Forensic Medicine and Anatomy Research
Vol. 1 No. 4 (2013) , Article ID: 37375 , 6 pages DOI:10.4236/fmar.2013.14016
Variation of blood vessels in the cranial-cervical legion
![]()
1Department of Legal Medicine, Shiga University of Medical Science, Ōtsu, Japan; *Corresponding Author: 31041220@belle.shiga-med.ac.jp
2Institute of Legal Medicine, Munich University, Munich, Germany
Copyright © 2013 Satoshi Furukawa et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received 9 May 2013; revised 19 June 2013; accepted 1 July 2013
Keywords: Variation of the Vessels; Forensic Pathology
ABSTRACT
The blood vessels in the head and neck have several main roots for supplying blood to the brain and returning of blood to the heart. It was well known that each artery and vein in the head and neck has its variation. The variation of the vessels some times gives rise to un-expectable findings, which are not described in the textbook. In this study we like to show the morphological variations observed at routine autopsy cases and some forensic pathological findings caused by those variations.
1. INTRODUCTION
We have examined the variation of blood vessels in the Willis circle and neck, after we have experienced one autopsy case where an old lady died due to cardiac tamponade with ascending aorta dissection. Her face showed severe congestion with severe bleeding in the conjuncttiva tongue and scalp, since she was found death in a head-down tile and her internal jugular veins were incomplete [1]. Since then we have studied and reported about morphological and distributional variations in blood vessels in the neck and Willis circle [2-6]. In this study we show morphological and distributional variation of the blood vessel in the cranial-cervical legion. And we present some rare autopsy cases caused by the variation of the blood vessels.
2. MATERIALS AND METHODS
As a routine examination, we have been performing observational study concerning existence of internal jugular vein valve, width of right and left internal jugular vein, entering level of the vertebral artery into transverse foramina, and morphology of Willis circles at autopsies.
3. RESULTS
3.1. The Internal Jugular Vein
3.1.1. Internal Jugular Vein Valve
In our recent observation in 200 autopsy cases, Valves were normally located at the level of superior upper margins of clavicles and present bilaterally 93% subject, unilaterally 5% and aplstic 2%, and bicuspid valves were 70.5%.
This observation is now continued and we find some individuals with incompetent valve and atypical valves, such as tricuspid valve, different direction of valve attached left and right side of the vessel, and high level that is C6 or more, respectively.
1) A Head down Tile Victim with Severe Bleeding in Face and Scalp A 76-year-old woman described above was found death in her dining-kitchen. She sat on a chair but upper part of her body slipped down from the chair after her death. She had severe bleeding in her conjunctiva, tongue, and scalp (Figure 1). There were valves in her internal and external jugular veins, however, these valves were incompetence with histological examination according to Sanchez-Hanke et al. [7]. This case was doubted as a murder one when police investigated her body.
2) A Head down Tile Victims without Conjunctiva Petechiea A 62-year-old man was found death in a concrete box with 45 cm × 90 cm wide and 120 cm deep, which was dug in the ground to form a stopcock for water supply to his rice field. He was 169 cm in height and weighted 77 kg, and was completely upside-down in the box. There was congestion and severalpetechiea on his face and conjunctiva, but no bleeding was observed in the tongue and scalp (Figure 2). His internal and external jugular veins had bicuspid valves. During working to open the cock, he accidentally felled into the box and died due to cervical vertebrate fracture.
3.1.2. Width of Internal Jugular Veins and Relationship of Distribution of the Common Carotid Arteries and Internal Jugular Veins
The width of the internal jugular vein was usually larger in right side than that in left side one, however some variations were recognized, that is, 10 of 200 individuals have larger one on their left side veins, and 15 individuals showed the same size. The largest one was 2.5 cm in right side and 2.3 cm in left side. We did not find aplastic case of internal jugular vein.
 (a)
(a) (b)
(b) (c)
(c)
Figure 1. Case A-1-1. Severe bleeding in the conjunctiva (a), scalp (b) and tongue was detected of an old woman who died due to cardiac tamponade caused by rupture of the ascending aortic aneurysm. She was found in head down tile posture.
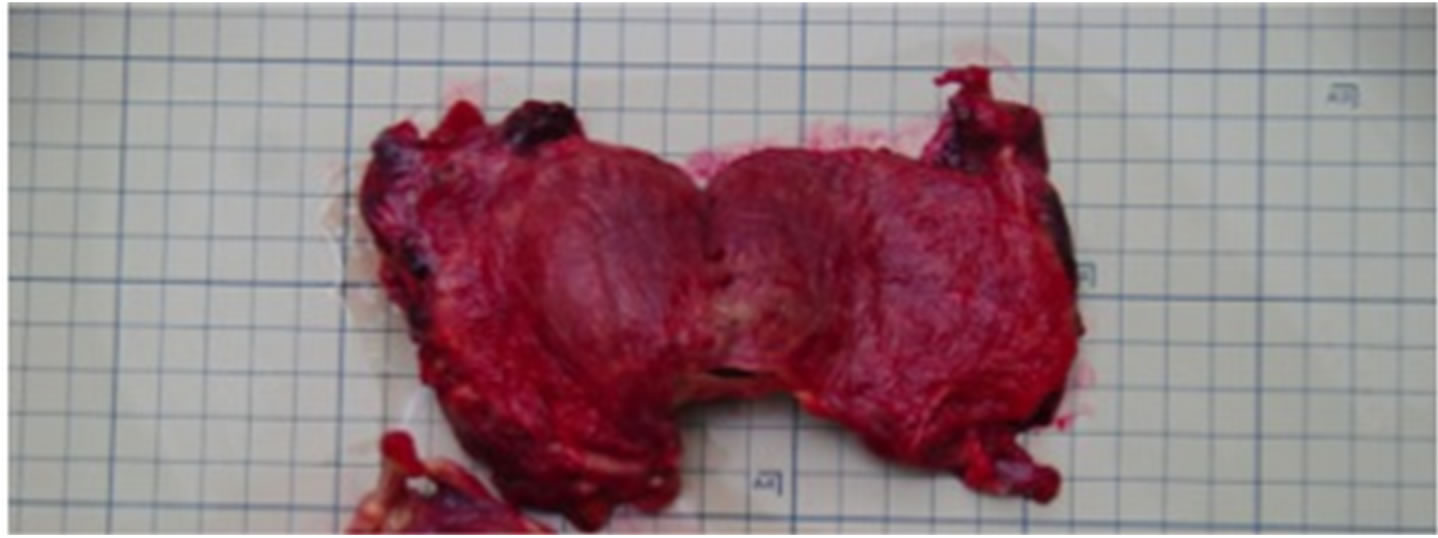
Figure 2. Case A-1-2. Congestion was detected in the both side conjunctiva from an old man who died due to cervical fracture and drawing when he full down into a hole during preparing water flow valve to his rice field. No bleeding in the tongue was observed. He was found upside down posture.
Usually common carotid artery and internal jugular vein are parallel to each other, however we found some variations. In 30% of individuals these vessels were closed to each other. We found two rare cases described bellow.
1) The Crossing of the Artery and Vein in Right Side of a Male A 65-year-old man lost his consciousness in his house and died after three hoursdespite the emergency medical service he died. Autopsy revealed that his right side internal jugular vein laid crossing to the common carotid artery and he died due to cardiac infarction. In this case, the bleeding in right side neck was detected (Figure 3), since an intravenous injection was attempted to make the cannulation to vena cava superior at the hospital.
2) The Left Internal Jugular Vein Lies inside the Carotid Artery The left internal jugular vein lied inside of the common carotid artery was found in a 71-year-old woman (Figure 4). She died due to blood loss caused by selfstab wound to the chest. This variation seems to be very rare.
3.2. The Vertebral Artery
We detected 5 cases of vertebral artery variation in the recent 200 autopsy cases. In these cases the both side vertebral artery entered into canal at 5th vertebrate level.
A Woman Died Due to Compression of Both Side of Neck
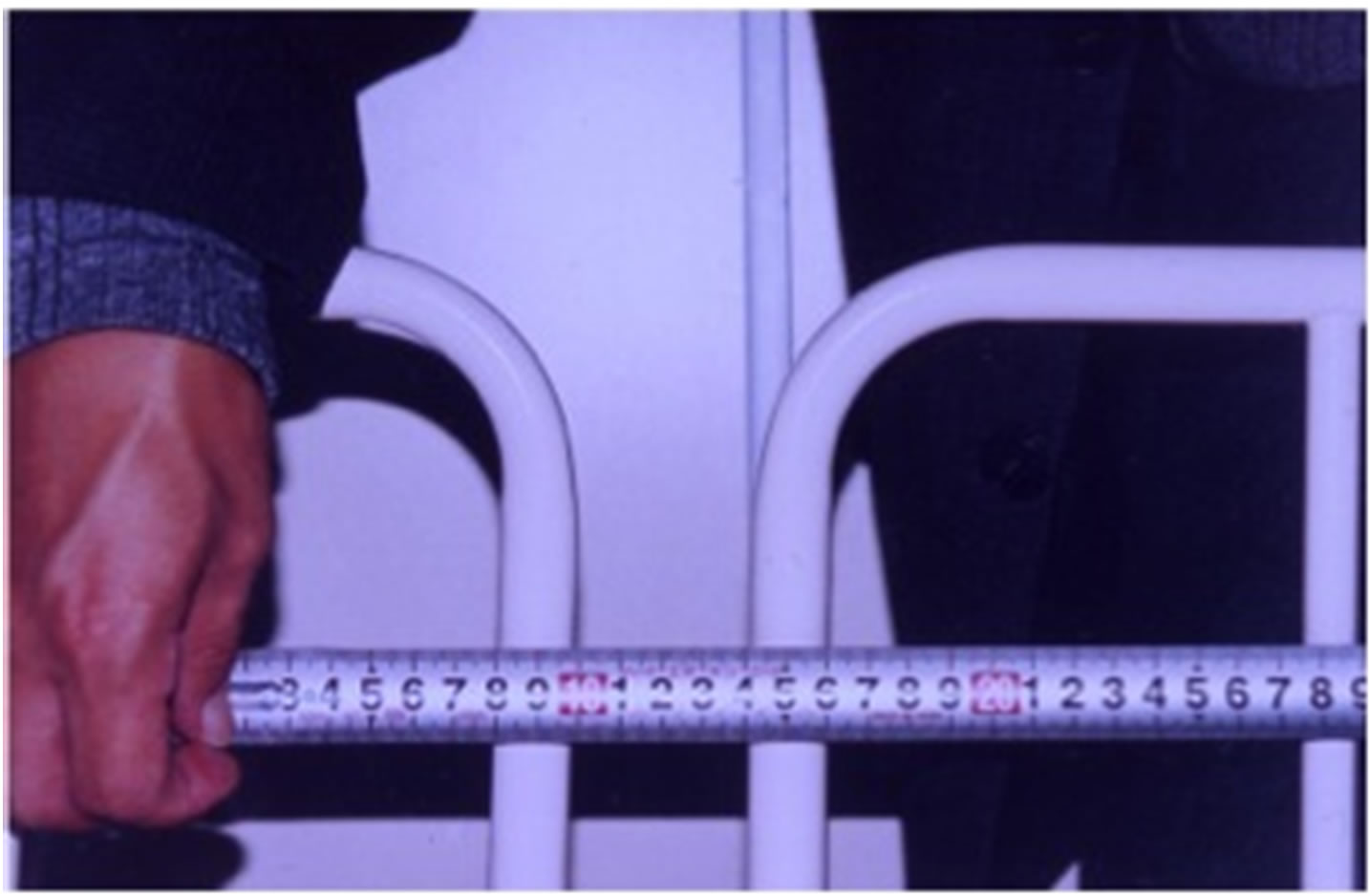
We encountered one case where 71-year-old female died due to compression of both side neck when she crumpled to bed-side in a hospital, and she was fasten her neck between two bed-side fences with a space of 4 cm width (Figure 5(a)). There was no-petechiae in her
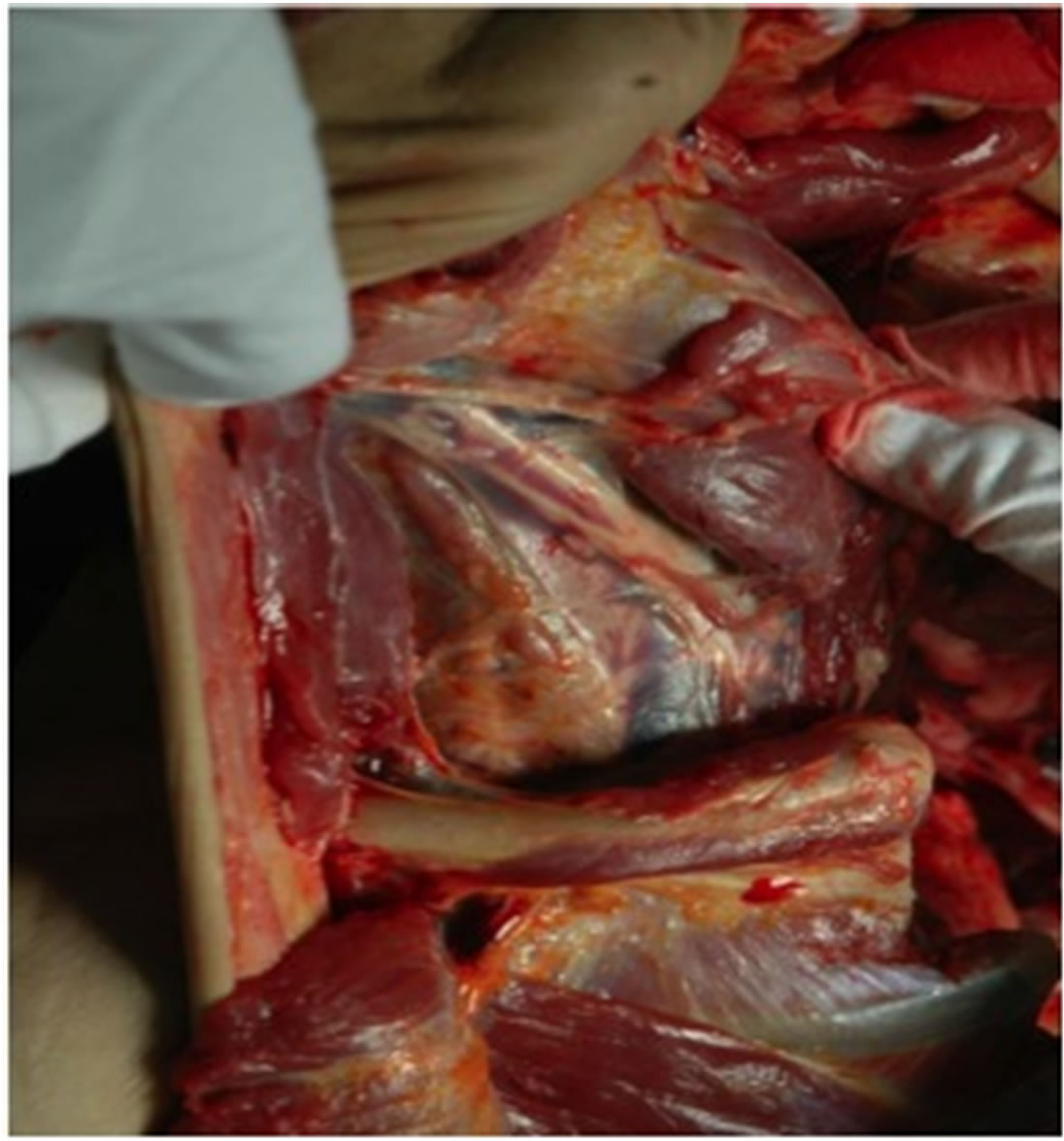
Figure 3. Case A-2-1. The right side internal jugular vein lays crossing over the carotid artery.
conjunctiva and face (Figure 5(b)). We found her both side vertebrate arteries entered into 6th vertebral, and the compression mark with severe bleeding was observed in the muscles at 6 and 7th vertebral level (Figure 5(c)), however no injury on the neck skin.
This case indicates that in a murder case by cervical strangulation with lower level we can not recognize facial congestion and petechiae in the conjunctiva of a victim whose vertebral artery enter into canal of 5th vertebrate or at much higher level.
3.3. Level of the Bifurcation of Common Carotid Artery
In our observation the distribution frequent of the bifurcation of common carotid artery located from C2 (Figure 6) to C5 level, and most frequent was C3 level, as shown in Table 1. Some individuals showed different level among the sides. We have no autopsy case where compression of bifurcation level might cause victim’s death, although we compress the neck to expect decreasing heart rate in a patient with paroxysmal supraventricular tachycardia (PSVT).
3.4. The Posterior Communicating Artery in the Willis Circle
In our study, there were 57.4% normal type, 13.0% hypoplastic type, 22.2% fetal type and absence 1.9%, and others 5.6% [8].
We experience two strangulation cases.
3.4.1. A Murdered Female without Facial Congestion and Petechiae in the Conjunctiva
A 65-year-old woman was murdered by her daughter with manual strangulation, after her death the daughter called police. She had no facial congestion and petechiae in the conjunctiva. Autopsy revealed severe bleeding in the neck and the tongue. Both side posteriol communi-
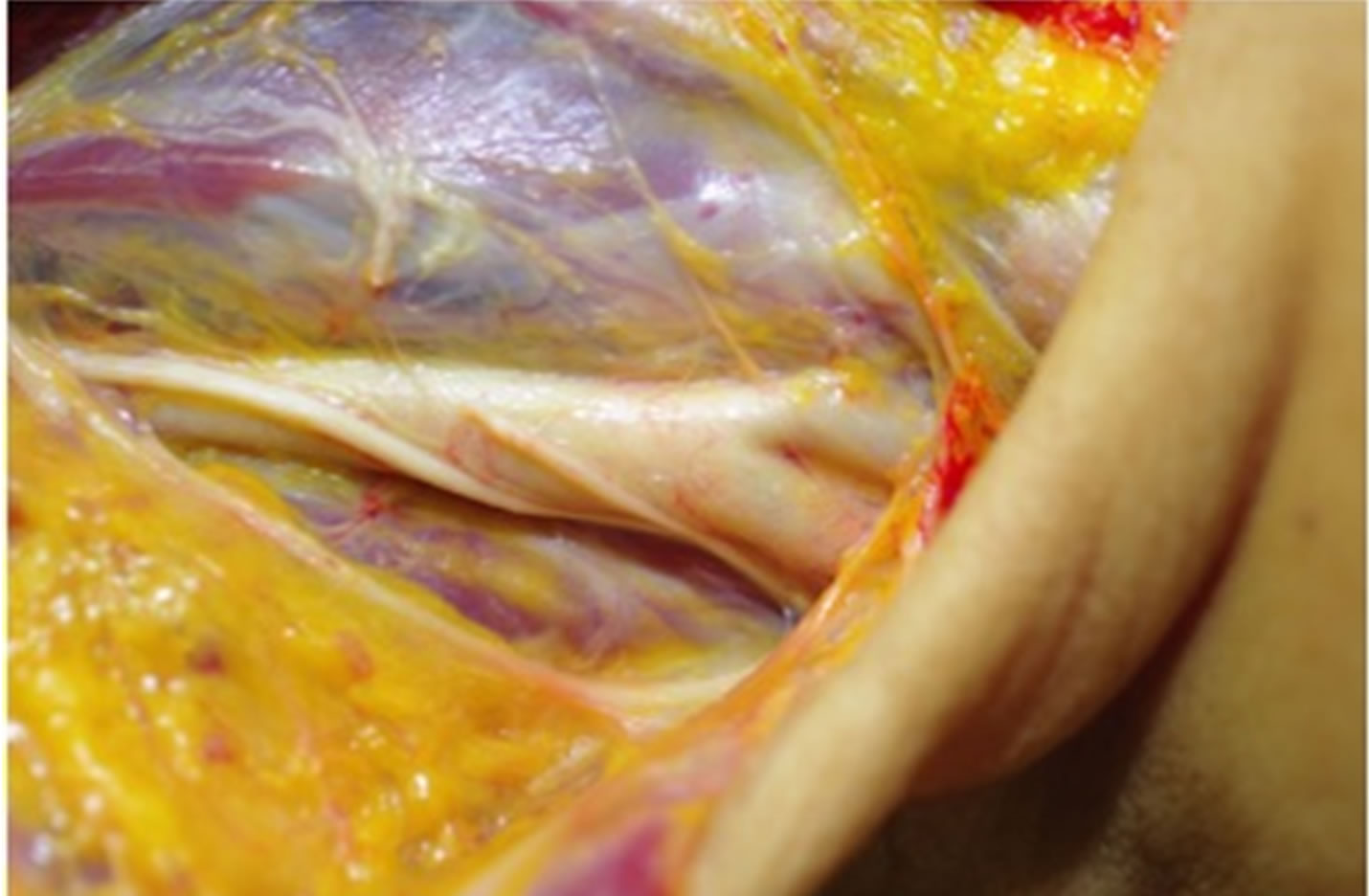
Figure 4. Case A-2-2. The left side internal jugular vein lays inside the carotid artery.
 (a)
(a) (b)
(b)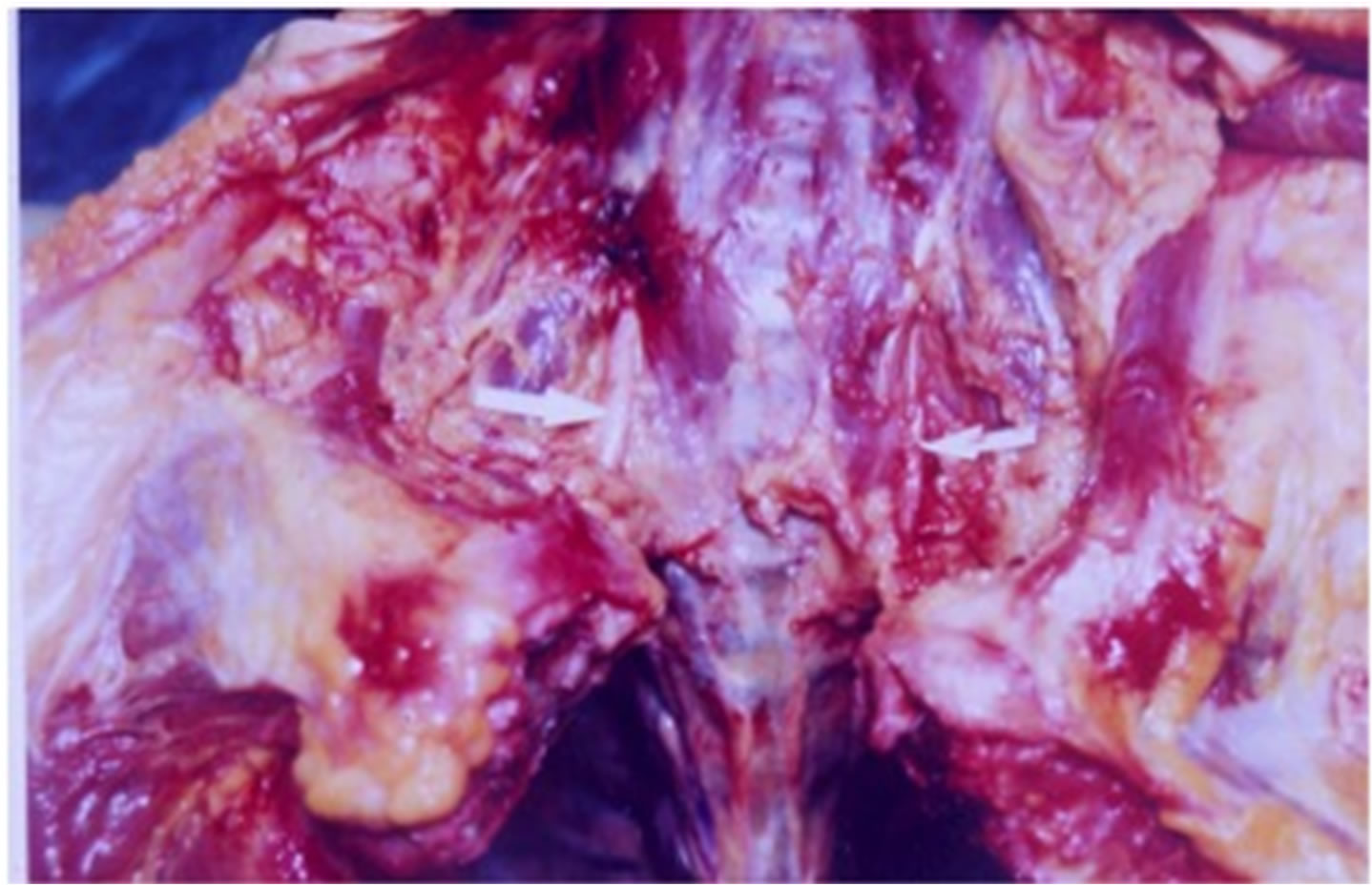 (c)
(c)
Figure 5. Case B-1. An old lady was found death in situation her neck being sandwiched between protective fence of her bed (a). No-petechiae in her conjunctiva (b) and bleeding were detected at C6 level (c).

Figure 6. Bifurcation of carotid artery. Both side bifurcation of the carotid arteries were observed at the level C2 from an individual.

Table 1. Distribution of level of the bifurcation of common carotid artery.
cating arteries were defect (Figure 7). In this case, the bleeding of the neck tissue was detected at lower level of the bifurcation of the carotid artery.
3.4.2. A Man Die Due to Atypical Hanging and with Severe Bleeding and Petechiae Only in One Side Eye
A 67-year-old man died due to atypical hanging, sitting position, showed severer bleeding in his right side eye compared with his left eye (Figure 8(a)).
Autopsy revealed that he had only right communicating artery of the Willis circle (Figure 8(b)).
4. DISCUSSION
Although we have been observing the internal jugular veins, vertebral arteries and the Willis circles as a routine performance at Department of Legal Medicine, Shiga University of Medical Science [2-6], there are many studies concerning variations in the literatures [7,9].
Clinical study is the main object and subject of their study. The relational study between variation of the vessels and forensic pathological finding was not common.
4.1. The Jugular Vein
Previous report revealed that the external jugular veins also have valves. Internal jugular vein valves combined with jugular vein valves seems to play an important role to prevent the backward blood-flow from the heart.
Fisher et al. revealed that patient with normal central venous pressure had competent valves during coughinduced transvalvular pressure gradients of 52.4 ± 8.6 mmHg (9). Two autopsy cases showed the different finding on the faces, that is, a woman had bleeding in the conjunctiva, the scalp and the tongue, the other hand showed no bleeding in these tissues, although their postmortem posture were almost the same. These differ-
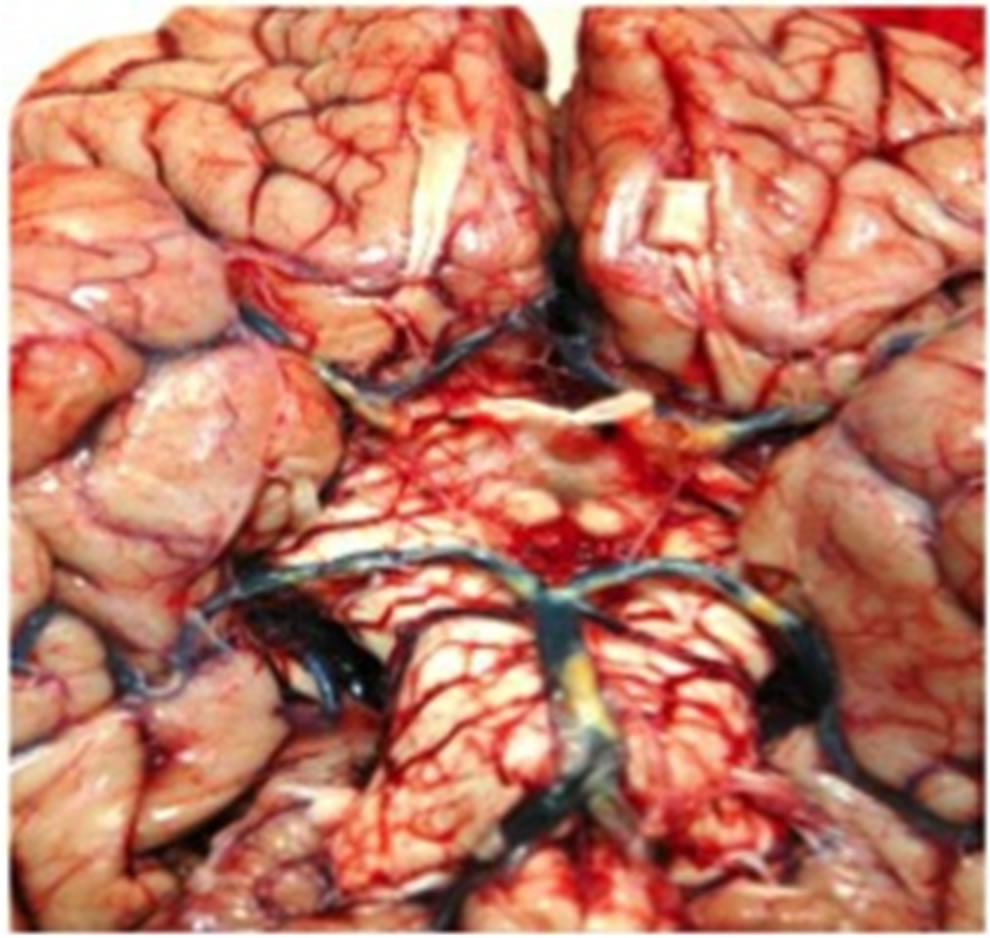
Figure 7. Case D-1. A murder case by manual strangulation. A 65-year-old woman was murdered by her daughter with manual strangulation, however she had no facial congestion and petechiae in the conjunctiva. Autopsy revealed defecting of both side posterior communicating arteries.
 (a)
(a)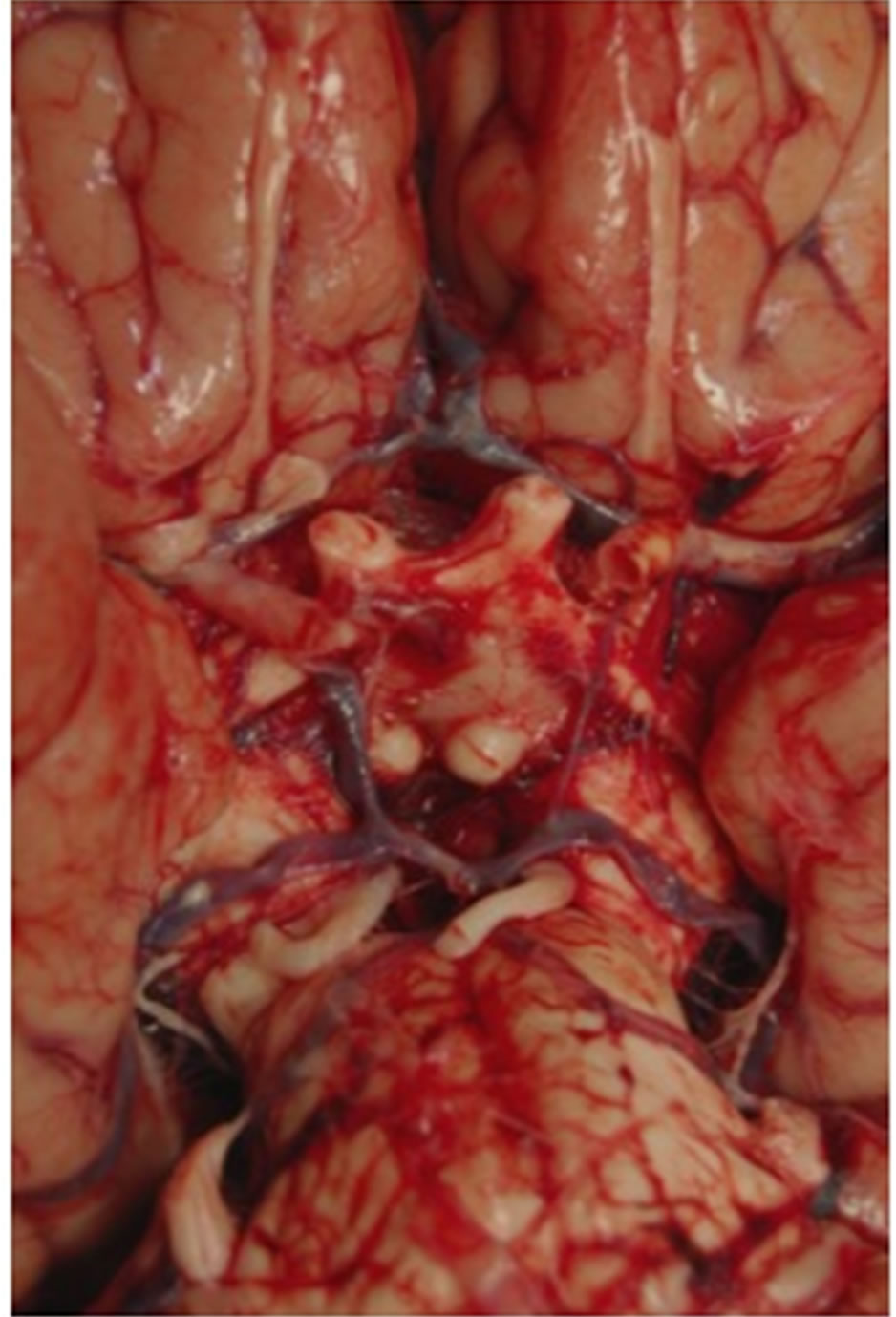 (b)
(b)
Figure 8. Case D-2. Atypical hanging case with severe bleeding in one side conjunctiva. A 67-year-old male died due to atypical hanging showed severer bleeding in his right side eye compared with his left eye (a). Autopsy revealed that he had only right communicating artery of the Willis circle (b).
ence seems to be caused by the efficiency of jugular venous valves to protect the backward blood flow from the heart. The efficiency of the valves in the internal and external jugular veins may be inducible to the death in positional asphyxia and head-down tile since the backward flow through veins causes congestion of blood stream and then brings about consumption of oxygen and ATP in the brain.
The right internal jugular vein is a common vessel to obtain venous access. It is important to have a clear understanding of the anatomy of the internal jugular vein and its relationship to the common carotid arteries to avoid inadvertent arterial puncture. We examined one autopsy case (Case A-2-2.) where left side internal jugular vein lays the inside of left common carotid artery. This case seems to be extremely rare.
4.2. The Vertebral Artery
The vertebral artery arises from the superior aspect of the subclavian artery, passes through the foramina of all cervical transverse processes except the seventh, curves medially behind the lateral mass of atlas, and then enters the cranium via the foramen magnum. At the lower pontine border, it joins its fellow to form the basilar artery. Occasionally, it may enter the bone at fifth, fourth, or seventh cervical transverse foramen. In approximately 60% cases, the arteries are unequal in size. The left vertebral artery is often larger in size than the right [10]. In a study by Bruneau et al., out of 500 vertebral arteries studied, they observed an abnormal level of entrance into foramentransversarium in 7% specimens (35 cases), with a level of entrance into the C3, C4, C5, or C7 foramen transversarium respectively in 0.2%, 1.0%, 5.0% and 0.8% of all specimens [11]. Seventeen abnormalities were right sided and 18 were left sided. Thirty-one out of 250 patients had a unilateral anomaly and two had a bilateral anomaly.
Autopsy cases presented in this study indicate that it is necessary to be careful not to overlook strangulation in patients without petechiae of the conjunctiva due to absence or hypoplastic type of posterior communicating artery and lower level strangulation or compression in forensic autopsy cases. The compression with around 5 or 7 kg to the lower neck can obstruct the common carotid and vertebral artery [12].
4.3. Carotid Artery Bifurcation
It is commonly accepted that the carotid artery bifurcation occurs about the level of C 4 [13] and carotid sinus exist on the part of the bifurcation [14].
Schrag et al. conducted a research concerning the opinion of forensic medical experts, but the cardioinhibitory reflex and described that 80.2% of experts believe that the cardioinhibitory reflex can theoretically cause death [15].
Forensic pathological evaluation of the cardioinhibitory reflex is still controversial. Whether the reflex is true or not, we should know existence of the variation of bifurcation, and that racial and ethical difference was also reported. Osborn showed that the normal common carotid artery bifurcation is at or near the level of the thyroid cartilage (approximately C4), but bifurcation may occur as high as C1 or as low as T2 [16]. Indeed several reports were made from Africa or Arab [17-19].
Although argument between the vagal reflex and neck compression is still unsolved, the reflex due to the compression of the carotid sinus is now out of thinkable, since it is clear that distribution of the bifurcation is so wide.
4.4. The Posterior Communicating Artery in the Willis Circle The existence of circle of Willis was described in 1664 by Thomas Willis [20], although innumerous anatomical variations are known. We encountered interesting autopsy cases where the variations of the Willis circle, especially posterior communicating artery, caused unexpected forensic pathological findings. In these cases, the blood supply to the ocular and orbital arteries that are tributaries of the internal cervical artery might be defective. In D-1 case, the cardioinhibitory death due to the compression of bifurcation was denied, since the bleeding part was identified at lower part of the bifurcation. Forensic pathologist should be careful not to overlook strangulation in patients without petechiae of the conjunctiva due to absence orhypoplastic type of posterior communicating artery.
5. CONCLUSIONS
This study showed that various variations exist in the cranio-cervical blood vessels. In some cases a victim seems to be a murdered body. Forensic pathologists should understand the relationship between the findings and physiological blood stream, and recognize that the unexpected findings might be caused by anatomical variations.
It is necessary to be careful not to overlook strangulation in patients without petechiae of the conjunctiva due to absence or hypoplastic type of posterior communicating artery and lower level strangulation or compression in forensic autopsy cases.
6. ACKNOWLEDGEMENTS
The Ethics Committee of the Shiga University of Medical Science approved this article. We thank Shiga University of Medical Science for supporting this article and giving permission to publish the article.
REFERENCES
- Nishi, K., Nakagawa, T., Yamamoto, A., Yamasaki, S., Morimoto, A., Yamamoto, Y., Morita, S., Kobayashi, A. and Takase, I. (2005) Is differential diagnosis of hemorrhages in the face and head in post-mortem and those in life possible? Japanese Journal of Forensic Medicine and Pathology, 11, 87-92 (In Japanese).
- Sanchez-Hanke, M., Pueschel, K. and Leuwer, R. (2000) Anatomy of the valve system of the internal jugular vein. Laryngorhinootologie, 79, 332-336 (in Germany with English Abstract).
- Morimoto, A., Takase, I., Shimizu, Y. and Nishi, K. (2009) Assessment of cervical venous blood flow and the craniocervical venous valve using ultrasound sonography. Legal Medicine (Tokyo), 11, 10-17. http://dx.doi.org/10.1016/j.legalmed.2008.07.006
- Furukawa, S., Nakagawa, T., Sakaguchi, I. and Nishi, K. (2010) The diameter of the internal jugular vein studied by autopsy. Romanian Journal of Legal Medicine, 18, 125-128.
- Furukawa, S., Takase, I., Nakagawa, T., Sakaguchi, I. and Nishi, K. (2011)Autopsic investigations of the morphological variations of the internal jugular valve. Indian Journal of Forensic Medicine & Toxicology, 5, 71-73.
- Furukawa, S., Wingenfeld, L., Takaya, A., Nakagawa, T., Sakaguchi, I. and Nishi, K. (2012) Morphological variation of the carotid artery bifurcation level. Forensic Research. http://www.omicsonline.org/scientific-reports/srep135.php
- Sanchez-Hanke, M., Pueschel, K. and Leuwer, R. (2000) Anatomy of the valve system of the internal jugular vein. Laryngorhinootologie, 79, 332-336 (in Germany with English Abstract).
- Fisher, J., Vaghaiwalla, F., Tsitlik, J., Levin, H., Brinker, J., Weisfeldt, M. and Yin, F. (1982) Determination and clinical significance if jugular venous valve competence. Circulation, 65, 188-196. http://dx.doi.org/10.1161/01.CIR.65.1.188
- Benter, T., Teichgraeber, U.K.M., Kluehs, L., Papadopoulos, S., Koehne, C.H., Felix, R. and Doerken, B. (2001) Anatomical variations in the internal jugular veins of cancer patients affecting central venous access. Ultraschall in der Medizin, 22, 23-26. http://dx.doi.org/10.1055/s-2001-11243
- Shoja, M.M., Tubbs, R.S., Khaki, A.A., Shokouhi, G., Farahani, R.M. and Moein, A. (2006) A rare variation of the vertebral artery. Folia Morphologica, 65, 167-170.
- Bruneau, M., Cornelius, J.F., Marneffe, V., Triffaux, M. and George, B. (2006) Anatomical variations of the V2 segment of the vertebral artery. Neurosurgery, 59, s20- s24. http://dx.doi.org/10.1227/01.NEU.0000219931.64378.B5
- Yamasaki, S., Takase, I., Takata, N. and Nishi, K. (2009) Measurement of force to obstruct the cervical arteries and distribution of tension exerted on a ligature in hanging. Legal Medicine (Tokyo), 11, 175-180. http://dx.doi.org/10.1016/j.legalmed.2009.03.007
- Vitek, J.J. and Reaves, P. (1973) Thoracic bifurcation of the common carotid artery. Neuroradiology, 5, 133-139. http://dx.doi.org/10.1007/BF00341527
- Doberentz, E., Schyma, C. and Madae, B. (2012) Histological examination of the carotid bifurcation in case of violence against the neck. Forensic Science International, 216, 135-140. http://dx.doi.org/10.1016/j.forsciint.2011.09.009
- Scharg, B., Mangin, P., Vaucher, P. and Bollmann, M.D. (2012) Death caused by cardioinhibitory reflex. What experts believe. The American Journal of Forensic Medicine and Pathology, 33, 8-12. http://dx.doi.org/10.1097/PAF.0b013e3181db7efd
- Osborn, A.G. (1999) Diagnostic cerebral angiography. 2nd Edition, Lippicott Williams & Wilkins, Philadelphia, 62-63.
- Anangwe, D., Saidi, H., Ogengo, J. and Awori, K.O. (2008) Anatomical variation of the carotid arteries in adult Kenians. East African Medical Journal, 85, 244-247. http://dx.doi.org/10.4314/eamj.v85i5.9619
- Al-Rafiah, A., El-Haggay, A.A., Aal, I.H.A. and Zaki, A.I. (2011) Anatomical study of the carotid bifurcation and origin variations of the ascending pharyngeal and superior thyroid arteries. Folia Morphologica, 70, 47-55.
- Koch, S., Nelson, D., Rundek, T., Mandrekar, J. and Rabinstein, A. (2009) Race-ethnic variation in carotid bifurcation geometry. Journal of Stroke and Cerebrovascular Diseases, 18, 349-358. http://dx.doi.org/10.1016/j.jstrokecerebrovasdis.2009.01.002
- Dewhurst, K. (1972) Some letters to Dr. Thomas Willis. Medical History, 16, 63-76. http://dx.doi.org/10.1017/S0025727300017269

