Successful Treatment of Spine Fracture for Diffuse Idiopathic Skeletal Hyperostosis with
Teriparatide—A Report of Two Cases 281
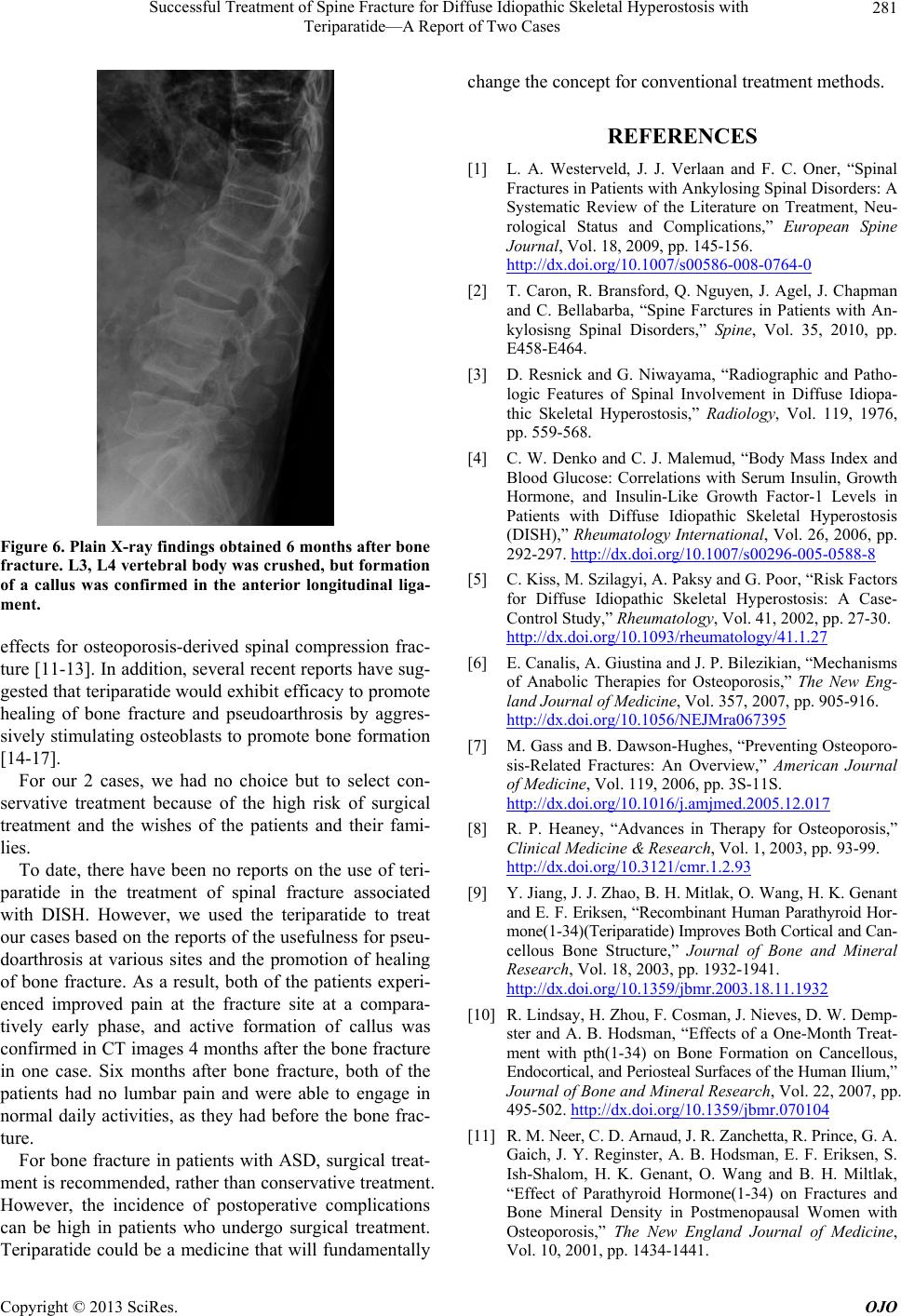
Figure 6. Plain X-ray findings obtained 6 months after bone
fracture. L3, L4 vertebral body was crushed, but formation
of a callus was confirmed in the anterior longitudinal liga-
ment.
effects for osteoporosis-derived spinal compression frac-
ture [11-13]. In addition, several recent reports have sug-
gested that teriparatide would exhibit efficacy to promote
healing of bone fracture and pseudoarthrosis by aggres-
sively stimulating osteoblasts to promote bone formation
[14-17].
For our 2 cases, we had no choice but to select con-
servative treatment because of the high risk of surgical
treatment and the wishes of the patients and their fami-
lies.
To date, there have been no reports on the use of teri-
paratide in the treatment of spinal fracture associated
with DISH. However, we used the teriparatide to treat
our cases based on the reports of the usefulness for pseu-
doarthrosis at various sites and the promotion of healing
of bone fracture. As a result, both of the patients experi-
enced improved pain at the fracture site at a compara-
tively early phase, and active formation of callus was
confirmed in CT images 4 months after the bone fracture
in one case. Six months after bone fracture, both of the
patients had no lumbar pain and were able to engage in
normal daily activities, as they had before the bone frac-
ture.
For bone fracture in patients with ASD, surgical treat-
ment is recommended, rather than conservative treatment.
However, the incidence of postoperative complications
can be high in patients who undergo surgical treatment.
Teriparatide could be a medicine that will fundamentally
change the concept for conventional treatment methods.
REFERENCES
[1] L. A. Westerveld, J. J. Verlaan and F. C. Oner, “Spinal
Fractures in Patients with Ankylosing Spinal Disorders: A
Systematic Review of the Literature on Treatment, Neu-
rological Status and Complications,” European Spine
Journal, Vol. 18, 2009, pp. 145-156.
http://dx.doi.org/10.1007/s00586-008-0764-0
[2] T. Caron, R. Bransford, Q. Nguyen, J. Agel, J. Chapman
and C. Bellabarba, “Spine Farctures in Patients with An-
kylosisng Spinal Disorders,” Spine, Vol. 35, 2010, pp.
E458-E464.
[3] D. Resnick and G. Niwayama, “Radiographic and Patho-
logic Features of Spinal Involvement in Diffuse Idiopa-
thic Skeletal Hyperostosis,” Radiology, Vol. 119, 1976,
pp. 559-568.
[4] C. W. Denko and C. J. Malemud, “Body Mass Index and
Blood Glucose: Correlations with Serum Insulin, Growth
Hormone, and Insulin-Like Growth Factor-1 Levels in
Patients with Diffuse Idiopathic Skeletal Hyperostosis
(DISH),” Rheumatology International, Vol. 26, 2006, pp.
292-297. http://dx.doi.org/10.1007/s00296-005-0588-8
[5] C. Kiss, M. Szilagyi, A. Paksy and G. Poor, “Risk Factors
for Diffuse Idiopathic Skeletal Hyperostosis: A Case-
Control Study,” Rheumatology, Vol. 41, 2002, pp. 27-30.
http://dx.doi.org/10.1093/rheumatology/41.1.27
[6] E. Canalis, A. Giustina and J. P. Bilezikian, “Mechanisms
of Anabolic Therapies for Osteoporosis,” The New Eng-
land Journal of Medicine, Vol. 357, 2007, pp. 905-916.
http://dx.doi.org/10.1056/NEJMra067395
[7] M. Gass and B. Dawson-Hughes, “Preventing Osteoporo-
sis-Related Fractures: An Overview,” American Journal
of Medici ne, Vol. 119, 2006, pp. 3S-11S.
http://dx.doi.org/10.1016/j.amjmed.2005.12.017
[8] R. P. Heaney, “Advances in Therapy for Osteoporosis,”
Clinical Medicine & Research, Vol. 1, 2003, pp. 93-99.
http://dx.doi.org/10.3121/cmr.1.2.93
[9] Y. Jiang, J. J. Zhao, B. H. Mitlak, O. Wang, H. K. Genant
and E. F. Eriksen, “Recombinant Huma n Parathyroid Hor-
mone(1-34)(Teriparatide) Improves Both Cortical and Can-
cellous Bone Structure,” Journal of Bone and Mineral
Research, Vol. 18, 2003, pp. 1932-1941.
http://dx.doi.org/10.1359/jbmr.2003.18.11.1932
[10] R. Lindsay, H. Zhou, F. Cosman, J. Nieves, D. W. Demp-
ster and A. B. Hodsman, “Effects of a One-Month Treat-
ment with pth(1-34) on Bone Formation on Cancellous,
Endocortical, and Periosteal Surfaces of the Human Ilium,”
Journal of Bone and Mineral Research, Vol. 22, 2007, pp.
495-502. http://dx.doi.org/10.1359/jbmr.070104
[11] R. M. Neer, C. D. Arnaud, J. R. Za nchetta, R. Prince, G. A.
Gaich, J. Y. Reginster, A. B. Hodsman, E. F. Eriksen, S.
Ish-Shalom, H. K. Genant, O. Wang and B. H. Miltlak,
“Effect of Parathyroid Hormone(1-34) on Fractures and
Bone Mineral Density in Postmenopausal Women with
Osteoporosis,” The New England Journal of Medicine,
Vol. 10, 2001, pp. 1434-1441.
Copyright © 2013 SciRes. OJO