Open Journal of Thoracic Surgery
Vol.2 No.3(2012), Article ID:23037,6 pages DOI:10.4236/ojts.2012.23015
Surgical Correction of Tetralogy of Fallot in Adulthood
![]()
1Pediatric Cardiovascular Surgery Unit, Fundación Favaloro University Hospital, Buenos Aires, Argentina; 2Department of Pediatric Cardiology, Fundación Favaloro University Hospital, Buenos Aires, Argentina.
Email: ignaciolugones@hotmail.com
Received April 3rd, 2012; revised May 2nd, 2012; accepted May 11th, 2012
Keywords: Adult Congenital Heart Disease; Congenital Heart Surgery; Postoperative Care; Pulmonary Arteries
ABSTRACT
Background: The aim of this study is to evaluate the short-term results of surgical correction of Tetralogy of Fallot in adult patients. Methods: Between 1999 and 2007, surgical correction was performed in 16 adult patients (mean age: 34.6 years; range: 18 to 62). Five previous procedures had been performed in 4 patients. Thirteen patients were in NYHA functional classification III or IV (81%), and 12 were cyanotic. Echocardiography was performed in all patients and 14 of them were catheterized. The mean gradient in the right ventricular outflow tract was 82 mmHg. Four patients had unfavorable anatomy, consisting in coronary fistulas (2) and small pulmonary artery branches (2). Results: Infundibular resection was performed in all patients, ventricular septal defect closure in 15, pulmonary valve commissurotomy in 8, right ventricular outflow tract patch enlargement in 9 and transannular patch placement in 4. Three patients died during the postoperative hospital stay, 2 of them due to sepsis. All of them had unfavorable anatomy and impaired preoperative condition. No residual defects were found. The other 13 patients had a good recovery. Eleven had less than 24 hours of mechanical ventilation. Early hospital discharge was possible in all survivors. Conclusion: Surgical correction of Tetralogy of Fallot in adulthood is an infrequent procedure. The short-term results depend mostly on the anatomic substrate and the preoperative clinical condition of the patient.
1. Introduction
Tetralogy of Fallot (TF) is a complex congenital heart disease caused by anterior and cephalic deviation of the conal septum during heart development. This malalignement of the embryonic conotruncal septum with the interventricular septum determines the existence of a ventricular septal defect (VSD) and varying degrees of right ventricular outflow tract (RVOT) obstruction. The large aortic root overrides the septum and the right ventricle becomes hypertrophic. Usually, the severity of the RVOT obstruction determines the clinical features. Severe forms produce intense cyanosis and early manifestations, while mild hemodynamic alterations can delay presentation and diagnosis.
Since the first report of complete correction of TF in 1955, there has been a continuous trend towards correction at earlier ages. This might be the reason why untreated or palliated adult patients are so unusual. Thus, the chance of extending their lives with corrective surgery becomes a hard challenge. Although the cardiac anatomy of these patients is theoretically favorable, the associated pathologies derived from the uncorrected disease determine the high mortality rate of the surgical repair.
The aim of this study is to describe our experience in the surgical repair of TF in patients older than 18 years of age, and to identify potential risk factors for postoperative mortality.
2. Material and Methods
We performed a retrospective study using medical records as the source of information. Several categorical and numerical variables were determined. Tables were used to describe the data. Statistical analysis was performed using Epi Info software (version 3.3.2). The p-values < 0.05 were considered statistically significant.
2.1. Patients
Between August 1999 and September 2007, surgical correction of TF was performed in 16 patients older than 18 years of age at the Fundación Favaloro University Hospital. The mean age was 34.6 years (range: 18 to 62 years). Twelve patients were female and 4 were male.
2.2. Preoperative Evaluation
All available data were collected from medical records and retrospectively analyzed. In addition to general and surgical medical history, the following variables were collected: New York Heart Association functional classification (NYHA FC), oxygen saturation, presence of cyanosis, physical examination, hematocrit and blood pressure. Results of additional studies were also recorded. These data are summarized in Table 1.
Five patients had one or more comorbidities. One patient had diabetes mellitus and osteoporosis. The second one suffered from syphilis, chronic obstructive pulmonary disease, atrial flutter and neurological sequelae of a previous stroke. The third had tuberculosis. The fourth patient presented arterial hypertension and uterine fibromas, and the last one suffered from asthma. Eight spontaneous abortions were confirmed in 3 patients. Some other events were also identified, such as multiple pneumonias in 1 patient, syncopes in 2 and hemoptysis in other 2 patients.
Five palliative surgeries had been previously performed in 4 patients. Four of these procedures, done in 3 patients, were Blalock-Taussig shunts. The remaining intervention was an atrial septal defect closure carried out in 1970. None of aforementioned surgeries had been performed in our institution.
From the clinical point of view, 13 patients (81%) were in NYHA FC III or IV, with severe impairment. Twelve patients (75%) were cyanotic. The mean arterial saturation was 82% (range: 55% to 97%) and the mean hematocrit was 52%. At cardiac auscultation, a systolic ejection murmur in the pulmonary area was usually detected. In patients with a previous shunt, a continuous parasternal murmur was also heard.
Sinus rhythm was present in 85% of the cases; two patients did not have it. The first one showed atrial fibrillation and the second one ectopic atrial rhythm. There were signs of dilation of the right atrium in 50% of the cases. Furthermore, 28% of the patients presented right bundle branch block and 71% showed signs of right ventricular hypertrophy.
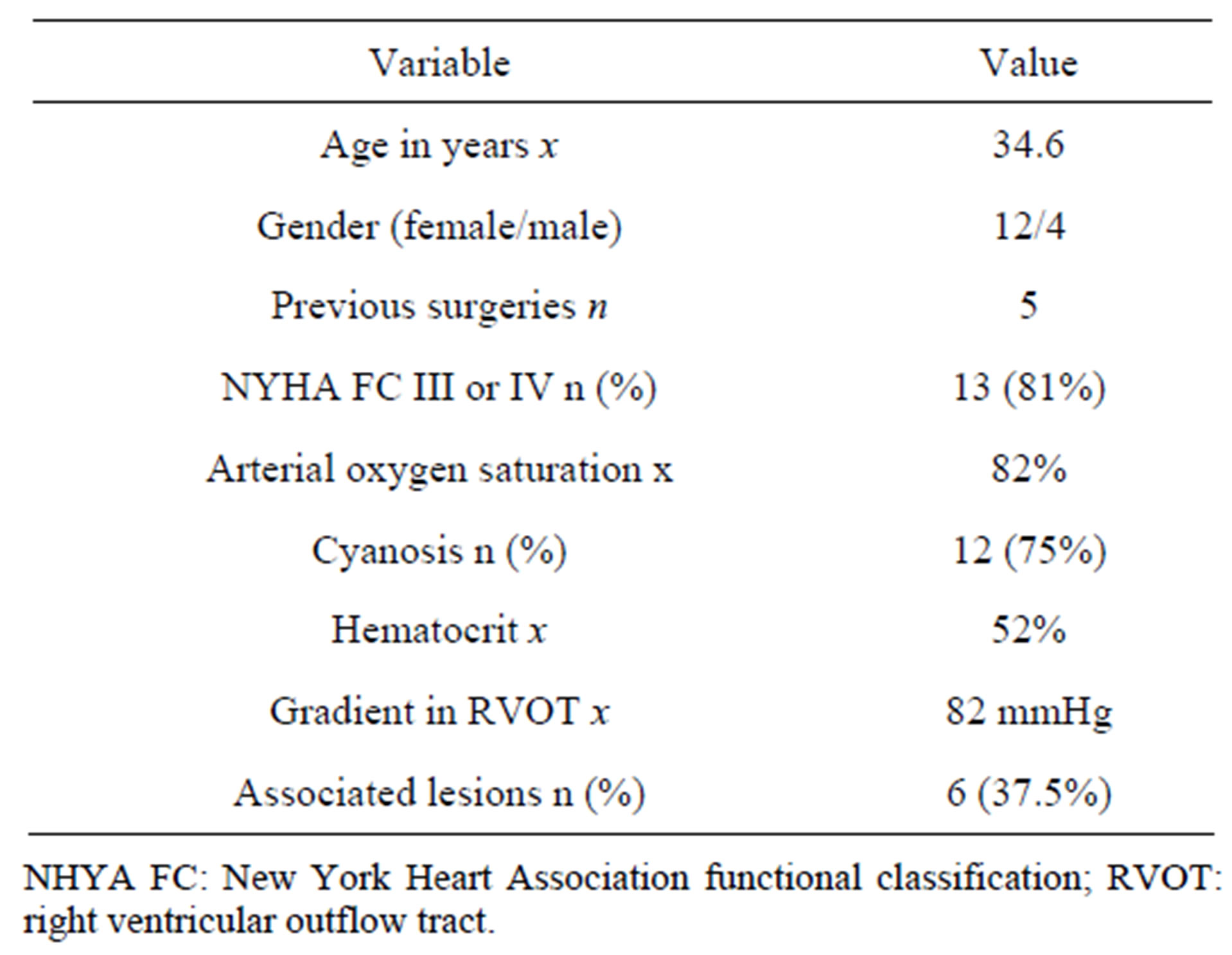
Table 1. Preoperative characteristics.
Diagnosis was confirmed by Doppler echocardiography in all patients. Typical findings were the presence of an unrestrictive subaortic VSD and variable degrees of RVOT obstruction. Fourteen patients underwent cardiac catheterization to assess oxygen saturation and pressures in each segment, to accurately delineate the anatomy and to evaluate the results of previous surgeries. The average gradient in the RVOT was 82 mmHg. This method also allowed us to investigate possible obstructive lesions in the coronary arteries. In 3 patients, cardiac magnetic resonance imaging was used to complement previous studies.
Eight patients (50%) presented associated cardiac anomalies (Table 2).
With the exception of atrial septal defects, hypoplastic pulmonary artery branches and fistulas between the coronary arteries and other segments were the anomalies most frequently found. One patient had a fistula connecting the left anterior descending and circumflex arteries with the right ventricle. He also had another large fistula, extended between the circumflex artery and the right pulmonary artery branch. In other 2 patients, there were fistulas directed to the main pulmonary artery. One last patient presented a fistula connected to the left ventricle.
2.3. Surgery
Corrective surgery was performed in all patients using cardiopulmonary bypass with moderate hypothermia. The routine use of tranexamic acid prevented episodes of major postoperative bleeding. Previous shunts were fully dissected before heparin administration, and they were closed just after initiation of the cardiopulmonary bypass. Intermittent administration of cold cardioplegic infusion was the chosen myocardial protection method.
Although the right atriotomy was considered the best approach for the repair, a ventriculotomy in the RVOT had to be performed in 15 patients. This was due to the impossibility to achieve an adequate infundibular resection through the atriotomy or the need to place a

Table 2. Associated lesions.
transannular patch. After relieving the infundibular obstruction, pulmonary valve commissurotomy was performed in 8 patients. The VSD was closed with a Dacron® patch in all cases. One patient had severely hypoplastic pulmonary artery branches and a small pulmonary valve annulus. We left the VSD open since its closure would have caused suprasystemic right ventricular pressure after correction. The ventriculotomy was closed with pericardium treated in glutaraldehyde in 13 patients. In 4 of these patients, the patch was placed in a transannular position, enlarging the pulmonary annulus and extending into the main pulmonary artery.
We carried out 5 additional procedures in 4 patients. In each case we closed an atrial septal defect. We also performed the closure of 3 muscular VSDs in one of those patients. These data are summarized in Table 3.
The mean times of cardiopulmonary bypass and aortic cross-clamping were 114.8 minutes (range: 88 to 176) and 64.4 minutes (range: 39 to 93), respectively.
3. Results
Three patients (18.75%) died during hospital stay. In 2 patients, the cause was sepsis, at days 28 and 70 after surgery. Both of them were undergoing a delicate postoperative course, with prolonged mechanical ventilation and multiorgan failure. The remaining patient developed cardiac and renal failure, both unresponsive to medical therapy, and died 3 days after surgery. All non-survivors had unfavorable anatomy and severe preoperative clinical condition. No residual lesions were detected in the postoperative echocardiograms.
Univariate analysis demonstrated a statistically significant difference between survivors and non-survivors regarding preoperative saturation (p = 0.0035), and the presence of coronary fistulas (p = 0.0366) and hypoplastic pulmonary artery branches (p = 0.0366). Nonsurvivors had higher hematocrit, worse preoperative NYHA FC and higher gradient across the RVOT than

Table 3. Procedures performed during surgery.
survivors. They were also older and more cyanotic. These data are summarized in Table 4.
The evolution in the 13 survivors was excellent, with less than 24 hours of mechanical ventilation in 11 patients. Inotropic support with dopamine at low doses was maintained during the first 48 hours. Hospital stay was brief and every patient received an early discharge.
4. Discussion
Despite the current global trend to correct TF during the first year of life [1], there is a large group of individuals who go through infancy without surgical treatment. In rare cases, these untreated patients reach adulthood. It is estimated that only 12% turns 20 years old and barely 3% reaches the fourth decade of life [2].
This small subset of adults without correction represents a major challenge for the health care system. Their unique features require a multidisciplinary team that includes pediatric cardiologists, congenital cardiovascular surgeons and adult intensivists.
Prolonged survival without surgery is usually determined by a favorable anatomy and a delicate and infrequent physiological balance. Many of these patients have mild pulmonary artery and annulus hypoplasia, in combination with a progressive development of infundibular obstruction and left ventricular hypertrophy [3]. This would protect them from a severe right to left shunt at the ventricular level. Besides, the presence of an additional pulmonary flow source such as a ductus arteriosus or aortopulmonary collaterals improves oxygenation.
Despite these favorable anatomic features, these patients suffer from other diseases of adulthood and the complications derived from many years of a cyanotic congenital heart disease. This might explain the higher mortality rate of this subgroup compared to infants and children. Chronic hypoxemia causes myocardial fibrosis with the subsequent development of ventricular dysfunction [4]. Other complications are given by polycythemia, coagulation disturbances, thromboembolism, stroke, arrhythmias and infective endocarditis. Previous surgeries can also induce anatomic distortions that require correction [5].
Previous studies have warned about the increased perioperative mortality and the decreased long-term survival at older age at the time of intervention [6,7]. Our analysis is consistent with those findings. The mean age of non-survivors was 47.66 years old, compared with 31.61 years old in survivors.
Preoperative clinical condition is also a key factor in the outcome of surgical correction. The severe impairment of our population is evidenced by the high proportion of cyanotic and NYHA FC III or IV patients. Besides, the average oxygen saturation was significantly lower in non-survivors than in survivors. This is in concordance

Table 4. Univariate analysis.
with the findings shown by Dittrich and collaborators, who defined severe insaturation, biventricular dilation, high end diastolic pressures and significant tricuspid regurgitation as predictors of augmented surgical risk [4].
The role of the associated lesions and their resolution has vital importance. We found a statistically significant difference between survivors and non-survivors in the presence of coronary fistulas and hypoplastic pulmonary artery branches. Both lesions were associated with higher early postoperative mortality.
Coronary fistulas may connect with the ventricles and with the pulmonary artery and its branches (Figure 1). The prevalence of the latter in TF is up to 11% [8]. Three of our patients (18.75%) had them, and 2 of them also had fistulas directed to ventricles. Even though they provide additional pulmonary blood flow, they can cause important volume overload and “coronary steal”. It is important to know their location and pathway by preoperative catheterization, magnetic resonance imaging or computed tomography. Although some cases of spontaneous closure after correction of TF have been described [9], most of them require occlusion, either by catheterization or surgery. Surgical occlusion is performed in a similar way to aortopulmonary collaterals, just after the beginning of cardiopulmonary bypass and before cardioplegic arrest, to avoid altering myocardial protection [10].
The pulmonary artery and its branches play a vital role in the postoperative period [11]. Adequate dimensions of
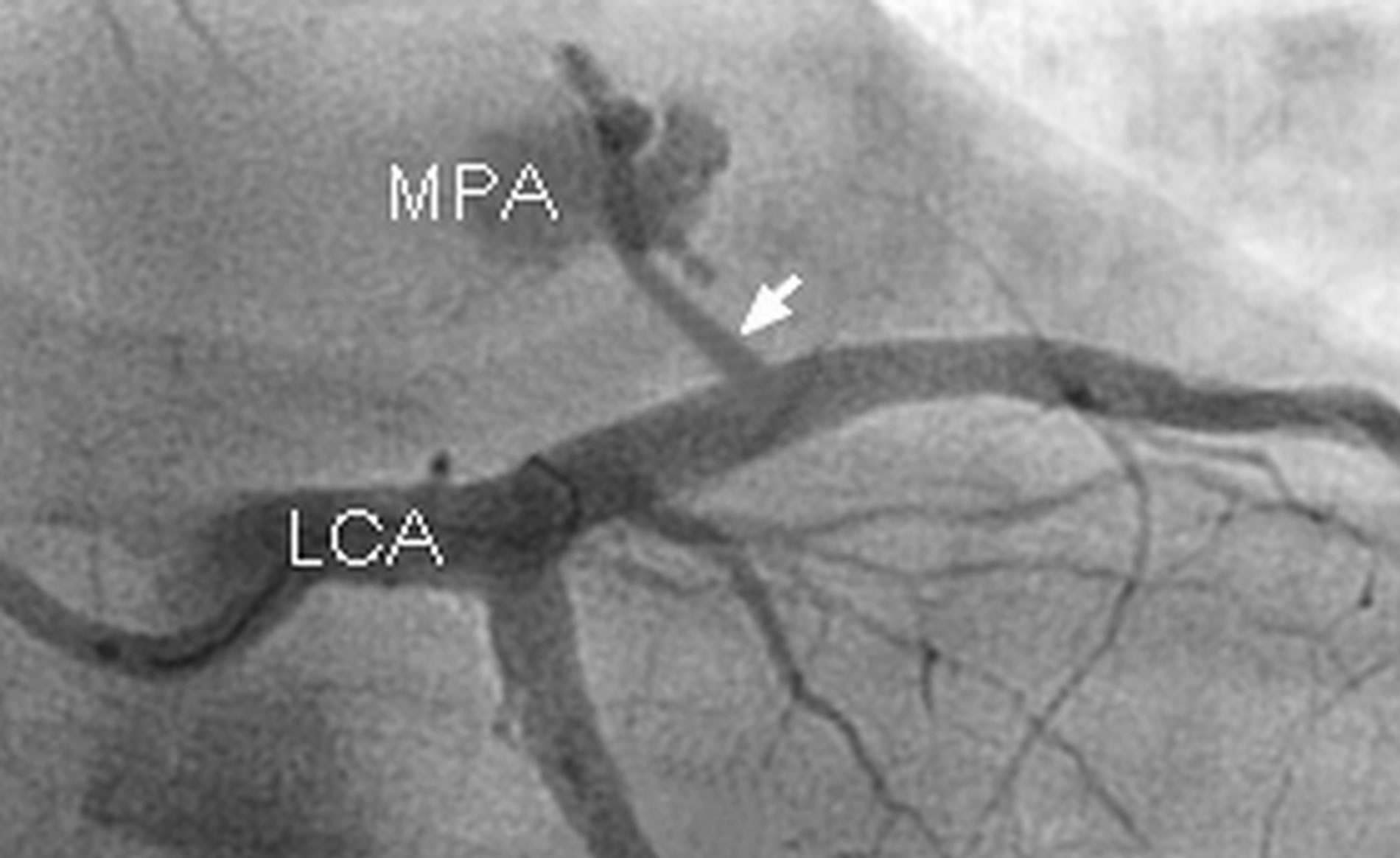
Figure 1. Left coronary artery angiography showing a fistula connecting the circumflex artery with the main pulmonary artery. (MPA: main pulmonary artery, LCA: left coronary artery, arrow: fistula).
these structures and low vascular resistance have a positive influence on outcome. In contrast, hypoplasia of the pulmonary artery branches leads to high right ventricular pressure in the postoperative period, with the consequent risk of ventricular failure. This happened in 3 of our patients, in whom Nakata indexes were lower than 200 mm2/m2 (Figure 2). This feature had a statistically significant negative impact on early postoperative mortality.
During surgery, particular attention must be taken to certain details. Previous shunts must be taken down and cut to relieve any possible distortion in the pulmonary artery branches. Aortopulmonary collaterals must also be

Figure 2. Angiography showing marked hypoplasia of pulmonary annulus, main pulmonary artery and its branches in a 42-year-old female patient. (Ao: aorta; MPA: main pulmonary artery; RVOT: right ventricular outflow tract.)
occluded systematically to avoid volume overload during the postoperative period. Myocardial protection of these markedly hypertrophied hearts must be extremely careful. Closing coronary fistulas before aortic crossclamping could be a useful maneuver to avoid losing cardioplegia.
When the pulmonary annulus is hypoplastic or infundibular resection is not possible through a right atriotomy, a ventriculotomy in the RVOT must be performed. This approach was necessary in almost all our patients, unlike what happened in other series, in which the use of the atrial approach reached 41% of the cases [12]. When annulus hypoplasia is present, the ventriculotomy is extended to the main pulmonary artery, transecting the annulus. This procedure was performed in 25% of our patients. If this is not necessary, the incision is limited to the RVOT. Section and resection of the hypertrophic muscle bands releases obstruction. Care must be taken not to weaken the right ventricular free wall. For VSD closure, the use of separate pledgeted stitches is recommended to prevent damage of the friable tissue of this region. The ventriculotomy confined to the RVOT is usually closed with glutaraldehyde treated pericardium or Dacron®. The latter is rigid and reduces the incidence of RVOT aneurysm. In contrast, untreated pericardium significantly increases the incidence of such aneurysms [13]. The transannular patch can be complemented with a monocuspid valve made of pericardium or thin expanded polytetrafluoroethylene. This monocusp is sutured to the inner surface of the patch or to the internal edges of the ventriculotomy. This could avoid severe pulmonary regurgitation, protecting the hypertrophic ventricle from volume overload of sudden installation in the immediate postoperative period.
Despite the severe clinical condition of these patients, the complex surgical correction and the high mortality rate associated to this procedure, many studies have demonstrated the benefits of the repair of TF in adulthood. The long-term survival has been shown to be higher compared to patients treated only with medication [12,14]. Similarly, NYHA FC and quality of life improve substantially after surgery [15].
5. Conclusion
Surgical correction of TF in adulthood is a procedure rarely performed. The short-term results depend mostly on the anatomic substrate and the preoperative clinical condition of each patient. Coronary fistulas and hypoplastic pulmonary artery branches have a statistically significant negative impact on mortality. Severe insaturation is also a predictor of augmented surgical risk. Mortality remains high in this subset of patients. Therefore, identifying good candidates for surgical repair becomes extremely important. Young acyanotic patients showing favorable anatomy and acceptable preoperative condition can be safely treated. On the other hand, older cyanotic patients with severe impairment and coronary fistulas or hypoplastic pulmonary artery branches have a substantially higher risk of early postoperative death. Such cases must be carefully analyzed before an aggressive surgical approach is chosen.
REFERENCES
- G. Van Arsdell, G. Maharaj, J. Tom, V. Rao, J. Coles, R. Freedom, W. Williams and B. McCrindle, “What Is the Optimal Age for Repair of Tetralogy of Fallot?” Circulation, Vol. 102, Suppl. III, 2000, pp. 123-129.
- E. Bertranou, E. Blackstone, J. Hazelrig, M. Turner and J. Kirklin, “Life Expectancy without Surgery in Tetralogy of Fallot,” American Journal of Cardiology, Vol. 42, No. 3, 1978, pp. 458-466. doi:10.1016/0002-9149(78)90941-4
- X. Yang, L. Freeman and C. Ross, “Unoperated tetralogy of Fallot: Case Report of a Natural Survivor Who Died in His 73rd Year; Is It Ever Too Late to Operate?” Postgraduate Medical Journal, Vol. 81, 2005, pp. 133-134. doi:10.1136/pgmj.2004.020172
- S. Dittrich, M. Vogel, I. Dahnert, F. Berger, V. AlexiMeskishvili and P. Lange, “Surgical Repair of Tetralogy of Fallot in Adults Today,” Clinical Cardiology, Vol. 22, No. 7, 1999, pp. 460-464. doi:10.1002/clc.4960220705
- E. Atik and F. A. Atik, “Tétrade de Fallot: Qual o Real Benefício da Correção OperatóRia na Idade Adulta?” Arquivos Brasileiros de Cardiologia, Vol. 83, No. 4, 2004, pp. 278-279. doi:10.1590/S0066-782X2004001600002
- M. Gatzoulis, S. Balaji, S. A. Webber, S. C. Siu, J. S. Hokanson, C. Poile, M. Nakazawa, J. Moller, P. Gillette, G. D. Webb and A. N. Redington, “Risk Factors for Arrhythmia and Sudden Cardiac Death Late after Repair of Tetralogy of Fallot: A Multicentre Study,” Lancet, Vol. 356, No. 9234, 2000, pp. 975-981. doi:10.1016/S0140-6736(00)02714-8
- N. M. Katz, E. H. Blackstone, J. W. Kirklin, A. Pacifico and L. M. Bargeron Jr., “Late Survival and Symptoms after Repair of Tetralogy of Fallot,” Circulation, Vol. 65, 1982, pp. 403-410. doi:10.1161/01.CIR.65.2.403
- R. Dabizzi, G. Caprioli, L. Aiazzi, C. Castelli, G. Baldrighi, L. Parenzan and V. Baldrighi, “Distribution and Anomalies of Coronary Arteries in Tetralogy of Fallot,” Circulation, Vol. 61, No. 1, 1980, pp. 95-102. doi:10.1161/01.CIR.61.1.95
- T. Kadokami, H. Shimokawa, A. Ito, M. Mohri and A. Takeshita, “Disappearence of Coronary Artery-Ventricular Fistulas after a Radical Operation for Tetralogy of Fallot,” Japanese Circulation Journal, Vol. 60, No. 8, 1996, pp. 624-627. doi:10.1253/jcj.60.624
- S. Talwar, P. Sharma, G. S. Gulati, S. Kothari and S. Choudhary, “Tetralogy of Fallot with Coronary Artery to Pulmonary Artery Fistula and Unusual Coronary Pattern: Missed Diagnosis,” Journal of Cardiac Surgery, Vol. 24, No. 6, 2009, pp. 752-755. doi:10.1111/j.1540-8191.2009.00917.x
- C. Erdal, M. Kir, E. Silistreli, G. Albayrak, O. Karabay, G. Saylam and U. Açikel, “Pulmonary Segmental Artery Ratio: An Alternative to the Pulmonary Artery Index in Patients with Tetralogy of Fallot,” International Heart Journal, Vol. 47, No. 1, 2006, pp. 67-75. doi:10.1536/ihj.47.67
- F. A. Atik, E. Atik, C. R. da Cunha, L. F. Caneo, R. S. Assad, M. B. Jatene, A. Riso and M. Barbero-Marcial, “Long-Term Results of Correction of Tetralogy of Fallot in Adulthood,” European Journal of Cardiothoracic Surgery, Vol. 25, No. 2, 2004, pp. 250-255. doi:10.1016/j.ejcts.2003.11.002
- T. Tirilomis, M. Friedrich, D. Zenker, R. G. Seipelt, F. Schoendube and W. Ruschewski, “Indications for Reoperation Late after Correction of Tetralogy of Fallot,” Cardiology in the Young, Vol. 20, No. 4, 2010, pp. 396-401. doi:10.1017/S1047951110000442
- G. Nollert, T. Fischlein, S. Bouterwek, C. Bohmer, O. Dewald, E. Kreuzer, A. Welz, H. Netz, W. Klinner and B. Reichart, “Long-Term Results of Total Repair of Tetralogy of Fallot in Adulthood: 35 Years Follow-Up in 104 Patients Corrected at the Age of 18 or Older,” The Thoracic and Cardiovascular Surgeon, Vol. 45, No. 4, 1997, pp. 178-181. doi:10.1055/s-2007-1013719
- P. Presbitero, S. B. Prever, I. Contrafatto and M. Morea, “As Originally Published in 1988: Results of Total Correction of Tetralogy of Fallot Performed in Adults. Updated in 1996,” Annals of Thoracic Surgery, Vol. 61, No. 6, 1996, pp. 1870-1873. doi:10.1016/0003-4975(96)00180-4

