Open Journal of Nursing
Vol.3 No.2(2013), Article ID:32985,6 pages DOI:10.4236/ojn.2013.32039
A study evaluating the effect of Educational Needs Assessment Tool (ENAT) focused patient education, on health outcomes in patients with Rheumatoid Arthritis: Protocol of an ongoing study*
![]()
1R&D Department, Barnsley Hospital NHS Foundation Trust, Barnsley, UK
2Academic and Clinical Unit for Musculoskeletal Nursing, School of Healthcare, University of Leeds, Leeds, UK
3Academic and Clinical Unit for Musculoskeletal Nursing, Institute of Rheumatic and Musculoskeletal Medicine, University of Leeds, Leeds, UK
4Medical Statistics, School of Health and Related Research, University of Sheffield, Sheffield, UK
Email: bernadette.hardware@nhs.net, c.a.hale@leeds.ac.uk, dawn.johnson2@nhs.net, j.hill@leeds.ac.uk, t.a.young@sheffield.ac.uk, aadebajo@nhs.net
Copyright © 2013 Bernadette Hardware et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received 4 February 2013; revised 6 March 2013; accepted 15 April 2013
Keywords: Educational Needs Assessment Tool; Protocol; Rheumatoid Arthritis; Self Management; Patient Education
ABSTRACT
Aims and objectives: To evaluate the effectiveness of a patient education tool (the ENAT) on self efficacy, patient knowledge, health outcomes and its usability in practice. Background: The effectiveness and value of patient education in rheumatoid arthritis have been questioned. The ENAT was developed to help the nurses to provide more focused, individualized and relevant education. The psychometric properties of the ENAT have been assessed. Design: This study is a single blind randomized controlled trial using both quantitative and qualitative methodology. The primary outcome is patient self efficacy. Secondary outcomes are physical function, psychological status, pain levels, social interaction and patient knowledge of disease. Methods: 130 RA patients will be randomized into an experimental (EG) or control group (CG). The EG patients will complete the ENAT prior to seeing a Clinical Nurse Specialist (CNS) at weeks 0, 16 and 32. The CNS will use the ENAT as a template to meet patients perceived educational needs in addition to the usual care. The CG will receive their usual care from the CNS without the aid of the ENAT. To determine the ENAT’s usability, semi-structured quail- tative interviews will take place with the practitioners and a sample of patients once they have completed the quantitative arm of the study. Results: The study commenced in April 2011 and the results are expected to be available after April 2013. Conclusions: It is hypothesized that nurses’ use of the ENAT will lead to increased patient self efficacy, and improved patient knowledge and health outcomes among the patients who used it. Furthermore, it is hypothesized that the ENAT will be easy for staff and patients to use. Relevance to clinical practice: The ENAT was developed to assess the perceived educational needs of patients with rheumatoid arthritis and thus help the nurses to provide more focused, individualised and relevant education.
1. BACKGROUND
Rheumatoid Arthritis (RA) is a chronic progressive and disabling disease associated with significant levels of pain, morbidity and reduced psychosocial and economic status [1,2]. There are approximately 400,000 people with RA in the UK with around 12,000 new cases being identified each year [3]. The disease has no predictable course and the extent of distress experienced varies greatly between patients and over time in the same patient [4]. Patients with RA have many and varied needs, including education and information relating to their disease. Therefore, in addition to offering specific treatments and therapies, nurses and health professionals spend a great deal of time providing advice and patient education to enable these patients to understand and manage their disease themselves [5]. There is published evidence to demonstrate that effective patient education is empowering, because it improves self efficacy and enables patients to cope with and manage their disease [6-8] and to adhere to drug regimens [9], but the outcomes are not strong [10]. A Cochrane review which examined the effectiveness of patient education on health status in early RA patients, suggested that although patient education has a small beneficial effect, these effects are short lived [1]. These findings may in part be explained by the work undertaken Brooks et al. [11] which demonstrated that many people with arthritis want to know more about their disease and treatments, but that a disparity exists between the patients’ perceptions of their educational needs and the health professionals who provide the education. This could mean that the educational interventions in the studies included in the Cochrane review [1], were not perceived by patients as relevant. Alternatively, it could mean that the outcome measures used were not the most appropriate. Either way, J. Kirwen [12] suggests that the effectiveness and clinical relevance of patient education in RA remains unclear. These debates notwithstanding, current guidelines for care of people with RA and other forms of arthritis, do emphasize the importance of integrating education and information into care delivery systems [13].
To address the above concerns, a patient self-completed Educational Needs Assessment Tool (ENAT) [4] was developed for use by health professionals to enable them to identify the educational needs of RA patients and then focus the education input upon those areas identified. The ENAT is a simple tool, which comprises 39 items divided into 7 domains: managing pain; movement; feelings; arthritis process; treatments; self-help measures; support systems. The psychometric properties of the ENAT for people with RA have been evaluated by fit to the Rasch model [14] and it was found to be unidimensional and free of Differential Item Functioning (DIF) for RA patients [15]. The ENAT was translated and adapted into 6 other European languages and its domains were found to be uni-dimensional and largely invariant by age, gender, educational level and disease duration for RA patients within each country [16-18]. The ENAT has also been used as a research tool to assess patients’ knowledge before and after an educational intervention [19].
However the effectiveness and usability of the ENAT for use within clinical practice is as yet unknown, and therefore the aim of this study is to evaluate the usability and effectiveness of the ENAT in clinical practice. The study commenced in April 2011 and the results are expected to be available after April 2013.
2. METHODS
2.1. Study Design
This study has been designed as a pragmatic trial in a complex clinical environment, and is being conducted over 36 months. Patients are being recruited from six centres in the United Kingdom. Randomization is carried out by an independent statistician. The randomization is stratified by centre and generated using block randomization based upon a computer program for generating random numbers. The results of the randomization are held at each centre in numbered sealed envelopes. If a patient decides to leave the study immediately following randomization, the number and code will be discarded.
2.2. Study Sample
One hundred and thirty (130) patients with Rheumatoid Arthritis are being identified from the list of new Rheumatology Clinic referrals to 6 hospital Rheumatology Departments. Inclusion criteria are defined as: aged 18 years or older, and have the ability to complete the study questionnaires unaided. Exclusion criteria are: patients who are suffering from a severe mental health problem which is likely to impair their ability to provide informed consent, and patients who are unable to complete the questionnaire unaided.
2.3. Hypothesis
The study hypotheses are that:
1) The nurses’ use of the Educational Needs Assessment Tool (ENAT) to determine the educational needs of RA patients, and subsequently focus patient education on these needs, will lead to increased patient self-efficacy, improved patient outcomes, and demonstrate long term health benefits;
2) The ENAT will be considered by those using it to be a user-friendly tool, which can be easily incorporated into routine clinical practice.
3. OUTCOME MEASURES
The primary outcome measure for this study is patient self efficacy, which will be measured by the Arthritis Self Efficacy Scale (ASES) devised by Lorig [20]. The secondary measures are patient physical function, psychological status, pain levels, social interaction and patient knowledge of disease. These outcome measures were chosen as they form part of the core set of outcome measures in clinical trials of RA which were agreed upon by the OMERACT committee [11,21,22]. Secondary outcomes will be measured by the AIMS2-SF [23] and the Patient Knowledge Questionnaire [24].
To determine the ENAT’s usability within the practice setting, a purposive sample of patients is being invited to take part in semi-structured qualitative interviews. Sixteen to twenty patients from the two main participating hospitals will be interviewed, as well as the Clinical Nurse Specialist (CNS) from hospital which recruited more than 15 patients. Interviews will take place within two weeks of participant completion in order to ensure that the recollection of events is reliable.
4. PRIMARY OUTCOME: SELF EFFICACY
Self-efficacy is a psychological construct that refers to an individual’s belief that he or she has the ability to perform certain behaviours successfully, to achieve a desired outcome [25]. Over the last 15 years self-efficacy has become an important psychosocial variable for people with RA [26] because studies have suggested that a person’s self-efficacy can mediate health-related outcomes for people with RA [27-29] and improve symptom management [30]. Self-efficacy is conceptualized as being domain specific, i.e. self-efficacy assesses a person’s confidence that he or she can perform a particular task (e.g., manage arthritis pain) rather than a global sense of control or mastery [25]. A high level of selfefficacy in a person can be a useful factor when coping with a chronic disease such as RA. In this study selfefficacy is being measured using the Arthritis Self Efficacy Scale (ASES) [20]. The ASES is a 20 item questionnaire consists of 3 domains; pain, function and “other symptoms” (such as fatigue, depression and frustration). Scores range from 1 (very uncertain) to 10 (very certain), with higher scores indicating higher self-efficacy [20]. However because in this study, function is being measured using Arthritis Impact Measurement Scales 2-SF (see AIMS2-SF below) described by Guillemin et al. [23], only the pain and “other symptoms” subscales of the ASES will be used.
5. SECONDARY OUTCOMES
The secondary patient outcomes for this study are physical function, psychological status, pain levels, social interaction and patient knowledge of disease.
These are measured by the AIMS2-SF [23] and the Patient Knowledge Questionnaire [24]. AIMS2-SF is a shortened form of AIMS2 [31]. The AIMS questionnaires are widely used disease-specific tools measuring many aspects of health status. They have been shown to be more responsive in patients with arthritis than any of the generic measures [32]. AIMS2-SF has similar psychometric properties to the full length versions but takes about 10 minutes to complete and score and so more appropriate in routine clinics [23]. It has 5 scales (26 items) comprising lower extremity function, upper extremity function, affect, pain and social interaction. The tool is self completed using a 5-point scales ranging from all days to no days. Low scores indicate higher health status.
The Patient Knowledge Questionnaire (PKQ) has been designed for use with patients who have RA. It comprises 12 multi-choice questions with a choice of 5 responses. Topics included are aetiology of RA, signs and symptoms, drug therapy and monitoring, joint protection and exercise and energy conservation. The PKQ has been shown to be stable (test/retest Pearson’s correlation coefficient 0.965), internally consistent (Cronbach’s alpha 0.62) and sensitive to change following a one hour education programme (Mann Whitney U test p < 0.001). It is quick to complete and easy to score. A higher score indicated higher levels of knowledge [24].
6. STUDY POWER
The sample size calculation of 130 patients is based on the primary end points of the ASES pain and symptoms scales and is based on clinical opinion of an acceptable change and the results of a study by Barlow et al. [33]. Assuming a mean difference of 5.5 (SD = 10.0) as being clinically meaningful for both the ASES pain and other symptoms scale with a 5% significance level and 80% power, 52 patients per arm of the trial are required (total 104). Further, it is expected that 25% of patients will be lost to follow up during the study period and therefore the study will aim to recruit 130 patients to allow for this.
7. PROCEDURES
On attendance at the Rheumatology clinic and prior to their consultation, those patients who fulfill the inclusion criteria, have received the relevant study information, and have provided written informed consent, are randomised either to receive and complete the ENAT (the experimental group), or receive usual care (the control group). For the experimental group, the Rheumatology Clinical Nurse Specialist (CNS) uses the patients’ completed ENAT as a template to meet the patients’ perceived educational needs in addition to the usual care provided by the nurse, and documents the educational intervention. Patients in the control group receive the usual care given by the nurse to rheumatology patients. For both groups of patients, the CNS completes a checklist after each consultation, which records the patient education which has been provided. At the end of the consultation all patients (both experimental and control groups), receive the above mentioned three validated health outcome assessment questionnaires. These are given to the patients by the CNS and returned by post to the research assistant. All patients then attend for two further visits to the CNS, at weeks 16 and 32, (as this is usual practice within the participating hospitals). The experimental group will complete the ENAT again at each visit and the control group will receive the usual care with the CNS recording any patient education that was given. At the end of each of these visits all patients will again complete the three above mentioned questionnaires. Figure 1 shows the flow diagram for the study.
8. ANALYSIS
All quantitative analysis will be undertaken on an intention to treat basis with a significance level of p < 0.05 regarded as statistically significant. The distribution of the data will be examined before the selection of the most appropriate statistical tests to use for analysis it is expected that a non-parametric analysis will be undertaken because the underlying distribution of the underlying scales in the questionnaires are typically asymmetric. The Wilcoxon signed rank test will be used to assess statistical significance within groups and the MannWhitney U tests for differences between groups after allowing for baseline differences using change scores. Friedman’s test will be applied to allow for the repeated measures nature of the data. This is equivalent to ANOVA repeated measures analysis. Data will be entered and analysed using SPSS.
The qualitative analysis of the verbatim interviews from this study will be analysed by the Framework method [34]. This method was developed in the UK specifically for applied or policy relevant qualitative research where the objectives of the investigation are clearly set out beforehand (Pope et al., 2000). The Framework method offers a clear analytic structure which enables both the researcher and other potential researchers trans-
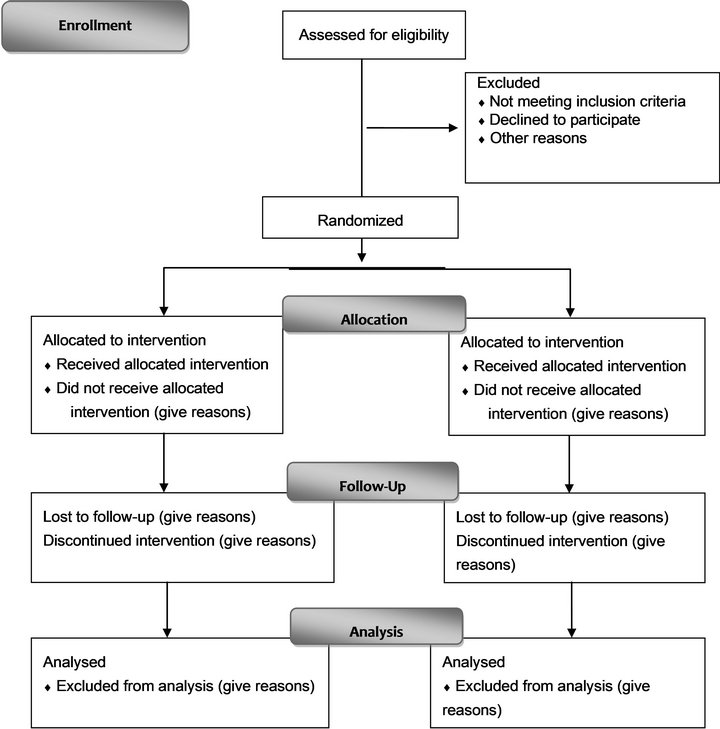
Figure 1. ENAT patient flow chart.
parency in the processes involved in the data analysis. The five-key stages are:
1) Familiarisation;
2) Identification of a thematic framework;
3) Indexing;
4) Charting;
5) Mapping and interpretation.
9. ANTICIPATED BENEFITS
There are over 400,000 people with Rheumatoid Arthritis in the UK, and they comprise a large proportion of visits the rheumatology clinics. The ENAT has the potential to impact directly on patient care if it enables Clinical Nurse Specialists (CNS) to deliver appropriate and timely patient education. In turn, this could enable patients to improve self management of their disease by increasing their self efficacy.
Previous work on the ENAT suggests that it is a valid and reliable tool. By determining individual patient educational needs, the CNS should be able to deliver a more patient tailored education programme. This should reduce time spent by the practitioner delivering education and advice seen by the patient to be of less relevance to the management of their disease.
The RCT will demonstrate if the ENAT is effective for use within a clinical practice setting, which in turn many lead to wider use and acceptability of the ENAT in rheumatology clinics.
10. STUDY REGISTRATION, FUNDING AND ETHICAL APPROVAL
The study is registered on the UK clinical research network study portfolio database ID number 9230, and the International Standard Randomized Controlled trials register ID number 51523281. Ethical approval for the study was obtained from South Yorkshire Research Ethics Committee. The study is funded by the UK NIHR Research for Patient Benefit Programme.
11. ACKNOWLEDGEMENTS
This article presents independent research funded by the National Institute for Health Research (NIHR) under its Research for Patient Benefit (RfPB) Programme (Grant Reference Number PB-PG-0408- 16106). The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health
REFERENCES
- Riemsma, R., Kirwen, J., Taal, E. and Rasker, H. (2003) Patient education for adults with Rheumatoid Arthritis. Cochrane Database of Systematic Reviews, Ariticle ID: CD003688.
- Lapsley, H., March, L.M., Tribe, K.L., Cross, M.J., Courtney, B.G. and Brooks, P.M. (2002) Living with Rheumatoid Arthritis: Expenditures, health status and scoial impact on patients. Annals of Rheumatic Disease, 61, 818- 821. doi:10.1136/ard.61.9.818
- Arthritis Research C (2002) Arthritis—The big picture. Arthritis Research Campaign Chesterfield. Arthritis Research UK. http://www.arthritisresearchuk.org/policy-and-public-affairs/reports-and-resources/reports.aspx
- Hardware, B., Lacey, E. and Shewan, J. (2004) Towards the development of a tool to assess educational needs in patiens with arthritis. Clinincal Effectiveness in Nursing, 8, 111-117.
- Hill, J. (2003) An overview of education for patients with rheumatic diseases. Nursing Times, 99, 26-27.
- Lorish, C. and Boutaugh, M. (1997) Patient education in rheumatology. Epidemiology and Health Services Research, 9, 106-111.
- Mazzuca, S., Brandt, K., Katz, B., Chambers, M., Byrd, D. and Hanna, M. (1997) Effects of self care education on the health status of inner-city patients with osteoarthritis of the knee. Arthritis and Rheumatism, 40, 1466-1474. doi:10.1002/art.1780400815
- Edworthy, S. and Devins, G. (1996) Improving medication adherence through patient education: Distinguishing between appropriate and inappropriate utilisation. Journal of Rheumatology, 26, 1793-1801.
- Hill, J., Bird, H. and Johnson, S. (2001) Effect of patient education on adherence with drug treatment for RheumaToid Arthritis; a randomised controlled trial. Annals of Rheumatic Disease, 60, 869-875.
- Li, L.C. (2007) If knowledge is power, why don’t RheuMatoid Arthritis education programs show better outcomes? The Journal of Rheumatology, 34, 1645-1646.
- Brooks, P., Hochberg, M. and for ILAR and OMERACT (2001) Outcome measures and classification criteria for the rheumatic diseases. A compilation of data from OMERACT (Outcome Measures for Arthritis Clinical Trials), ILAR (International League of Associations for Rheumatology), regional leagues and other groups. Rheumatology, 40, 896-906. doi:10.1093/rheumatology/40.8.896
- Kirwen, J. (2007) Patient education—From information to empowerment. Annals of Rheumatic Disease, 66, 10.
- Combe, B., Landewe, R., Lukas, C., Bolosiu, H.D., Breedveld, F., Dougados, M., Emery, P., Ferraccioli, G., Hazes, J.M.W., Klareskog, L., et al. (2007) EULAR recommenddations for the management of early arthritis: Report of a task force of the European Standing Committee for International Clinical Studies Including Therapeutics (ESCISIT). Annals of the Rheumatic Diseases, 66, 34-45. doi:10.1136/ard.2005.044354
- Rasch, G. (1960) Probabilistic models for some intelligence and attainments tests. University of Chicago, Chicago.
- Hill, J., Tennant, A. and Adebajo, A. (2004) Further development of an educational needs tool (ENAT) for patients with rheumatoid arthritis. Arthritis and Rheumatism, 50, 616.
- Ndosi, M., Tennant, A., Bergsten, U., Kukkurainen, M., Machado, P., de la Torre-Aboki, J., Vliet Vlieland, T., Zangi, H. and Hill, J. (2011) Cross-cultural validation of the educational needs assessment tool in RA in 7 European countries. BMC Musculoskeletal Disorders, 12, 110. doi:10.1186/1471-2474-12-110
- Hale, C., Hill, J. and Tennant, A. (2006) The use of RASch analysis in the construct and cross-cultural validation of questionnaire data: An example from the educational needs assessment tool. Annals of Rheumatic Disease, 65, 665.
- Meesters, J.L., Vliet Vlieland, T.M., Hill, J. and Ndosi, M. (2009) Measuring educational needs among patients with rheumatoid arthritis using the Dutch version of the Educational Needs Assessment Tool (DENAT). Clinical Rheumatology, 28, 1357-1357. doi:10.1007/s10067-009-1271-3
- Grønning, K., Skomsvoll, J.F., Rannestad, T. and Steinsbekk, A. (2012) The effect of an educational programme consisting of group and individual arthritis education for patients with polyarthritis—A randomised controlled trial. Patient Education and Counseling, 88, 113-120. doi:10.1016/j.pec.2011.12.011
- Lorig, K., Chastain, R.L., Ung, E., Shoor, S. and Holman, H.R. (1989) Development and evaluation of a scale to measure perceived self-efficacy in people with arthritis. Arthritis & Rheumatism, 32, 37-44. doi:10.1002/anr.1780320107
- Tugwell, P. and Boers, M. (1993) OMERACT conference on outcome measures in RA clinical trials: Introduction. Journal of Rheumatology, 20, 528-530.
- Tugwell, P., Boers, M., Baker, P. and Snider, J. (1994) Endpoints in rheumatoid arthritis. Journal of Rheumatology, 21, 2-8.
- Guillemin, F., Coste, J., Pouchot, J., Ghézail, M., Bregeon, C. and Sany, J. (1997) The AIMS2-SF. A short form of the arthritis impact measurement scales 2. Arthritis & Rheumatism, 40, 1267-1274.
- Hennell, S.L., Brownsell, C. and Dawson, J.K. (2004) Development, validation and use of a patient knowledge questionnaire (PKQ) for patients with early rheumatoid arthritis. Rheumatology, 43, 467-471. doi:10.1093/rheumatology/keh069
- Bandura, A. (1977) Self-efficacy; towards a unifying theory of behavioural change. Psychological Review, 84, 191- 215. doi:10.1037/0033-295X.84.2.191
- Somers, T.J., Shelby, R.A., Keefe, F.J., Godiwala, N., Lumley, M.A., Mosley-Williams, A., Rice, J.R. and Caldwell, D. (2010) Disease severity and domain-specific arthritis self-efficacy: Relationships to pain and functioning in patients with rheumatoid arthritis. Arthritis Care & Research, 62, 848-856. doi:10.1002/acr.20127
- Primdahl, J., Wagner, L. and Hørslev-Petersen, K. (2010) Self-efficacy in rheumatoid arthritis: translation and test of validity, reliability and sensitivity of the Danish version of the Rheumatoid Arthritis Self-Efficacy questionnaire (RASE). Musculoskeletal Care, 8, 123-135. doi:10.1002/msc.172
- Marks, R. (2001) Efficacy theory and its utility in arthritis rehabilitation: Review and recommendations. Disability and Rehabilitation, 23, 271-280. doi:10.1080/09638280010004162
- Lorig, K., Ritter, P., Laurent, D. and Hobbs, M. (2001) Effect of a self management programme on patients with chronic disease. Effective Clinical Practice, 4, 256-62.
- Brekke, M., Hjortdahl, P. and Kvien, T.K. (2003) Changes in self-efficacy and health status over 5 years: A longitudinal observational study of 306 patients with rheumatoid arthritis. Arthritis Care & Research, 49, 342-348. doi:10.1002/art.11112
- Meenan, R.F., Mason, J.H., Anderson, J.J., Guccione, A.A. and Kazis, L.E. (1992) AIMS2. The content and properties of a revised and expanded arthritis impact measurement scales health status questionnaire. Arthritis & Rheumatism, 35, 1-10. doi:10.1002/art.1780350102
- Carr, A. (2003) Adult measures of quality of life: The arthritis impact measurement scales (AIMS/AIMS2), disease repercussion profile (DRP), EuroQoL, nottingham health profile (NHP), patient generated index (PGI), quality of well-being scale (QWB), RAQoL, short form-36 (SF-36), sickness impact profile (SIP), SIP-RA, and world health organization’s quality of life instruments (WHOQoL, WHOQoL-100, WHOQoL-Bref). Arthritis Care & Research, 49, S113-S133. doi:10.1002/art.11414
- Barlow, J.H., Williams, B. and Wright, C. (1997) The reliability and validity of the arthritis self-efficacy scale in a UK context. Psychology, Health and Medicine, 2, 3-17. doi:10.1080/13548509708400556
- Richie, J. and Spencer, L. (1994) Qualitative data analysis for applied policy research. In: Bryman and Burgess, Eds., Analyzing Qualitative Data, Routledge, London, 173-194. doi:10.4324/9780203413081_chapter_9
NOTES
*Conflicts of interest: The authors have no conflicts of interest. Contributions: BH and CH prepared the manuscript, TY gave statistical advice, JH, CH, BH, AA, DJ designed the study, AA and DJ reviewed the manuscript.

