Open Journal of Nursing
Vol.3 No.8A(2013), Article ID:41032,8 pages DOI:10.4236/ojn.2013.38A003
Identify gaps between local and international measures to avoid administration error on 1-year review in United Christian Hospital, Hong Kong
![]()
United Christian Hospital, Kwun Tong, Hong Kong, China
Email: tsanlf1@ha.org.hk
Copyright © 2013 Lap Fung Tsang. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received 24 August 2013; revised 24 September 2013; accepted 15 October 2013
Keywords: Medication Administration Errors; Contributory Factors; Preventive Measures; Gap Review
ABSTRACT
Many medication errors could be avoided if administration was more closely linked with structured monitoring. The contributory factors to administration errors occurred in one recent year were reviewed and identified contributory factors to errors as six domains of administration principles according to the report from the Quality and Safety website. The current measures including guidelines, policy, and practices to prevent the administration errors identified in the previous step were searched from the United Christian Hospital (UCH) homepage. Meanwhile, the international measures suggested in literature were identified to address the administration errors identified. 41 cases were identified as medication errors related to administration error events, with total twenty contributory factors identified according to the incident report which identified five contributory factors as common causes. Measures to prevent interruption of medication round and measures to improve individual knowledge and skills, and personal responsebility were suggested to fill the gaps. The medication administration errors should be avoided through both education reinforcing programme and preventive interventions of distraction or interruption to the procedure after comparing the existing measures to the suggested measures from literature. This study was so important to improve the current measures to prevent medication administration errors.
1. INTRODUCTION
Medication error events can occur at any phase of the complex medication process including prescription, transcribing, dispensing, and administration. This problematic area has received considerable attention among healthcare professions because of its potential mortality, morbidity, and additional health care costs. Prevention of medication errors is an important topic frequently discussed and addressed in clinical settings.
The Swiss Cheese model “Figure 1”, which has gained widespread acceptance and use in healthcare, indicated how errors occur when several safety nets fail and each layer of the safety gate is not strictly applied [1]. It alerts administrators to safeguard the medication administration from malpractices. Indeed, medication administration errors can occur at any stage of the medication administration process if nurses fail to implement the relevant measures. For example, a medication error will ensue if the medicine is reconstituted incorrectly or the intravenous rate is set inappropriately either manually or mechanically, although each nurse may have correctly identified the patient, dose, time, route, and drug. The model shows that no matter how many measures are implemented, medication administration error can result from various contributory factors.
The Hospital Authority (HA) in Hong Kong has introduced and established the Advanced Incidents Reporting System (AIRS). This system requires that each of the Kowloon East Cluster hospitals should set up its own set of procedures or operation manual to document the flow of reporting to top management for critical incidents. Any significant incident must be reported through the AIRS system so that a variety of measures can be implemented and the reported incident can be shared and learned from after the root cause analysis has been performed for risk identification. Medication error events are continually ranked as either the first or second most frequent risk among Serious Untoward Events (SUE). In-depth analysis of these medication error events often

Figure 1. Swiss Cheese Model to explain medication administration error in various preventive measures.
places prescription error as the top risk, followed by administration and dispensing errors in priority in recent years. Administration error is the one that is most likely to fall within the scope of nurses but this does not mean that other types of medication error are not significant. Nurses are subject to a range of practices and procedures, which are dictated through legal, management and medical requirements to ensure safe medication administration [2].
Many medication errors could be avoided if administration was more closely linked with structured monitoring. Incident review is one of the important processes to facilitate changes and improvements in healthcare system. Forty-one cases of the incident review were identified as medication error related to administration error events. This paper aims to identify the measures addressing the various contributory factors to medication administration errors in United Christian Hospital (UCH), a district hospital in Hong Kong. Secondly, it aims to utilize the findings of the review process to give some ideas of what other measures can be further reinforced to promote in UCH with reference to international evidence-based measures.
2. METHOD
The review paper made use of existing data and relevant literature. The initial review was to identify the contributory factors to errors in six domains of administration principles from the report of administration incidents of medication in UCH. Administration errors recorded in one recent year (between September 2011 and September 2012) were reviewed according to the report from the Quality and Safety website. Factors contributing to administration errors were then identified and categorized into several domains. Current measures, including guidelines, policy, and practices to prevent medication administration errors, were identified from the UCH homepage based on the contributory factors. Meanwhile, measures suggested in the international literature for prevention of medication errors were identified. Lastly, recommendations were suggested to identify the gaps between the local practices and the international findings so as to further improve our existing measures.
3. RESULT
3.1. Review of One Recent Year’s Medication Administration Errors Related to Nurses
To delineate and understand further the factors involved in medication administration errors, the UCH Quality and Safety (Q&S) is responsible to analyze reports made to centralized reporting systems for sharing in a developed website. According to the information from the website, each report summarized and identified the incident as relating to various contributory factors, and action plans were suggested for further improvement accordingly. This paper used existing incident reports to determine the occurrence of medication administration errors related to nurses from September 2011 to September 2012, and to analyze the data to categorize errors in six associated domains: 1) right patient; 2) right drug; 3) right route; 4) right dose; 5) right frequency; and 6) others. These categories were based on HA guidelines on medication management which emphasize that nurses should always adopt the checking principle to achieve the “Five Rights”. That is the right drug in right dose must be delivered to the right patient by the right route at the right time. This principle should be maintained whenever the drug administration procedure is implemented. The category “others” was added to allow recording of factors outside these principles, such as allergy checking, interruption, complacency regarding common medications, failure to check previous history of receiving the medication and so on. A variety of contributory factors leading to administration error among six categories (known drug allergy, dangerous drugs, anti-coagulants, hypoglycemic agent, concentrated electrolytes, and other kinds of drug) were allocated to the six aforementioned domains associated with administration error.
In this search, 41 cases were identified as medication error related to administration error events, with a total of twenty contributory factors identified “Table 1”. Incidents related to “lack of checking allergy” accounted for 47.8 per cent (11/23) of cases in “known drug allergy” and also accounted for the commonest factor among six domains of error. Incidents related to “knowledge deficits” of “right drug” accounted for 26.1 per cent (6/23) of “known drug allergy”, 3.6 per cent (1/28) of “dangerous drugs”, and 5.3 per cent (1/19) of “other kinds of drug”. “Lack of independent counter-checking on medication” is regarded as the third common factor in
“right dose” of administration error. It accounted for 10.7 per cent (3/28) of “dangerous drugs”, 33.3 per cent (1/3) of “hypoglycemic agent” and 15.8 per cent (3/19) of “other kinds of drug”. “Look-alike-sound-alike” and “failure to spell medication name” were placed as the fourth contributory factors to cause medication administration error in “dangerous drugs”, “anti-coagulants”, and “other kinds of drug”. None of incidents were related to “right route” of administration error in this review.
3.2. Review the Local Practices, Policy, and Guideline to Address the Identified Factors in Administration
In the incident review mentioned above, “lack of checking allergy” in the “others” category, “knowledge deficits” in the “right drug” category, “lack of independent counter-checking on medication” in the “right dose” category, and “look-alike-sound-alike” and “failure to spell medication name” in the “right drug” category as the common factors in administration errors were identified. According to these factors, the existing hospital measures were reviewed to identify whether further measures needed to be improved in the UCH.
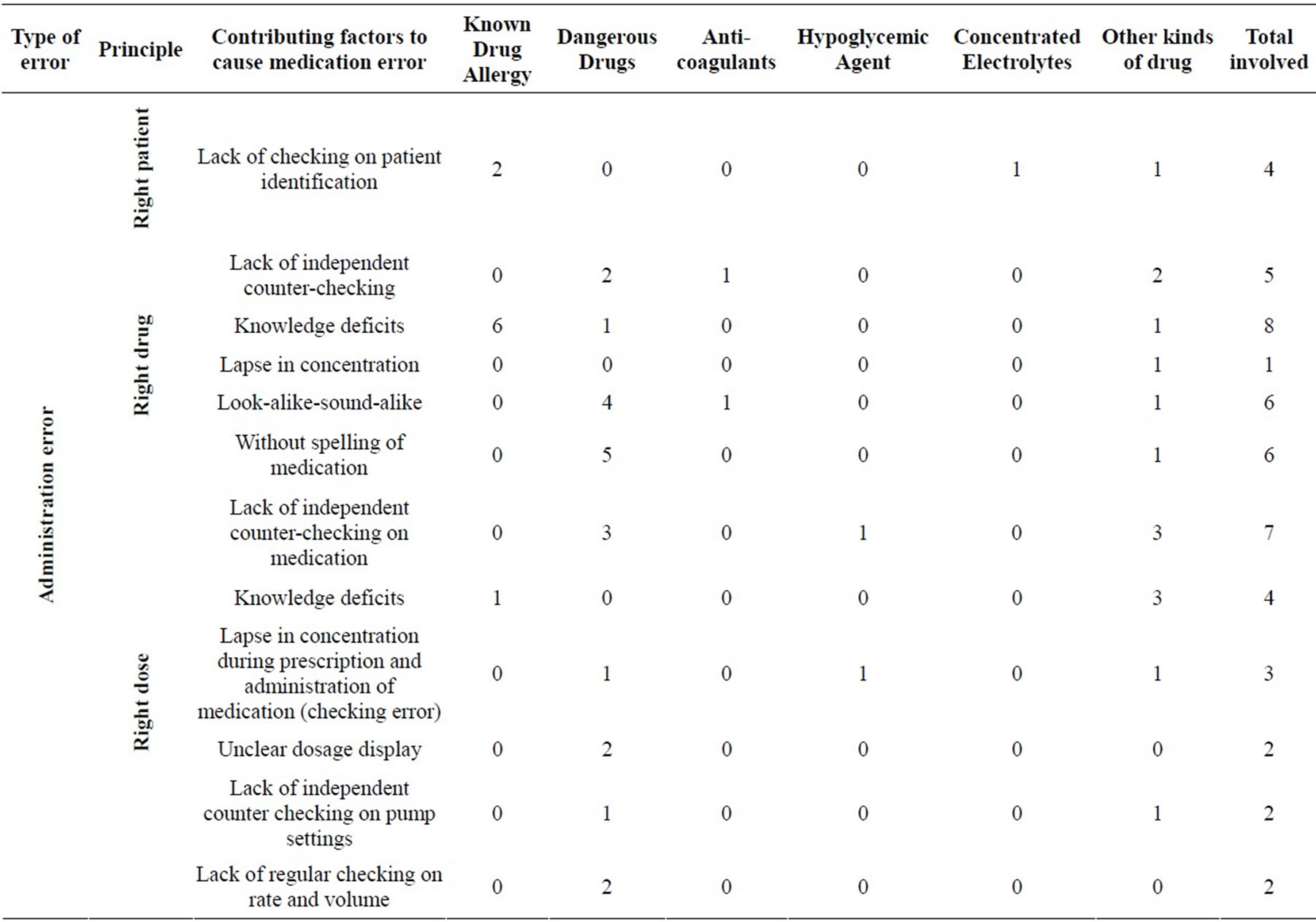
Table 1. Serious Untoward Event (SUE) from Sep 2011 to Sep 2012 (Medication error—administration) total 41 cases was reviewed.
3.2.1. “Lack of Checking Allergy” of Administration Error with “Known Drug Allergy”
In the HA Guidelines on Medication Management—Prescribing, Dispensing and Administration (Administration Guidelines) [3], a statement about “patient’s drug allergy status” is quoted and it indicates that this should be checked carefully before drug administration. In the selfassessment guide for medication safety—in public hospitals [4], several core characteristics of strategies are mandatory or recommended for nurses to comply with maintaining accurate and consistent allergy documentations to ensure patient safety and quality patient care. For instance• Medicines are not administered if the section for entering Drug Allergy information in the Medication Administration Record (MAR)/prescription is left blank (mandatory).
• Patients’ drug allergy status (prominent signs, colored record, drug allergy alert bands etc.) are made readily distinguishable and easily reviewed by doctors and nurses during drug prescribing and administration (recommended).
• For patients who have an allergy, ensure allergy alert wrist bands are worn. In settings where these allergy bracelets are not used, there is a drug allergy notification policy (recommended).
• Patients/carers are educated and instructed to share their drug allergy information with all their healthcare providers in all encounters to prevent recurrence of allergic drug reactions (recommended).
On the other hand, there is a guideline for handling problems with using the CMS drug allergy module to provide a safe and consistent method for handling dubious medication allergy history [4]. A sample of colored card attached to MAR, for ease of drug allergy identification, and a drug allergy reference chart depicting drugs of the same class for possible cross sensitivity considerations, are suggested in this guide. In UCH, different strategies according to the Self-Assessment Guide for Medication Safety (2005) are promulgated and implemented [4]. For example, the drug allergy reference card is prepared for staff to avoid possible cross-hypersensitivity [5]. For patients who have an allergy, allergy alert wrist bands are worn. The nurse should pre-print the patient’s CMS Allergy Alert sheet, if available, and file it in the patient’s record. A facsimile of the Medication Administration Record (MAR) used to be prescribed by doctors should be sent to the pharmacy for drug order verification.
3.2.2. “Knowledge Deficits” of Right Drugs with “Known Drug Allergy”
The qualified nurse should be competent to administer drug on his/her own. In UCH, different strategies according to the Self-Assessment Guide for Medication Safety (2005) [4] are promulgated and implemented to avoid possible cross-hypersensitivity. For example, the drug allergy reference card is prepared for staff to avoid possible cross-hypersensitivity [5]. The principle that the right drug in right dose is delivered to the right patient by the right route at the right time should be upheld. Qualified nurses should have the accountability to ensure the right drugs administering to right patients. There are different materials for references if nurses have any suspicion about the medication administration process.
3.2.3. “Lack of Independent Counter-Checking on Medication” of “Right Dose”
In the HA Guidelines on Medication Management—Prescribing, Dispensing and Administration (Administration Guidelines) [3], qualified nurses are advised to have the process counter-check by a second person especially for high alert drugs such as paediatric drugs, intravenous high alert drugs, dangerous drugs, cytotoxic drugs and drugs added to infusion fluids. Qualified nurses should exercise care to counter-check and not rely solely on others with regard to the checking process.
3.2.4. “Look-Alike-Sound-Alike” of Right Drug with “Dangerous Drugs”
HAHO Medication Safety Committee (2008) [6] has proposed that each individual hospital should devise strategies to reduce errors associated with look-alikesound-alike medications. For example, qualified nurses should clarify with the prescriber when medication orders are incomplete, illegible or unclear. They should check the diagnosis and appropriateness of dose prior to administering medications that have been identified to have the potential for mix-up due to look-alike names. UCH pharmacy emphasize the drug name differences by using “TALL man” lettering (writing the drug name in upper case letters) and color on labels of ward top-up stock bottles or highlight parts of the drug name that could cause confusion for selected look-alike drug name pairs [6].
3.2.5. “Failure to Spell Medication Name” of Right Drug with “Dangerous Drugs”
Spelling of the name of each medication is the basic practice to check the right medication in clinical areas. The label should be read carefully each time a medication is accessed and again prior to administration, rather than relying on visual recognition, location or other less specific cues [6].
3.3. Review the Contributory Factors in the Literature
Numerous factors have been identified in the literature as contributing to errors in the process for routine medication administration. They include mathematical skills, knowledge of medications, how clearly the prescription is written, length of experience, shift patterns, workload and staffing levels, medication delivery systems, single-nurse administration, policies and procedures and distractions and interruptions [7,8]. The synthesis of findings from three qualitative studies highlighted that there were external and internal factors that were perceived by nurses as contributing to medication administration errors [7]. External administration-related factors contributing to errors include use of policies, protocols and guidance, context and organisation of care and roles of people within the system. Interruptions to the medication round as an external factor contributing to errors should be minimized. Internal administration-related factors contributing to errors include interpersonal skills and relationships, individual knowledge and skills, personal responsibility in terms of tiredness, stress, lack of confidence in challenging doctors, concentration, complacency and even the personality of the nurse [7].
Referring to the external and internal factors, nurses would offer a valuable insight in explaining how the contributing factors in administration error can be used to analyze the organizational and personal contributions to such errors in UCH. In view of the existing measures in UCH, they can address the contributory factors instead of the internal and external factors. This may be a gap of the existing measures needed to be improved. Of the contributory factors identified in this review, “Knowledge deficits”, “failure to spell medication name”, “lack of independent counter-checking on medication” and “lack of checking allergy” in administration errors events in UCH were all identified as internal or person-centred factors merged into individual knowledge and skills, and personal responsibility whereas interruption was regarded as the external factor. Further measures are required to retrieve useful measures to avoid these factors from happening.
3.4. Review the Preventive Measures in the Literature
We attempted to identify all studies relevant to the review, written in English from the beginning of the year 2008 to the beginning of 2012 limiting the articles to those from peer-reviewed or research-based publications through searching in the e-Knowledge Gateway (eKG). The keywords “measure” or “intervention” combined with “interruption”, “administration error”, “individual knowledge and skills”, or “personal responsibility” were searched. The term “measure” or “intervention” was presented in every search. The reference list of all the studies identified by the above search strategy was checked. Relevant studies were read, and where appropriate, included in the review.
3.4.1. Measures to Decrease Interruptions of the Medication Round
From the identified 100 articles, 7 studies were considered relevant to this topic. From these, it was found that there were numerous external factors that make the busy ward environment conducive to error. Interruption is frequently highlighted in the literature as a causative factor. Interruption to the medication round is believed to be highly associated with administration errors and it can lead to raising internal factors in the process of administration [7]. Different characteristics of nurses’ work interruptions during medication administration have been reported in an observational study. In both the preparation phase and the administration phase, numbers of interruptions were found that related to missing medication or equipment, care coordination, self-initiation and patient care [9]. Another study concluded that the occurrence and frequency of interruptions were significantly associated with the incidence of procedural failures and clinical errors [10]. Indeed, these pieces of evidence indicate that minimizing interruptions would be optimal measure for nurses to ensure safe medication administration. Some interventions to avoid interruption are suggested by Kliger et al. (2009) [11]. These methods include large posters developed and placed around the unit listing quiet times for medication administration, overhead announcements at the beginning and end of quiet time for medication administration, medical team rounds only during non–medication administration times, and education of other staff about the importance of protected time for medication administration. The results showed these measures significantly improved the accuracy of medication administration [11].
Another article reported the use of a hospital-based and multi-intervention programme to evaluate interruptions that occurred during medication rounds and the results showed, interestingly, the interventions was paradoxically effective on the minimization of interruption from patients rather than that from other staff members [12]. Three strategies proposed in this study were the preparation of medications in a dedicated room, a red tabard worn by the nurses responsible for the medication round, and education of staff members about the new medication round policy. The authors proposed three methods including signage to mark areas where medications were prepared, a checklist for administration, staff and nurse education, and vests worn during medication rounds to decrease distractions and interruptions. Their results found that medication errors related to interruptions were statistically significantly decreased [13].
3.4.2. Measures to Improve Individual Knowledge and Skills, and Personal Responsibility
From the identified 181 articles, 10 studies were considered relevant to this topic. The five rights of medication safety which have long been standard to all theoretical and clinical nursing instruction are the conceptual framework for patient safety practice enhancement. Nurses are full of education and experience after several years working in clinical areas. However, nurses begin to rely on human memory and vigilance, with medications with which they are familiar [14]. Some occasions of administration error relate to nurses who are complacent about common medications or rely on visual recognition rather than reading carefully. The process of precise and clear checking in each step of the “five rights” is crucially important for nurses to adhere to; nurses are regarded as gate-keepers to the safe administration of drugs to patients. Therefore, a strategy needed to improve individual knowledge, skills and personal responsibility is to change individuals’ mindfulness and behaveior in medication administration practice. Education is not the only way but must be provided along with other interventions to reduce administration error. Patient mortality has been found to be linked to nurses’ educational attainment [15], and knowledge may safeguard against medication errors [16].
One study indicated that there was limited pharmacological knowledge in nursing and recognition of inadequate teaching in pharmacology was noted [17]. Pharmacological education is a potential improving strategy to increase confidence and proficiency in medication administration for nurses. Since there are no national competency guidelines which explicitly identify the adequate amount and depth of pharmacological knowledge for nursing practice [18], it is hard to develop a competence guide to ascertain a certain level in nursing. In addition, nurses have graduated from accredited institutes following a comprehensive and rigorous training to obtain their license to practice which means that they should be assumed to have the necessary competence to provide safe nursing practices to patients. However, this does not mean that they do not need to have further programmes or trainings for consolidation of their knowledge and skills. A study examined a 3-month educational intervention with qualified nurses, using a nonrandomized, single group comparing preand post-outcome variables so that, by reinforcing basic medication administration procedures, medication administration errors in the emergency department could be reduced [19]. Although the result of the educational intervention showed no improvement in total medication errors, it successfully improved knowledge of recommended medication administration practices. Research reported in an article mentioned earlier focused on Integrated Nurse Leadership Program to improve the reliability of medication administration by developing and deploying nurse leadership and process improvement skills on one medical/surgical inpatient unit [11]. The program consisted of six safety processes to improve the accuracy of medication administration. It included comparing the medication label to the medication administration record (MAR), keeping medication labeled throughout, checking two means of patient identification (ID), explaining the drug to patient (if applicable), charting immediately after administration, and protecting the process from distractions and interruptions. Although the results showed improvement in the accuracy of medication administration after the intervention, only members of staff involved in this project though the program were sustainably improved. This program was implemented successfully when each team developed a sustainability plan entailing monitoring of progress. However, the sustainability of the accuracy of medication administration can become susceptible if there is no on-going monitoring. More measures are required to ensure so that the interventions can be sustained.
One article suggested the use of counter checking to minimize medication errors [20]. Counter checking is essential when preparing and administering a high alert medication and specific procedures of administration. A literature review evaluated the evidence from research reported in sixteen articles for double checking the administration of medicines [21]. There was insufficient evidence to either support or refute the practice of double checking the medication administration. In spite of Alsulami’s findings in an earlier paper [21], David (2003) illustrated an example that if a pharmacy dispensing error rate is 5% and a double check occurs before medications are dispensed, the actual chance of a dispensing error reaching the patient is 5% of 5%, that is, only 0.25% [22]. If the same could be applied in medication administration, the administration error would be theoretically minimized at 0.25% if double checks were performed independently. However, the manpower shortage is another issue we should consider, as counter-checking requires double-staffing for medication administration. Therefore, David (2003) recommends that counterchecking should only be applied strategically to situations that most warrant the medication administration in high alert medications [22]. Fewer well-placed counter checks in selecting high alert medications will be much more successful than an overabundance of counter checks [22].
4. DISCUSSION
After reviewing the one recent year’s medication administration errors in the UCH, the current guidelines, policies and measures using, and the contributory factors and the measures suggested from the literature, lots of preventive measures, guidelines and policies have been introduced in the UCH. However, most of the measures can only address the contributory factors but not the internal and external factors. Some of the key measures were currently recommended to policy makers and nurses for further attention.
The interruption which is seldom to be associated with medication errors in the UCH is frequently highlighted in the literature as a causative factor. Although there is no strong evidence to support the positive association between interruption and medication errors, no measure is currently used to address this issue in the UCH. Executive officer may consider if the suggested strategies (external) such as wearing a red tabard and educating staff members about the new medication round policy should be implemented.
In addition, education is an important element to minimize medication errors. Education is one of the ways to change individuals’ mindfulness and behavior (internal) in medication administration practices. Each of the nurses should require receiving on-going education regardless the length of nurses’ experience. The content of the education can be more diversified and widespread, including pharmacological knowledge, the accuracy of medication administration and the sharing of medication administration errors analysis. Some medication administration errors were associated with poor mathematical calculation skill especially arithmetic. There is no ongoing arithmetical assessment in UCH because nurses are supposed to have full of competence to do so. Education reinforcement is suggested to uphold the medication safety whereas mathematical assessment or quiz is suggested to be promoted in order to maintain the concept of arithmetic. The behavior of nurses on medication administration is valuable to be explored in future.
5. CONCLUSION
Several suggested measures from the literature have been reported in order to address the internal and external factors identified such as the development of large poster, listing quiet time, on-going education regarding various areas related to the medication administration and emphasis on counter-checking in high alert medication. Other potentially effective measures, such as bar-code technology, are not mentioned in this text but that does not mean that they are less important. This is because other measures may require much time to build up and to conduct pilot test in clinical area or a lot of resources to support. This article has suggested measures that would be possible in our settings. It is evident that medication administration errors should be avoided, and use of the different preventive measures discussed in this paper may have the potential to improve the safety in the process of medication administration. We hope to address the measures that can help improve the internal and external practices and behavior through an education reinforcement programme and interventions to prevent contributory factors to the procedure after comparing the existing measures to the suggested measures from literature.
6. ACKNOWLEGEMENTS
This study is supported by Deputizing General Manager (Nursing) of Nursing Services Division, United Christian Hospital. I would like to extend my gratitude to thank Ms. Yuk Tak Kwan (Dep. GMN) and Mr. William Poon Tak Fai (SNO) to provide valuable opinion on this study.
REFERENCES
- Reason, J. (1990) Human error. Cambridge University Press, Cambridge. http://dx.doi.org/10.1017/CBO9781139062367
- Gibson, T. (2001) Nurses and medication error: A discursive reading of the literature. Nursing Inquiry, 8, 108- 117. http://dx.doi.org/10.1046/j.1440-1800.2001.00098.x
- HAHO Medication Safety Committee (2012) HA Guidelines on Medication Management—Prescribing, Dispensing and Administration (Administration Guidelines). http://uchweb5/Pharm/Guidelines/HAHO%20and%20Medication%20Safety%20Committee/HA%20Guidelines%20on%20Medication%20Management-Prescribing,Dispensing%20and%20Administration.pdf
- Self-Assessment Guide for Medication Safety (2005) Hospital Authority. http://uchweb5/Pharm/Guidelines/HAHO%20and%20Medication%20Safety%20Committee/Self%20Assessment%20Guide%20for%20Medication%20Safety.pdf
- Drug Allergy Reference Card (2011) Kowloon East Cluster. http://uch.home/pharm/usefulinfo/AllergyRefCard.pdf
- HAHO Medication Safety Committee (2008) Safety Solutions on Look-Alike Sound-Alike Medications. http://uchweb5/Pharm/Guidelines/HAHO%20and%20Medication%20Safety%20Committee/Safety%20Solutions%20on%20Look-alike%20Sound-alike%20Medications.pdf
- Joanna Briggs Institute (2010) Evidence-based information sheets for health professionals. Best Practice, 14, 1-4.
- Tang, F.I., Sheu, S.J. and Yu, S. (2007) Nurses relate the contributing factors involved in medication errors. Journal of Clinical Nursing, 16, 447-457. http://dx.doi.org/10.1111/j.1365-2702.2005.01540.x
- Biron, A.D., Lavoie-Tremblay, M. and Loiselle, C.G. (2009) Characteristics of work interruptions during medication administration. Journal of Nursing Scholarship, 41, 330-336. http://dx.doi.org/10.1111/j.1547-5069.2009.01300.x
- Westbrook, J.I., Woods, A. and Rob, M.I. (2010) Association of interruptions with an increased risk and severity of medication administration errors. Archives of Internal Medicine, 170, 683-690. http://dx.doi.org/10.1001/archinternmed.2010.65
- Kliger, J., Blegen, M.A. and Gootee, D. (2009) Empowering frontline nurses: A structured intervention enables nurses to improve medication administration accuracy. The Joint Commission Journal on Quality and Patient Safety, 35, 604-612.
- Tomietto, M., Sartor, A. and Mazzozoli, E. (2012) Paradoxical effects of a hospital-based, multi-intervention programme aimed at reducing medication round interruptions. Journal of Nursing Management, 20, 335-343. http://dx.doi.org/10.1111/j.1365-2834.2012.01329.x
- Yoder, M. and Schadewald, D. (2012) The Effect of a safe zone on nurse distractions, interruptions, and medication administration errors. Western Journal of Nursing Research, 34, 1068-1069. http://dx.doi.org/10.1177/0193945912453687
- Miranda, S. (2011) Back to basics, medication safety at the bedside a nursing administrator’s perspective. Penn Nursing, 66, 6-10.
- Aiken, L.H., Clarke, S.P., Cheung, R.B., et al. (2003) Educational levels of hospital nurses and surgical patient mortality. JAMA, 290, 1617-1623. http://dx.doi.org/10.1001/jama.290.12.1617
- Kendall-Raynor, P. (2010) Training assessment will address medication and care concerns. Nursing Standard, 24, 7.
- King, R. (2004) Nurses’ perceptions of their pharmacological educational needs. Journal of Advanced Nursing, 45, 392-400. http://dx.doi.org/10.1046/j.1365-2648.2003.02922.x
- Bullock, S. and Manias, E. (2002) The educational preparation of undergraduate nursing students in pharmacology: A survey of lecturers’ perceptions and experiences. Journal of Advanced Nursing, 40, 7-16. http://dx.doi.org/10.1046/j.1365-2648.2002.02335.x
- Blank, F.S.J., Tobin, J. and Macomber, S. (2011) A “Back to Basics” approach to reduce ED medication errors. Journal of Emergency Nursing, 37, 141-147. http://dx.doi.org/10.1016/j.jen.2009.11.026
- Evans, J. (2009) Prevalence, risk factors, consequences and strategies for reducing medication errors in Australian hospitals: A literature review. Contemporary Nurse, 31, 176-189. http://dx.doi.org/10.5172/conu.673.31.2.176
- Alsulami, Z., Conroy, S. and Choonara, I. (2012) Double checking the administration of medicines: what is the evidence? A systematic review. Archives of Disease in Childhood, 97, 833-837. http://dx.doi.org/10.1136/archdischild-2011-301093
- David, U. (2003) Medication safety alerts. JCPH, 56, 167-169.

