Surgical Science
Vol.06 No.12(2015), Article ID:62285,6 pages
10.4236/ss.2015.612078
Parosteal Lipoma of Femur―A Case Report
Yogesh S. Salphale*, Prakash Lalwani, Wasudeo M. Gadegone, Ajay Mehra, Ravi Alurwar
Department of Orthopaedic & Traumatology, Chandrapur Multispeciality Hospital, Chandrapur, India

Copyright © 2015 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



Received 16 November 2015; accepted 25 December 2015; published 28 December 2015
ABSTRACT
A case of 16 yrs male patient with parosteal lipoma affecting the lower metaphyseal end of the left femur is presented. Clinical suspicion, plain radiographs, CT (Plain and 3 D) as well as MRI suggested a diagnosis of parosteal lipoma. Lipomas may be defined as benign lesions of mature adipose tissue without evidence of cellular atypia [1] . Lipomas are the most common soft tissue lesions and surprisingly are among the rarest bone neoplasias. The most frequent complaints are a tumoral convexity presenting as a visible or palpable mass or a mild-intensity, dull pain. The parosteal type is a rare tumor accounting for 0.3% of all lipomas [2] and is usually asymptomatic. It is seen commonly affecting adults aged over 40 [3] . The present article describes a rare case of parosteal lipoma located in the femur, with extensive hyperostosis visible on plain xray and confirmed by imaging studies (CT and MRI). Unlike the parosteal lipomas reported in adults over 40 yrs in this case it presented in a much younger age group.
Keywords:
Parosteal Lipoma, Nonpulsatile Mass, Tumoral Mass

1. Case Report
A 16 year-old male patient noticed an increase in the volume of his Left thigh with dull aching pain, approximately 2 years ago. The symptoms had increased since one month. The clinical evaluation revealed a nonpulsatile mass in the anteromedial face of the distal two-thirds of the left thigh that had a tender consistency and regular contour adhered to the deeper planes. It was painless upon diffuse palpation. The patella was shifted laterally due to the tumoral extension.
Conventional radiographs of the left thigh showed the presence of a spiculated periosteal bone formation in the antero medial face of the distal region of the femur and an increase in the amount of soft tissue with a radio density characteristic of fatty tissue (radiolucent image) (Figure 1) [4] -[6] .
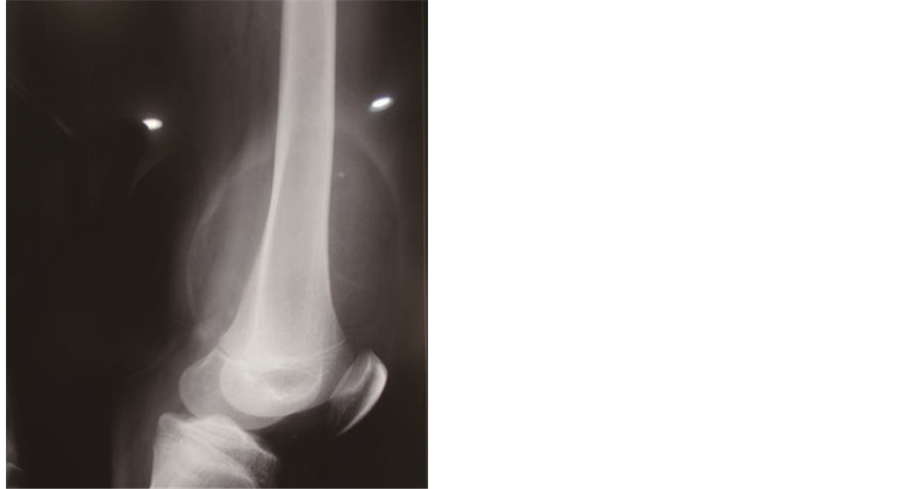
Figure 1. (a) and (b) showing increased perisoteal reaction associated with an increase of adjacent radioluscent soft parts.
Computed tomography of the left thigh showed a heterogeneous calcification image in the periosteal topography located in the medial region of the distal third of the femur in the meta-diaphyseal junction. There was no evidence of cortical discontinuity or bone marrow invasion. The lipoma was seen displacing the fat planes, and abutting the synovium of the knee joint. The patello femoral joint, as a result, showed widening. In the muscular plane, the density was similar to that of subcutaneous tissue in the intermediate vastus muscle topography, suggesting fat replacement (Figure 2, Figure 3).
To characterize the lesion and define the compression of adjacent neurovascular bundle, magnetic resonance imaging (MRI) was performed [7] . It revealed a well-defined, multilobulated, and juxtacortical bony excrescence measuring 8 × 4.7 cm in size at the lower end of the left femur. It had no contiguity with marrow space of the distal femur differentiating it from an osteochondroma. There was mild enhancement of interface between the bony protuberance and the lipid component of the lesion suggesting the fibrous tissue rim. There were no findings of neurovascular bundle compression. The diagnosis of parosteal lipoma with bony excrescence was made [8] [9] .
During the surgery, it was confirmed that the lesion had adhered to the femur in the region of the hyperostosis (periosteal reaction) (Figure 4).
The tumor specimen weighed 500 g and had a lobulated appearance, with an intact, thin, and translucent pseudocapsule (Figure 5).
Microscopic examination showed that the neoplasia was adhered to the strip of skeletal muscular tissue in its most superficial portion by fibrous tissue, with mature bone metaplasia in the deep portion with no evidence of malignancy. The results showed a lipoma with periosteal reaction.
After 15 months follow up the patient had no complaints and had normal range of movements at the knee.
2. Discussion
Osseous lipomas have been classified according to their site of origin: either within bone (intraosseus) or on its surface (juxtacortical). Surface osseous lipomas can be classified into parosteal and subparosteal lipomas [2] . The most frequently affected sites are the diaphysis [3] and metaphyseal regions of long bones The Parosteal lipomas often has a tendency to induce a periosteal reaction [1] [10] .
Parosteal lipomas are known to cause pressure effects especially nerve compression. These parosteal lipomas by virtue of their anchoring effect of the attachment site at the bone may predispose to mass effect and nerve
Figure 2. CT scan images showing the lipoma was seen displacing the fat planes, and abutting the synovium of the knee joint.
impingement which is in contrast to the soft tissue lipomas, which expand along the path of least resistance [11] .
The bone may be normal inspite of the close relationship of lipoma with the periosteum [12] [13] , but reactive changes in the adjacent bone [14] such as bone deformity, cortical erosion, and bony hyperostosis [15] [16] had been detected. More than half of parosteal lipomas presenting bone reactions are associated with hyperostosis [13] [17] .
It is assumed that cortical hyperostosis can be explained by the contact of the lipoma with the bone [12] [18] . A possibility which could be caused by stimulation or irritation of the periosteum [19] . In this case there was a distinct periosteal reaction. The reason why some lipomas located near the periosteum cause cortical hyperostosis
Figure 3. MRI Images showing the tumoral mass and the dilineation.
Figure 4. Showing the intraoperative photograph of the lesion adhering to the lower end of the femur.
Figure 5. Showing the excised tumor specimen.
while others fails to display the same is still unclear [18] . However, the amount of cortical hyperostosis can vary from a small area of the thickened cortical to exuberant exostoses [13] [14] .
Prominent hyperostosis promotes a typical appearance that, when combined the radiolucence of the soft parts of the tumor, has been described as pathognomonic for parosteal lipoma [19] -[21] .
Conventional radiographic exams showed an increase in the extra-bone soft tissues and formation of bone spicula over the periosteum. The radiodensity of the tumoral mass in conventional radiographs, which was consistent with fatty tissue, suggested the diagnosis in our case.
Grecco et al. in their series of 15 cases stressed the use of Computed tomography which characterizes degree of septation and defines relationship of mass with underlying cortex which is important for surgical planning.
The prognosis is usually favorable, with no proven reports of malignancy or recurrence and with full recovery of the patient [2] .
3. Conclusion
It is essential to resort to computed tomography and MRI to help with the diagnosis and therapeutic planning. We agree that resecting the lipomatous tumor [19] [22] [23] with further exeresis of the bone and periosteal excrescence in cases with hyperostosis [2] [12] should be performed.
Cite this paper
Yogesh S.Salphale,PrakashLalwani,Wasudeo M.Gadegone,AjayMehra,RaviAlurwar, (2015) Parosteal Lipoma of Femur—A Case Report. Surgical Science,06,549-554. doi: 10.4236/ss.2015.612078
References
- 1. Enneking, W.F. (1983) Limb Salvage in Musculoskeletal Oncology. Vol. 2. Churchill Livingstone, New York, 1225-1269.
- 2. Kapukaia, A., Subas, M., Dabak, N. and Ozkul, E. (2006) Osseous Lipoma: Eleven New Cases and Review of the Literature. Acta Orthopaedica Belgica, 72, 603-614.
- 3. Miller, M.D., Ragsdale, B.D. and Sweet, D.E. (1992) Parosteal Lipomas: A New Perspective. Pathology, 24, 132-139.
http://dx.doi.org/10.3109/00313029209063160 - 4. Kenin, A., Levine, J. and Spinner, M. (1959) Parosteal Lipoma. A Case Report of Two Cases with Associated Bone Changes. Journal of Bone and Joint Surgery, 41, 1122-1126.
- 5. Smith, T. (1866) Specimen of Firm Bilobed Fatty Tumor, Weighing 10 Ounces, Removed from Little Girl Age 5 Years. Transactions of the Pathological Society of London, 17, 286.
- 6. Power, D.A. (1888) Parosteal Lipoma, or Congenital Fatty Tumour, Connected with Periosteum of Femur. Transactions of the Pathological Society of London, 39, 270-272.
- 7. Yu, J.S., Weis, L. and Becker, W. (2000) MR Imaging of a Parosteal Lipoma. Clinical Imaging, 24, 15-18.
http://dx.doi.org/10.1016/S0899-7071(00)00156-X - 8. Kim, J.Y., Jung, S.L., Park, Y.H., Park, S.H. and Kang, Y.K. (1999) Parosteal Lipoma with Hyperostosis. European Radiology, 9, 1810-1812.
http://dx.doi.org/10.1007/s003300050927 - 9. Blair, T.R. and Resnick, D. (2000) Subperiosteal Lipoma: A Case Report. Clinical Imaging, 24, 381-383.
http://dx.doi.org/10.1016/S0899-7071(01)00236-4 - 10. Greco, M., Mazzocchi, M., Ribuffo, D., Dessy, L.A. and Scuderi, N. (2013) Parosteal Lipoma: Report of 15 New Cases and a Review of the Literature. Annali Italiani di Chirurgia, 84, 229-236.
- 11. Rich, P.J. and King III, W. (1982) Benign Cortical Hyperostosis Underlying Soft Tissue Tumors of the Thigh. American Journal of Roentgenology, 138, 419-422.
http://dx.doi.org/10.2214/ajr.138.3.419 - 12. Balani, A., Sankhe, A., Dedhia, T., Bhuta, M., Lakhotia, N. and Yeshwante, J. (2014) Lump on Back: A Rare Case of Parosteal Lipoma of Scapula. Case Reports in Radiology, 2014, Article ID: 169157.
http://dx.doi.org/10.1155/2014/169157 - 13. Fleming, R.J., Alpert, M. and Garcia, A. (1962) Parosteal Lipoma. American Journal of Roentgenology, 87, 1075-1084.
- 14. Laorr, A. and Greeenpan, A. (1993) Parosteal Lipoma with Hyperostosis: Report of Two Pathologically Proven Cases Evaluated by Magnetic Resonance Imaging. Canadian Association of Radiologists Journal, 44, 285-290.
- 15. Asirvatham, R. and Linjawi, T. (1994) Ossifying Parosteal Lipoma with Exuberant Cortical Reaction. International Orthopaedics, 18, 55-56.
http://dx.doi.org/10.1007/bf00180182 - 16. Rosenberg, A.E. and Bridge, J.A. (2002) Lipoma of Bone. In: Fletcher, C.D.M., Unni, K.K., Mertens, F., Eds., Pathology and Genetics of Tumours of the Soft Tissues and Bones, IARC Press, Lyon, 328-329.
- 17. Goldman, A.B., Di Carlo, E.F. and Marcove, R.C. (1993) Case Report 774: Coincidental Parosteal Lipoma with Osseous Excrescence and Intramuscular Lipoma. Skeletal Radiology, 22, 138-145.
http://dx.doi.org/10.1007/BF00197997 - 18. Jones, J.G., Habermann, E.T. and Dorfman, H.D. (1989) Case Report 553: Parosteal Ossifying Lipoma of Femur. Skeletal Radiology, 18, 537-540.
http://dx.doi.org/10.1007/BF00351757 - 19. Jacobs, P. (1972) Parosteal Lipoma with Hyperostosis. Clinical Radiology, 23, 196-198.
http://dx.doi.org/10.1016/S0009-9260(72)80095-3 - 20. Rodriguez-Peralto, J.L., Lopez-Barea, F., Gonzales-Lopes, J. and Lamas-Lorenzo, M. (1994) Case Report 821. Skeletal Radiology, 23, 67-69.
http://dx.doi.org/10.1007/BF00203707 - 21. Bridge, J.A., De Boer, J., Walker, C.W. and Neff, J.R. (1995) Translocation t(3;12)(q28;q14) in Parosteal Lipoma. Genes, Chromosomes and Cancer, 12, 70-72.
http://dx.doi.org/10.1002/gcc.2870120113 - 22. Kubo, T., Matsui, Y., Goto, T., Yukata, K., Endo, K., Sato, R., et al. (2006) MRI Characteristics of Parosteal Lipoma Associated with the HMGA2-LPP Fusion Gene. Anticancer Research, 26, 2253-2258.
- 23. Kawashima, A., Magid, D., Fishman, E.K., Hruban, R.H. and Ney, D.R. (1993) Parosteal Ossifying Lipoma: CT and MR Findings. Journal of Computer Assisted Tomography, 17, 147-150.
http://dx.doi.org/10.1097/00004728-199301000-00029
NOTES
*Corresponding author.







