payments in Japan are measured by points, and hospitals receive a payment of 10 yen per point. The per diem inclusive payments were 2547 points for days 1 - 7 of hospitalization, 1855 points for days 8 - 15, and 1577 points for 16 - 29 days, independent of the purpose of hospitalization.
The Department of Health Care Economics at the Tokyo Medical and Dental University collected data from 67 hospitals. The Institutional Review Boards of the University of Tokyo (number: KE12-7) and Tokyo Medical and Dental University (number: 839) approved the use of this dataset. The sample period was July-December 2008, and the total numbers of patients for all types of diabetes and those with type 2 diabetes were 4213 (ALOS = 18.3 days) and 3,313 (ALOS = 17.3 days). Of these, 93 patients from the former group and 4 patients from the latter were classified under 100070xxxxxx1x. Among the type 2 diabetic patients, about one-third (1101) participated in educational hospitalization. The data included patients’ LOS, age, gender, principal diseases as per the International Classification of Diseases (version 10) (ICD-10) by the World Health Organization (WHO), reasons for hospitalization, presence of up to four comorbidities and complications, medical treatments, placement after hospitalization, and medical costs. Comorbidities are defined as diseases other than the principal disease at the time of hospitalization, while complications are diseases that occur during hospitalization, including those related and unrelated to the principal disease. The (DPC-based) average cost per patient for educational hospitalization was 434,719 yen and the total cost for all 4213 patients was 2,313,230,070 yen, with educational hospitalization accounting for about 20% of the total cost.
We excluded data for patients treated in clinical departments that do not specialize in the treatment of diabetes, such as pediatrics, orthopedics, psychiatrics, ophthalmology, and otolaryngology. Similarly, data for patients whose disease that caused hospitalization was not diabetes―such as those with gastric cancer, polymyalgia rheumatica, primary thrombocytopenic, myocardial infarction, chronic renal failure, and sudden deafness―were excluded. Figure 1 shows that the medical expenditures of certain patients were unreasonably high compared to their LOS. Data for such patients were deemed unreliable and excluded from the analysis. Thus, the final dataset comprised 991 patients from 28 Red Cross hospitals (i.e., H1-H28) that had at least 10 educational hospitalizations. Among these hospitals, one hospital has 100 - 200 beds, three have 300 - 400, eight have 400 - 500 beds, five have 500 - 600 beds, five others have 600 - 700 beds, three have 700 - 800 beds, two have 800 - 900 beds, and one has 1000 - 1100 beds. Since the average number of beds in a general hospital is about 120, these hospitals are considered to be rather large in scale.
Table 1 summarizes LOS across the hospitals. ALOS and standard deviation (SD) were 14.63 and 6.49 days, respectively, and the skewness and kurtosis were 1.36 and 6.52 for all 28 hospitals. ALOS for H5 was the longest (23.28 days) and that for H12 was the shortest (6.91 days), indicating a difference of 16.4 days and that ALOS for H5 was 3.4 times higher than that of H12. The highest and lowest SDs were 10.39 (H13) and 1.30 (H25) days, with the former’s SD being 8.5 times higher than that of the latter. Therefore, this study found significantly large differences in not only ALOS but also SD.
3.2. Results of Estimation
The explanatory variables in this study were selected on the basis of results from previous studies [9] [17] [18] [27] [28] . The Female Dummy (0: male, 1: female) was used for gender. The numbers for male and female patients were 581 and 410, respectively. Since LOS increases with patients’ age, four age dummies were used: Age 60 - 64, Age 65 - 69, Age 70 - 74, and Age 75 years and above. If the participants fell within the mentioned
![]()
Figure 1. Medical expenditures and the LOS.
![]()
Table 1. Summary of LOS by hospital.
Kurtosis is the value where the normal distribution is 0.
age groups, the value of the dummies equaled 1, and 0 otherwise. The average age and its SD were 60.9 and 13.1 years, respectively. Comorbidities (number of comorbidities) and Complications (number of complications) were used to represent patients’ conditions. Of the study’s participants, 193 patients had no comorbidities and 143, 285, and 370 patients had 1, 2, and 3 comorbidities, respectively. In terms of complications, 723 had none and 116, 66, 43, and 43 had 1, 2, 3, and 4 complications, respectively. Other explanatory variables representing patients’ characteristics were Acute Hospitalization, Another Hospital (i.e., introduced by another hospital), Own Outpatient, and Discharged Place (to another hospital or facility) Dummies. If the patients reported any of these characteristics, the mentioned variables were valued at 1, and 0 otherwise. The numbers of acute hospitalizations, patients introduced by another hospital, already outpatients before hospitalization, and patients discharged to another hospital or facility were 81, 384, 933, and 189, respectively. Figure 2 shows the distribution of LOS. It shows that LOS peaked on days eight (one week after hospitalization) and 15 (two weeks after hospi-
talization). Therefore, Day 8 and Day 15 Dummies were added. The dummies equaled 1 if the patients LOS’ was 8 or 15 days, and 0 otherwise.ICD classifications were used to represent the type of principal disease (diabetes). ICD-10 classifies diabetic patients by type of complication. The classifications include kidney complications (E11.2), ophthalmic complications (E11.3), neurological complications (E11.4), circulatory complications (E11.5), other specified complications (E11.6), multiple complications (E11.7), and without complications (E11.9). Dummy variables based on E11.9 were used to classify principal diseases. Patients 49, 36, 77, 2, 199, 296, and 332 in this study were classified under E11.2, E11.3, E11.4, E11.5, E11.6, E11.7, and E11.9, respectively. Twenty-eight hospital dummies were used to denote the influence of hospitals. These dummies were valued at 1 if hospital i affected patients’ LOS, and 0 otherwise. To evaluate the direct effects of hospitals, a constant term was not used.
Therefore, ![]() of Equation (1) can be presented as
of Equation (1) can be presented as
![]() (12)
(12)
Tables 2-4 present the estimation results for BC MLE, N-estimator, and robust estimators, respectively. The
estimates of ![]() were
were![]() ,
, ![]() , and
, and![]() . We first tested the small
. We first tested the small ![]() assumption. The value of
assumption. The value of ![]() was 0.0725, and
was 0.0725, and ![]() was obtained from Equation (6).
was obtained from Equation (6).
Therefore, the small ![]() assumption was accepted at the 5% significance level. We then tested the assumption
assumption was accepted at the 5% significance level. We then tested the assumption
of homoscedasticity. From Equation (11), ![]() and
and
![]() . Thus, the assumption of homoscedasticity was also accepted at the 5%
. Thus, the assumption of homoscedasticity was also accepted at the 5%
significance level, indicating that BC MLE could be used in this study1. The BC MLE results were used in the remainder of this study.
![]()
1Except Nawata’s estimator [26] [28] , which is adopted in this study, Powell’s [44] is the only known robust estimator that is consistent under heteroscedasticity. One or more instrumental variables are needed to calculate Powell’s estimator; thus, ![]() was chosen. The value of
was chosen. The value of ![]() becomes zero at
becomes zero at ![]() = −0.01, which means the estimate of
= −0.01, which means the estimate of ![]() is −0.01, where
is −0.01, where ![]() are least squares residuals for a given value of
are least squares residuals for a given value of![]() . However, this is an unreasonable value, and thus, Powell’s estimator is not suitable in the context of this study.
. However, this is an unreasonable value, and thus, Powell’s estimator is not suitable in the context of this study.
The Female Dummy was not significant at the 5% level. As for patients’ age, the Age 75 Dummy was posi-
![]()
Table 2. Results of estimation (BC MLE).
*Significant at the 5% level, **Significant at the 1% level.
tive and significant at the 1% level, and the LOS became longer for a patient aged 75 or over. Comorbidities and Complications were positive and significant at the 1% and 5% levels, respectively, indicating that comorbidities and complications prolonged LOS, as expected. Acute Hospitalization, Another Hospital, Own Outpatient, and Discharged Place Dummies were not significant at the 5% level, and the influences of these variables were not admitted. The Day 8 Dummy was negative and significant the 1% level, but the Day 15 Dummy was not signifi- cant at the 5% level. This indicates that one-week hospitalization, and not two-week hospitalization, affected
![]()
Table 3. Results of estimation (N-estimator).
discharge decisions in hospitals. As for ICD-10 classifications, E11.7 was significant at the 1% level, while the other estimates were not significant at the 5% level. Patients classified under E11.7 had multiple complications. Although classification problems may exist2, they are consistent with the results for comorbidities and complications. In other words, higher comorbidities and complications worsen a patient’s condition and prolong LOS. For the hospital dummies, the maximum and minimum estimates were 5.527 for H19 and 2.414 for H12,
![]()
Table 4. Results of estimation (Robust-estimator).
indicating a difference of 3.113―this figure is much higher than the effects of the other variables. Figure 3 illustrates the relationship between ALOS and the estimates of the hospital dummies. The correlation coefficient was 0.947, and there was an almost linear relationship between the two variables. Surprisingly, despite controlling for patient characteristics, significant differences remain across hospitals.
4. Discussion
The estimates of the dummy variables demonstrate the net effects of hospitals on ALOS, thus eliminating the effects of patient characteristics. In other words, LOS for education hospitalization is largely determined by hospitals, and patient characteristics have only a minor influence. As shown in the previous section, significant differences were found across hospitals. Therefore, I examined hospital and regional factors affecting ALOS using the following regression model:
![]() (13)
(13)
![]()
Figure 3. ALOSs and estimates of hospital dummies.
where ![]() is the estimate of Hospital i Dummy,Beds denotes the number of beds and the size of the hospital, Bed Density is the number of beds per 100 thousand people, Population Density is population density per
is the estimate of Hospital i Dummy,Beds denotes the number of beds and the size of the hospital, Bed Density is the number of beds per 100 thousand people, Population Density is population density per![]() , and Average Stay is the ALOS of all patients for general hospitals in the prefecture where the hospital is located. These data were obtained by the hospital survey [33] and the 2010 National Census data [34] . Bed Density and Population Density are represented competition among hospitals and ease of access to hospitals in the region. Average Stay denotes a rough standard of ALOS in the region. Weather may also be a factor hindering the commute to hospitals, especially in cold regions. Temperature is the average annual temperature between 1981 and 2010, recorded at the closest observation point from the hospital [35] . Since all 28 hospitals were Red Cross hospitals, the effect of management was not considered.
, and Average Stay is the ALOS of all patients for general hospitals in the prefecture where the hospital is located. These data were obtained by the hospital survey [33] and the 2010 National Census data [34] . Bed Density and Population Density are represented competition among hospitals and ease of access to hospitals in the region. Average Stay denotes a rough standard of ALOS in the region. Weather may also be a factor hindering the commute to hospitals, especially in cold regions. Temperature is the average annual temperature between 1981 and 2010, recorded at the closest observation point from the hospital [35] . Since all 28 hospitals were Red Cross hospitals, the effect of management was not considered.
The estimation results are provided in Table 5. The standard errors are calculated using the robust estimation method [36] . The estimate of Average Stay was positive and significant at the 5% level. In other words, regional hospitalizations with prolonged ALOS indicated that the hospitals tended to keep their patients for longer terms. Thus, the regional standard of ALOS affected hospitals’ behavior.
According to a hospital survey conducted by the Osaka Prefectural Government [37] , 115 hospitals had educational programs and ALOS varied from a few days to few weeks across the hospitals. The survey also pointed out the poor quality of educational programs; for example, only few hospitals had patient associations that encouraged patients to help each other and exchange correct information about diabetes before and after hospitalization. In fact, some hospitals did not have clinical paths for educational programs. The report also emphasized the importance of regional corporations among hospitals. Reducing ALOS for educational hospitalization by half the time (e.g., from 14 to 7 days) can save as much as 100 billion yen in medical expenses. However, DPC hospitals are required to satisfy certain criteria3, as a result of which their costs are considerably higher than those of small-scale hospitals and clinics. Thus, substantial investments in medical resources for educational hospitalization are a viable option for such hospitals. In other words, future medical policies to control medical costs in Japan must also consider the productivity of hospitals [38] . Evidently, some hospitals must also improve their educational hospitalizations―for example, by ensuring better management of hospitalization schedules [39] ―and modify their programs [40] [41] to reduce ALOS. Regional corporations, hospital networks, clinics, and local administrations such as prefectural governments and public healthcare centers could help realize such improvements. In addition, local corporations and networks can care for diabetic patients before and after hospitalization. This way, patients can join relevant associations, obtain accurate information about diabetes at public
![]()
Table 5. Hospital and regional factors which might affect the LOS.
*Significant at the 5% level.
healthcare centers, and receive periodic medical checks at clinics in their residential areas rather than regularly visiting a hospital
Cavan et al. [42] associated the introduction of ward-based nurse advisors for diabetes patients in January 1998 with significant reductions in LOS for inpatients with diabetes in the United Kingdom. Puig et al. [43] evaluated the impact of consultation by an endocrinology team on the LOS of diabetic patients in a Spanish hospital’s short-stay unit and reported that consultation reduced patients’ LOS. Such approaches can be adopted in Japan to improve regional corporations’ educational programs for diabetic patients.
5. Conclusions
This study analyzed LOS of educational hospitalizations for 991 type 2 diabetic patients in 28 Red Cross hospitals using the BC model. The results of the Hausman test indicated that BC MLE could be used for the purpose of this analysis. The variables found to affect LOS were patients’ age (75 and above), numbers of comorbidities and complications, the day 8 dummy, and the principal disease classification E11.7. The analysis also found significant differences in the LOS across hospitals, even after controlling for patient characteristics. This proves that LOS is primarily affected by hospitals, while patient characteristics have only marginal effects. In addition, it was found that ALOS for all patients in general hospitals in a given prefecture affected LOS. Thus, it may be necessary for some hospitals to revise their current educational programs by improving their management of hospitalization schedules and adopting appropriate educational programs for the effective use of medical resources. This can be easily facilitated by regional corporations, hospital networks, clinics, and administrations, such as prefectural governments and public healthcare centers. Regional corporations and networks can also facilitate caring for patients before as well as after hospitalization.
With the introduction of DPC/PDPS, an enormous amount of medical information has been computerized. Future research can access this information to evaluate other important diseases to facilitate the effective use of medical resources.
Acknowledgements
This study was supported by a Grant-in-Aid for Scientific Research, “Analyses of Large Scale Medical Survey Data and the Policy Evaluations in Japan (Grant Number: 24330067),” from the Japan Society of Science. We would like to thank two anonymous referees and Prof. Yoshiyuki Takeuchi of Osaka University for their helpful comments and suggestions.
NOTES
2Classification problems may exist among DPC codes, comorbidities, complications, and IDC-10 classifications. Since DPC codes are determined by the principal disease―for which most medical resources were used during hospitalization―and not the disease that causes hospitalization, some ambiguity may exist in their classifications among hospitals. For example, neither comorbidities nor complications were reported for 7, 6, 6, 8, 17, and 34 patients classified under E11.2, E11.3, E11.4, E11.6, and E11.7, respectively. These patients should have been classified under E11.9. On the other hand, among the 324 patients classified under E11.9, 224 had comorbidities, 58 had complications, and only 93 were free from comorbidities and complications. Diabetic patients with the DPC code 100070xxxxxx0x had similar medical payments, independent of the IDC-10 classifications. Although the findings of the analysis―comorbidities and complications prolonged LOS―were not affected by these problems, establishing a standard classification method across hospitals seems crucial to improve the quality of data in the future.
![]()
3The basic criteria to qualify as a DPC hospital are as follows [45] : 1) A hospital must provide acute medical care, and the patient-nurse ratio must be 7:1 or 10:1. (In Japan, hospitals are classified into four categories on the basis of patient-nurse ratios. They are 7:1, 10:1, 13:1, and 15:1. The medical payments to hospitals are determined by these categories.) 2) A hospital must participate in DPC surveys and provide proper data to those conducting the surveys. 3) A hospital must set up a coding committee for accurate DPC coding. The committee members must comprise a person in charge of coding, a medical doctor, a pharmacist, and an individual from a division that records medical information or handles medical payments. A committee meeting must be held at least twice a year.