Modern Economy
Vol.07 No.13(2016), Article ID:72475,9 pages
10.4236/me.2016.713139
Utilization of Health Services in the Burkina Faso Health System: Empirical Evidence of Health System Fragmentation and Integration
Ousmane Traoré
Economic and Social Science Training and Research Unit (UFR/SEG), Ouaga University II (UO2), Ouagadougou, Burkina Faso

Copyright © 2016 by author and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY 4.0).
http://creativecommons.org/licenses/by/4.0/



Received: October 8, 2016; Accepted: November 28, 2016; Published: December 1, 2016
ABSTRACT
In this paper, the utilization of health services in the context of health system fragmentation in Burkina Faso is analyzed using household living condition survey data. The methodology explores the relationships between population health risk factors and health services utilization. The results of the analysis highlighted eight reference care providers in the Burkina Faso health system; thus, the probability of service use in the first level of the system, assumed to be its point of entry, is significantly and negatively associated with age and sex, with a lower probability for female gender. As a whole, the health risk factors positively influence the probability of service use at the higher levels of the health system and in the private sector. The results suggest that utilization of the traditional health sector remains predominated by the elderly. These results thus suggest the need for coordination of care across the levels of the public healthcare sector, on the one hand, and the presence of interaction and integration between the traditional or private sector and the public sector, on the other hand.
Keywords:
Health System, Fragmentation and Integration, Health Risk Factors, Utilization of Health Services

1. Introduction
In Burkina Faso, the health system has a pyramid structure (see Figure 1), in which, the first (bottom) level consists of the Health and Social Promotion Centers (CSPSs), assumed to be the point of entry to the health system. At the intermediate level, there are successively larger medical centers with surgical units (CMA/CM), which take referrals
Figure 1. The health system pyramid structure of Burkina Faso. Source: author’s construction.
from the CSPSs, and the regional hospital (CHR). On top of the health pyramid is the National University Hospital (CHN), which provides specialized care. This fragmentation of the health pyramid seems to correspond to a hierarchy of care. Alongside this public health sector, there are two coexisting care-providing sectors, namely the private sector and the traditional sector.
By analyzing the utilization of health services in this context of health system fragmentation in Burkina Faso, the main purpose of this paper is to highlight the potential challenges associated with this fragmentation and provide the basis on which future studies should be conducted. Indeed, [1] argued that most health systems are characterized by fragmentation and continue to face the major challenge of integration between the various parts of the system. Henceforth, to enhance integration, the first step is to perform an assessment of the health system fragmentation and integration.
We conducted a demand-side analysis focused on the utilization of health services by the population instead of healthcare provision to empirically study fragmentation and integration within the Burkina Faso health system. The paper is organized as follows: Section 2 briefly introduces the methodology and data; the main results are presented and discussed in Section 3, and Section 4 concludes the paper.
2. Method and Data
2.1. Count Data for Health Services Utilization
The health services utilization data analyzed in this paper was obtained from the survey of household living conditions in Burkina Faso in 1998. This survey was conducted by the National Institute of Statistics and Demography (INSD). One of the main objectives of the survey was to provide data at each of the 10 planning regions defined by the Ministry of economy and finance in order to enable economic analysis. To this end, the survey covered a sample of 8,500 households. The utilization of health services was determined according to the number of services used by persons who had a disease fifteen days prior to survey participation. The records in this database provided a sample pool including 44,941 observations (individual).
Table 1 summarizes the descriptive statistics for the count data used to assess health services utilization in Burkina Faso. This table shows nine potential types of healthcare services in the Burkina Faso health system. They include: the traditional healer, the private doctor, the private pharmacist, the private nurse, the other private stakeholders, the CSPS, the CMACM, the CHR and the CHN. For each of these nine types of health services, the variance in utilization is (far) higher than what would be expected on average. Therefore, there is overdispersion of the count data for the variable used to analyze health services utilization in Burkina Faso in this paper.
Table 1. Summary of health services1 utilization data.
Source: Author’s calculations using Stata.
2.2. The Count Data Model for Health Services Utilization
Utilization of healthcare services is analyzed using a count data model. However, events such as visits to a doctor or a specialist, or in short, utilization of health services, may be affected by recall bas, causing a correlation between the utilization of different healthcare services. For the modelling of correlated count data, [2] showed that the negative binomial distribution was more appropriate than the Poisson distribution because the Poisson distribution assumes that the average equals the variance and therefore is not consistent with the overdispersion observed in our data. In addition, the Poisson distribution would assume utilization events to occur independently. Therefore, a negative binomial model is used in this paper.
To account for the overdispersion observed in our data, we use the [3] extension of the Poisson model, which assumes the Poisson parameter  to be gamma distributed with parameters
to be gamma distributed with parameters  and
and ; therefore,
; therefore,
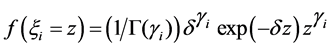 (1)
(1)
with 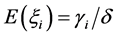 and
and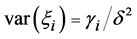 .
.
Thus, letting  be considered as the count data variable of interest, or the number of health services visits,
be considered as the count data variable of interest, or the number of health services visits,  takes one of the values
takes one of the values  Since
Since  is Poisson
is Poisson 
 (2)
(2)
This equation represents the negative binomial distribution with 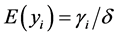 and
and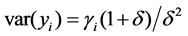 . Therefore, in cases in which the variance is higher than the mean, this model is appropriate for the treatment of overdispersion in data. In fact, we have
. Therefore, in cases in which the variance is higher than the mean, this model is appropriate for the treatment of overdispersion in data. In fact, we have
 (3)
(3)
2.3. Definition, Measurement and Descriptive Analysis of Explanatory Variables
[4] Showed that during the analysis of healthcare services utilization, the parameter of the distribution law for the number of healthcare service visits can be expressed as a fun- ction of observable individual attributes and health characteristics. To analyze the use of healthcare services, we thus assume that key drivers, in addition to income, include health risk factors (see Figure 2) relating to the individual, namely age, sex, health status, marital status and disability.
In this study, health status was assessed by applying the Goldberg scoring method to the General Health Questionnaire (GHQ). Thus, variables considered in the model included the area of residence, type of toilets, garbage disposal method and drinking water supply system (see Table A1 in the Appendix for the different categories of these variables and their assigned values used when computing health status).
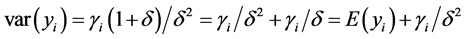
Income was predicted using the instrumental variables estimation method, as follows:
 (4)
(4)
in which vector 

3. Results and Discussion
Table 3 shows the estimation results of the negative binomial model (Equation (2)) for health services utilization in the Burkina Faso health system. In this fragmented health system, our results indicate that only the utilization of a private pharmacist for healthcare services did not seem to be correlated with any health risk factor as a determinant of health services utilization. Indeed, the estimates for this modality of health care services did not converge and were not identified as significant even when using alternative estimation methods.
Figure 2. Components of variations in health spending: health risk factors. Source: Built from [5] .
Table 2. Measures and descriptive statistics for explanatory variables.
Source: Author’s calculations using Stata.
For the others modalities of health services in the Burkina Faso health system, our results highlight that sex and age as determinants of care services utilization are negatively and significantly correlated with the use of CSPS, considered to be the point of entry to the Burkina Faso health system. However, the probabilities of using higher levels of the health system were positively associated with the following risk factors: health status is associated with CMA/CM use; sex, age, and marital status are associated with CHR use; and marital status is associated with CHN use. Apart from the public sector of the health system, having received consultations from traditional healers is positively correlated with age, particularly among the elderly. As a whole, use of the private healthcare sector is positively correlated with the evaluated health risk factors.
Given these results, the reform in Burkina Faso aimed at making CSPSs a mandatory point of entry to the health system proves relevant and should be strengthened and accompanied by support measures designed primarily to optimize the waiting time of patients in CSPSs while decongesting facilities within the upper level of the health system, such as the CHR and the CMA/CM, thereby ensuring better coordination of care across the various providers in the health system. [6] showed that while waiting times can be a tool used to control healthcare demand in countries with health insurance systems, it is never optimal to have a positive waiting time when the marginal cost of waiting times is higher for patients expecting a significant benefit from healthcare. Furthermore, mechanisms to facilitate integration and coordination between the private and public sectors should be envisioned. Indeed,
Table 3. Estimation results of the negative binomial model for health services utilization in the Burkina Faso health system.
Source: Author’s calculation using Stata. Notes: Standard deviations are reported in parentheses. *, ** and *** indicate significance at 10%, 5% and 1% respectively.
private healthcare providers have often been considered to generate additional costs in healthcare or health insurance systems. In the case of Burkina Faso, for example, [7] demonstrated that the use of external care (private providers) was associated with a significant increase in the direct costs of household healthcare in the Nouna District in Northwest Burkina Faso.
4. Conclusions
The health system in Burkina Faso has a pyramid structure. Thus, we analyze the utilization of healthcare within this system by highlighting system fragmentation and its associated challenges. This paper suggests the need for integration between the various providers in the system. In line with this need, recent empirical research has focused on essential aspects required for integration of a fragmented system. Using a qualitative approach, Shevski and Sheiman (2014) performed a conceptual assessment of fragmentation and integration, arguing that the key attributes of integration were teamwork, coordination and continuity of care.
In Burkina Faso, some steps have been taken towards continuity of care, namely encouraging use of the first level of care provision as the point of entry to the health system. However, research conducted on fragmented and highly integrated systems should consider all dimensions of integration to improve the efficiency of healthcare provision.
Cite this paper
Traoré, O. (2016) Utilization of Health Services in the Burkina Faso Health System: Empirical Evidence of Health System Fragmentation and Integration. Modern Economy, 7, 1555-1563. http://dx.doi.org/10.4236/me.2016.713139
References
- 1. Sheiman, I. and Shevski, V. (2014) Evaluation of Health Care Delivery Integration: The Case of the Russian Federation. Health Policy, 115, 128-137.
http://dx.doi.org/10.1016/j.healthpol.2013.12.011 - 2. Amemiya, T. (1985) Advanced Econometrics. Harvard University Press, Cambridge.
- 3. Cameron, A.C. and Trivedi, P.K. (1986) Econometric Models Based on Count Data: Comparisons and Applications of Some Estimations and Tests. Journal of Applied Econometrics, 1, 29-53.
http://dx.doi.org/10.1002/jae.3950010104 - 4. Cameron, A.C., Trivedi, P.K., Milne, F. and Piggott, J. (1988) A Microeconometric Model of the Demand for Health Care and Health Insurance in Australia. Review of Economic Studies, 55, 85-106.
http://dx.doi.org/10.2307/2297531 - 5. Van de Ven, W.P.M.M. and Ellis, R.P. (2000) Risk Adjustment in Competitive Health Plan Markets. In: Culyer, A.J. and Newhouse, J.P., Eds., Handbook of Health Economics, Elsevier Science BV, Amsterdam, p. 768.
- 6. Gravelle, H. and Siciliani, L. (2008) Optimal Quality, Waits and Charges in Health Insurance. Journal of Health Economics, 27, 663-674.
http://dx.doi.org/10.1016/j.jhealeco.2007.08.004 - 7. Su, T.T. and Flessa, S. (2013) Determinants of Household Direct and Indirect Costs: An Insight for Health-Seeking Behaviour in Burkina Faso. European Journal of Health Economics, 14, 75-84.
Appendix
Table A1. Categories and values of health status variables (GHQ).
Source: Built from the INSD’s 1998 survey data base.
Table A2. Results of income estimation using instrumental variables.
Source: Author’s calculation using Stata. Notes: Standard deviations are reported in parentheses. *, ** and *** indicate significance at 10%, 5% and 1% respectively. CNSS: National Social Security Fund; CARFO: Independent Civil Servants’ Pension Fund; cnasur: variable for CNSS + insurance; carsur: variable for CARFO + insurance; irevtran: variable for transitory income.
NOTES
1Tradhealer: traditional healer; Privdoc: private doctor; Privpharm: private pharmacist; Privnurs: private nur- se; Private: Other private stakeholders.





