Open Journal of Nursing
Vol.3 No.2(2013), Article ID:32966,8 pages DOI:10.4236/ojn.2013.32035
The devil is in the detail: Prevention of diabetic foot ulceration in rural area is possible
![]()
1Graduate Institute of Nursing, Chang Gung University of Science and Technology, Chiayi, Taiwan
2Plastic Surgery, Chang Gung Memorial Hospital, Chiayi, Taiwan
3Ophthalmology, Chang Gung Memorial Hospital, Chiayi, Taiwan
Email: *meiyen@gw.cgust.edu.tw
Copyright © 2013 Chia-Mou Lee et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received 2 March 2013; revised 16 April 2013; accepted 15 May 2013
Keywords: Diabetes; Nursing Assessment; Peripheral Neuropathy; Peripheral Vasculopathy
ABSTRACT
Background: Foot self-care capability is an important factor in diabetic foot ulceration, especially in disadvantaged rural areas. Aim: To explore the causes of foot ulceration and practice foot self-care behaviors before and after diabetic foot ulceration. Method: A descriptive, retrospective design was conducted in a rural hospital in southern Taiwan. Results: A total of 49 participants with diabetic foot ulcers participated in this study. More than half were male (63.3%), still working in farming or fishing (61.2%). All participants were suffering from peripheral neuropathy (100%) and 71.5% showed claudication. Nearly two thirds reported not having received diabetic foot care education and 82% not having received regular vasculopathy assessment before the wound appeared. The common reasons for foot ulcers were unnoticed trauma, neglect of foot self-care. Conclusions: Most diabetic foot ulcers are preventable, since they result from a high prevalence of peripheral neuropathy, inadequate provision of vasculopathy assessment and inappropriate management of foot self-care. Community health nurses can focus care toward screen regularly for early diabetic foot problems.
1. INTRODUCTION
Diabetic foot ulcers are a complication of diabetes, and approximately 5% of sufferers require major amputation. Diabetes is the most common disease process associated with lower limb amputation, accounting for approximately half of nontraumatic amputations [1]. Diabetic foot ulcers result from neuropathy, vasculopathy and immunopathy [2]. Diabetic neuropathy is a significant risk factor for the development of foot ulcer [1,3]. Early diagnosis of peripheral vasculopathy using the ankle brachial pressure index (ABPI) has often been recommended. The ABPI is the ratio between the ankle and brachial systolic blood pressures. A low ABPI is a good marker of vascular disease such as peripheral arterial disease, coronary heart disease, stroke or death [4]. ABPI values have been classified as >0.9 normal and <0.89 abnormal [5].
Epidemiological studies have revealed the prevalence of distal lower limb neuropathy, ranging from 30% to 50% of the diabetic population. Because of its frequent occurrence, more than 60% of diabetic foot ulcers are primarily due to an underlying neuropathy [2]. Loss of nerve function is associated with hyperglycemia, as reflected in the mean level of glycosylated hemoglobin over time. Peripheral neuropathy affects all components of the peripheral nervous system, sensory, motor, and autonomic, each of which contributes to foot ulcer development [2,3].
According to the statistics of ICD-10, type 2 diabetes mellitus (T2DM) is the 4th most common cause of death and the most recent estimate of standardized mortality rate (SMR) was 26.9/105 in Taiwan [6]. The SMR is higher than that in the United States (14.1/105), the United Kingdom (5.0/105), and Japan (4.0/105) [7]. The crude mortality rate from diabetes in Chiayi County (59.4/105) was ranked the highest nationwide [6]. A systematic review indicated that foot ulcers in diabetic patients are common and frequently lead to lower limb amputation [2]. The literature shows that the lifetime risk of a person with diabetes developing a foot ulcer could be as high as 25%, and about one third of these are at risk for amputation [3]. Further, it is believed that a lower limb is lost somewhere in the world every 30 seconds as a consequence of diabetes.
If a diabetic foot ulcer is identified but management is inadequate, there is a high risk of infection, gangrene, amputation and death [1,8]. Foot-related disease is the most common cause of hospital admissions among the diabetic population. Diabetic foot complications cause fifteen times more amputations than that occur in non-diabetic patients. After amputation, physical impairment and disability, psychological barriers, large social costs and medical expenses have been reported in many publications. Also, that expenditure does not include indirect costs relating to loss of productivity, individual patients’ and family costs and loss of quality of life [3,9].
Fortunately, some studies have indicated that enhancing the patient’s foot care capabilities and conducting foot care nursing programs are effective in preventing diabetic foot ulceration, even for patients with a foot ulceration history [3,10,11]. The American Association of Diabetes Educators has suggested seven self-care behaviors for diabetes education [12], including healthy eating, physical activity, and reducing risky behaviors. Lifestyle modifications such as increased physical activity, adherence to medication strategies, and smoking cessation have been shown to improve the condition of T2DM patients markedly [13]. However, many patients all over the world still suffer from diabetic foot ulceration and amputations occur every day. Stories of limb amputations happen again and again, especially in the western coastal Chiayi County. The literature concerning the causes and phenomena of diabetic foot ulceration in Taiwan is limited, especially in relation to rural areas.
2. METHODS
2.1. Design and Participants
The aim of the study was to explore the causes of foot ulceration and to implement foot self-care behaviors before and after diabetic foot ulceration. This study was part of a longitudinal cohort study of HPDMF (health promotion for preventing T2DM foot among rural community residents) in the south-western coastal Chiayi County. A descriptive, retrospective method was applied to participants with diabetic foot ulcers in a rural hospital around southern Taiwan, from February to November 2010. Participants were recruited from the plastic surgery outpatient department. Selection criteria included subjects having been diagnosed as T2DM by a physician, with a history of diabetic foot ulcers but without major amputation, and being willing to participate in the study. Exclusion criteria included serious mental problems and serious diabetes complications, e.g. above-ankle or major amputation.
2.2. Data Collection and Ethical Considerations
This study was approved by the institutional review board ethical committee. During the study period, data were collected by the authors after the purpose and procedure had been explained and informed consent had been obtained from the participants. Using face-to-face interviews with a semi-structured questionnaire, and chart reviews from the hospital computer record, a detailed history was obtained and diabetic foot inspection carried out for each participant.
2.3. Measurements
The instruments and semi-structured questionnaire comprised three sections:
1) Demographic characteristics included birth year, gender, duration of diabetes, history and treatment of diabetes, history of debridement, years in education, occupation, family and personal past health history.
2) Foot self-care capability and the reasons for foot injuries. Five open and semi-structured questions were used: (A) Were you taught diabetes foot care before the wound appeared? (B) What kinds of indoor and outdoor footwear did you use before the wound appeared? Data were classified as “appropriate/inappropriate” depending on whether their shoes provided good protection, such as indoors with/without bare feet, and outdoors with/without bare feet, slippers or sandals. (C) Did you take regular exercise before the wound appeared? Data were classified as “irregular/regular” according to whether the answers were “never” or “sometimes”, or around 30 minutes per day or 3 times a week, or 150 minutes a week. (D) What did you do when the wound appeared? How many times did you hurt your foot? (E) What were the reasons your feet were hurt? How do you think the wound was caused?
3) Health status was determined using the following four indicators from the review chart: 1) Normal glycemic levels and blood pressure were defined by the BHP [14], including HbA1C < 7.0%, fasting blood glucose (FBG) < 130 mg/dl, and blood pressure (BP) < 130/85 mmHg. Blood pressure was measured using standard practice procedures during the study period, while A1C and FBG were recorded from the chart review with the latest lab data; 2) Waist circumference (WC) was used to measure central obesity, measuring the mid-abdominal distance between the last rib margin and the iliac crest. According to the nationwide standard, WC values > 90 cm for men and >80 cm for women were classified as obese; 3) Peripheral neuropathy was assessed using the Michigan neuropathy screening instrument (MNSI, range = 0 - 10) [15]. This instrument contains five parameters:
a) appearance of feet; b) foot ulceration; c) vibration perception at the great toe; d) ankle reflexes; e) 10-g Semmes-Weinstein monofilament. A MNSI score of 2 or more was considered to indicate neuropathy; 4) Peripheral vascular status was evaluated from the patient’s chart review, e.g. ABPI.
2.4. Data Analysis
Both quantitative and qualitative data analyses were performed. Quantitative variables were analyzed using the SPSS statistical software package for Windows (Version 17; SPSS, Inc., Chicago, IL, USA). All tests were twosided, and p values less than 0.05 were considered statistically significant. Missing data were excluded from analysis. Descriptive data and frequency of patient’s reports from the semi-structured questionnaire were recorded as percentages for qualitative analysis.
2.5. Reliability and Validity
The accuracy and adequacy of the above equipment and semi-structured questionnaire were evaluated by a critical review of the literature, professional critiques and pilot trials. Four experts, two plastic wound surgeons, one metabolic endocrinologist and one diabetic nurse educator, were involved in the professional critiques, and a content validity index (CVI) of 0.87 was obtained. Further, according to working experience and academic requirements, the investigators were reliable and their health assessment was valid, specifically during the full foot inspection.
3. RESULTS
Except for five cases with amputations at the knee and above, a total of 49 participants with diabetic foot ulcers participated in this study. More than half (63%) were male and the mean age was 66.1 years (SD = 8.9). The majority of participants (74%) had received less than six years of education. Most of them still worked in farming and fishing (61.2%). The average duration of diabetes was 16.5 years (SD = 10.1). More than two thirds (71.5%) reported suffering claudication, and more than one-third (38.8%) had received minor amputations, e.g. toe or below ankle.
Table 1 showed that 71.4% of participants had fasting blood glucose levels higher than 130 mg/dl, and 57.1% had HbA1C higher than 7%. More than two thirds (69.4%) had a waist circumference greater than 80/90 cm (female/male), and 100% of MNSI were abnormal. Nearly 82% (N = 40) had not had their ankle brachial pressure index checked by physicians between being diagnosed as diabetic and the onset of foot ulceration. Systolic/diastolic blood pressure was higher than the recommended 130/85 mmHg in 71.4% and 20.4%. Most of the treatments were oral medications (59.2%), while 38.8% adopted insulin combined with oral anti-diabetic drugs (OAD). Nearly 88% reported taking regular medication and 44.9% were currently smoking.
More than 77% reported that they had not exercised regularly after being diagnosed with diabetes and before the wound appeared. Footwear was inappropriate in 85.7% (indoor) and 38.8% (outdoor). Before the wound occurred, 65.3% (n = 32) reported not having been taught about diabetes foot care by health care providers. (Figure 1) indicates the reasons why the wounds appeared; more than half (53.1%) were attributed to unnoticed foot trauma, including scratching with fingers because of dry skin and itching, and inappropriate cutting of nails or use of a knife during farming or fishing. Wounds were shoerelated in 18.4% of cases, including foreign bodies inside the shoes. When the wounds occurred, 71.4% (n = 35) of participants neglected them or used their own drugs (traditional or folk medicine) (Figure 2). Only 28.6% consulted experts from hospital or clinics (Table 1).
According to the nonparametric analysis, (Table 2) shows that patients who had received debridement (Z = −2.19, p = 0.03), had a past history of minor amputation (Z = −2.48, p = 0.01) and took irregular or less exercise (p = 0.05) had significantly higher mean rank of MNSI. Female gender, older age, low education level, longer duration of diabetes, absence of foot self-care education, obesity and claudication all tended to be associated with higher mean rank of MNSI, but they did not reach statistical significance.
4. DISCUSSION
Three key findings emerged from this study. First, most of the diabetic foot patients suffered from peripheral neuropathy, poor diabetes control and inappropriate foot self-care. Secondly, many diabetic foot ulceration participants did not receive appropriate foot care education or foot examination by health care providers before or after the wound appeared. Finally, the main cause of foot ulcers was neglect of foot self-care.
4.1. Community Nurses Can Take off Shoes and Early Detection of Peripheral Neuropathy
Several techniques have been developed to induce healing of chronic diabetic foot and many strategies appear satisfactory for diabetic foot ulcers; for instance, new generation dressings e.g. silver dressings, ultrasonic debridement, extracorporeal shockwave therapy and vacuum-assisted closure therapy [16]. However, risks of consequent amputation are still high, since diabetic foot ulcers are typically chronic wounds and difficult to heal. Hence, the best strategy is to prevent diabetic foot ul-

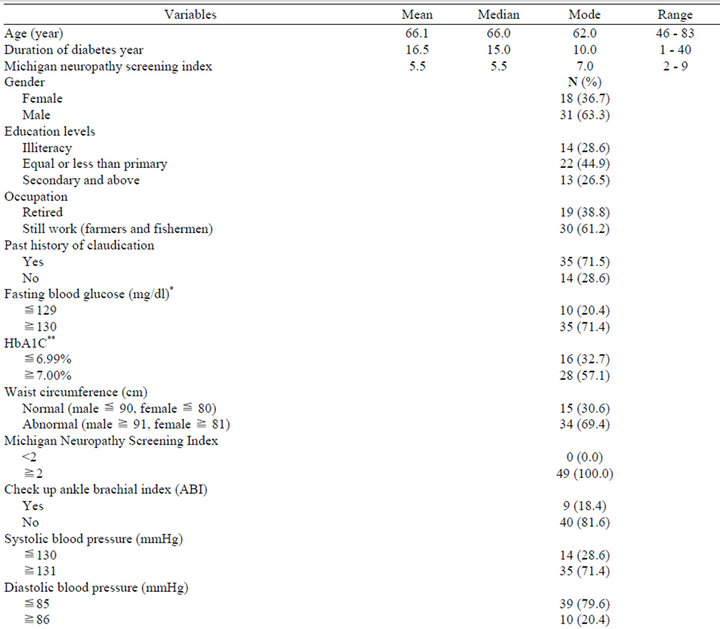
Table 1. Demographic characteristics.

Figure 1. Frequency of the reasons related to foot ulceration.

Figure 2. Self-management of wound by folk-belief.
ceration from happening. Evidence indicates that foot ulcers are more likely to be of neuropathic origin, and therefore eminently preventable [1]. This study found apparent peripheral neuropathy in all patients and claudication in a high percentage. Unfortunately, many participants did not receive adequate foot-care education by primary health care providers.
It can be predicted that primary health care providers might neglect to examine patients’ feet frequently. A possible reason is the limited continuing education for primary health care providers, together with inadequate podiatric care in disadvantaged areas. In a study of physicians and patient chart evaluations in Canada, Bowering [2] reported that fewer than 50% of diabetic patients received appropriate foot evaluation as part of their annual medical checkups. This finding suggested that a requirement for nurses is to take off the patient’s shoes and assess whether there is peripheral neuropathy. This process is not complex, e.g. it takes nurses only a few minutes to judge the appearance of the feet and use a 10-g monofilament to screen for neuropathy. This perspective was also suggested by experts such as Singh et al. [8], who indicated that prevention of diabetic foot ulcers begins with screening for loss of protective sensation, which is best accomplished in the primary care setting with a brief history and the monofilament.
4.2. Ensuring Foot Care Capabilities Should Be Recognized by Diabetic Community Residents
Some studies have indicated that enhancing foot care capability decreases the prevalence of diabetic foot [3, 10,11]. However, the phenomenon of dry and itching skin between the fall and spring seasons was commonly found in this study. According to Taiwan’s weather reports, temperatures below 10 degrees Celsius are common in winter. Only a few patients understood the necessary of using skin lotion and wearing socks to protect their feet, especially in cold weather. Surprisingly, this study found that before the wound appeared, many patients used inappropriate indoor and outdoor footwear, e.g. bare feet were very common both indoors and outdoors. Consequences of unnoticed foot trauma were frequent, e.g. hitting a door or chair, or stepping on fish or chicken bones at home. Furthermore, 10.2% were burnrelated, e.g. some patients made inappropriate use of electric radiators, hot water bags on cold days, or hot water in showers.
Moreover, some myths were found in this study. For instance, some participants said they were told that “walking barefoot on stones in the park is beneficial for health because it stimulates the acupuncture point… hot water benefits health as heat promotes circulation…” Even after the wound occurred, foot self management was lacking and few participants chose experts; instead, traditional medicine and folk beliefs were popular among them. Additionally, many of them thought their wound happened because of bad fate or a curse from God. Therefore, they sought remedies from temples and obtained amulets (Figure 2).
These observations indicate that diabetic rural elders with low social economic status have no knowledge and skill in foot care. The results also reveal that a high proportion of patients (65.3%) have not been taught about diabetes foot care by primary health care providers. The percentages of inappropriate choices of both indoor and outdoor footwear were higher than in a study in India; Chandalia et al. [10] found that 44.7% had not received previous foot care education, 0.6% walked barefoot outdoors, and 45% walked barefoot indoors. Other studies have indicated that diabetic patients with peripheral neuropathy tend to have high risk for plantar skin breakdown owing to unnoticed plantar stresses during walking [3, 17]. Patients who walk barefoot on stones as an exercise option will aggravate their foot injuries.
Nicotine and physical inactivity are well-known risk factors for peripheral arterial disease and diabetic foot [5,18]. However, nearly half the participants in this study were current smokers and more than two thirds did not exercise regularly. In consequence, a high percentage did
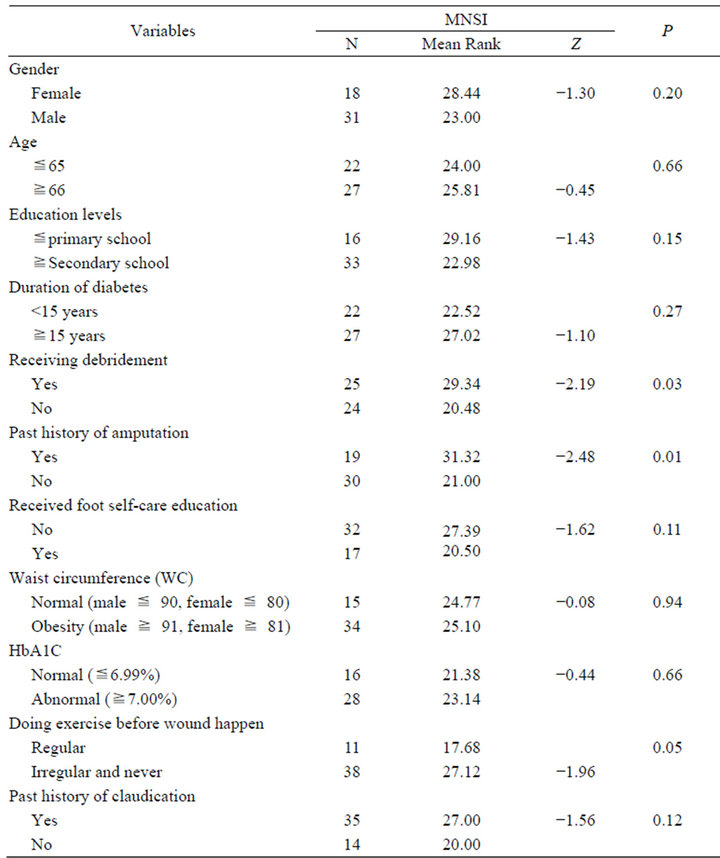
Table 2. Mann-Whitney U test of factors associated with peripheral neuropathy.
not reach expert recommendations for glycemic control [6,12]. Therefore, initiating a nurse-based foot care program is immediately required, including lifestyle modification, teaching patients to choose appropriate shoes with sufficient width, depth, and arch support, and cultivation of foot self-care practice; these are all important issues for disadvantaged patients.
4.3. Enhancing Devil in the Detail
From the findings of this study, most of the causes of foot ulceration were preventable, e.g. by being careful with knives and nail cutting, using skin protection, seeking experts when injury first appears, and using appropriate footwear, but all these tactics were neglected by the participants. In a systematic review, Singh et al. [8] pointed out that educating patients about proper foot care and conducting periodic foot examinations are effective interventions to prevent ulceration. Unfortunately, we cannot take for granted that all diabetic patients will receive the same professional or quality service as in urban areas, though 99% of the Taiwanese population is covered by the national health insurance [6]. Although we all know that ABPI is a noninvasive, and cost-effective strategy for early detection of diabetic foot circulation [2,4,5], most participants had not been checked for ankle brachial pressure at any time and only a low percentage of participants had received foot care education before their foot ulcer appeared. Although 11 patients had received ABPI assessment once, no annual examination took place. A possible reason could be lack of insurance cover.
Therefore, it is necessary to reassess health care accessibility around the rural region, especially for the early detection of diabetic neurovasculopathy to prevent foot ulceration. Continuing education for primary health care providers regarding screening for peripheral neuropathy and vasculopathy through MNSI and ABPI are cost-effective and recommended by many experts [4,5], since the health care costs of peripheral artery disease are extremely high and outcomes are adverse. Hence, the ABPI is the only available tool that can be deployed to identify patients, refer them and facilitate further treatment, with lower costs and improved outcome [18,19].
Further, most of the participants in this study were farmers and fishermen, and the disastrous consequences for their occupational situation must be considered. It is time to initiate foot care nursing programs in local hospital or community settings as a priority. Arts et al. [20] pointed out the cost-effectiveness of substituting physicians with diabetes nurses in terms of quality of life and economic value. Fujiwara et al. [11] encouraged nurses to design and administer foot care programs for diabetic patients aimed at preventing foot ulceration, especially in hospitals that lack podiatrists. Since early neuropathy and vasculopathy are signs of systemic disease, we suggest they should never be regarded as trivial. As suggested by Clair [3], simple methods can save a toe, foot, leg, or even a life. Wherever nurses are in local hospital or community settings, teaching diabetic patients to recognize the devil is in the detail for reducing diabetic foot ulceration is very critical.
4.4. Limitations
Data were obtained from just one local hospital; the small sample size and nonrandom sampling might limit generalizability. Selection and recall bias need to be considered because all the participants had suffered various durations of diabetes, times and levels of foot ulcers. Further research should consider designing a longitudinal study.
5. CONCLUSIONS AND IMPLICATIONS
This study provided valuable information related to the causes of foot ulceration: the high prevalence of peripheral neuropathy, inappropriate footwear, and deficit of foot self-care in disadvantaged rural areas. On the other hand, primary health care providers did not provide regular peripheral neurovascular assessment or adequate foot care education to diabetic patients around the rural area. The findings could be used to develop health strategies to reduce the consequences of foot ulceration and amputation, such as using the simple equipment of MNSI and ABPI for regular screening in disadvantaged regions, since diabetic foot problems are common throughout the world and the economic consequences are extreme. Before diabetic foot ulcers formed, most of the patients had suffered peripheral neuropathy and vasculopathy. If we can identify them earlier and teach them how to protect their feet, it will be possible to reduce the number of foot amputations.
REFERENCES
- Boulton, A.J.M., Vileikyte, L., Ragnarson-Tennvall, G. and Apelqvist, J. (2005) The global burden of diabetic foot disease. Lancet, 366, 1719-1724. doi:10.1016/S0140-6736(05)67698-2
- Bowering, C.K. (2001) Diabetic foot ulcers: Pathophysiology, assessment, and therapy. Canadian Family Physician, 47, 1007-1016.
- Clair, D. (2011) Diabetic foot ulcers: Assessment and education. Long-Term Living: For the Continuing Care Professional, 60, 20-22.
- Doobay, A.V. and Anand, S.S. (2005) Sensitivity and specificity of the ankle-brachial index to predict future cardiovascular outcomes: A systematic review. Arteriosclerosis, Thrombosis, and Vascular Biology, 25, 1463- 1469. doi:10.1161/01.ATV.0000168911.78624.b7
- Alzamora, M., Fores, R. and Baena-Diez, J. (2010) The peripheral arterial disease study: Prevalence and risk factors in the general population. BMC Public Health, 10, 38. doi:10.1186/1471-2458-10-38
- Department of Health (DOH), Executive Yuan, Taiwan (2012) Cause of death statistics: In statistics and publications. http://www.doh.gov.tw/CHT2006/DM/DM2_2.aspx?now_fod_list_no=12336&class_no=440&level_no=4
- World Health Organization (WHO) (2012) World health statistics, World Health Organization, Geneva. http://www.who.int/gho/publications/world_health_statistics/en/index.html
- Singh, N., Armstrong, D.G. and Lipsky, B.A. (2005) Preventing foot ulcers in patients with diabetes. Journal of American Medical Association, 293, 217-228. doi:10.1001/jama.293.2.217
- Manderbacka, K., Peltonen, R., Koskinen, S. and Martikainen, P. (2011) The burden of diabetes mortality in Finland 1988-2007—A brief report. BMC Public Health, 11, 747. doi:10.1186/1471-2458-11-747
- Chandalia, H.B., Singh, D., Kapoor, V., Chandalia, S.H. and Lamba, P.S. (2008) Footwear and foot care knowledge as risk factors for foot problems in Indian diabetics. International Journal of Diabetes in Developing Countries, 28, 109-113. doi:10.4103/0973-3930.45269
- Fujiwara, Y., Kishida, K., Terao, M., Takahara, M. and Matsuhisa, M. (2011) Beneficial effects of foot care nursing for people with diabetes mellitus: An uncontrolled before and after intervention study. Journal of Advanced Nursing, 67, 1952-1962. doi:10.1111/j.1365-2648.2011.05640.x
- American Diabetes Association (ADA) (2008) Standards of medical care in diabetes. Diabetes Care, 32, S62-S63.
- Shaw, M., Savoye, M. and Cali, A. (2009) Effect of a successful intensive lifestyle program on insulin sensitivity and glucose tolerance in obese youth. Diabetes Care, 32, 45-47. doi:10.2337/dc08-0808
- Bureau of Health Promotion (BHP), Department of Health, Taiwan (2011) Adult and elderly health. http://www.bhp.doh.gov.tw/BHPNet/English/Class.aspx?Sub=publications&No=200705180041
- Moghtaderi, A., Bakhshipour, A. and Rashidi, H. (2006) Validation of Michigan neuropathy screening instrument for diabetic peripheral neuropathy. Clinical Neurology and Neurosurgery, 108, 477-481. doi:10.1016/j.clineuro.2005.08.003
- Nather, A., Chionh, S.B., Han, A.Y.Y., Chan, P.L. and Nambiar, A. (2010) Effectiveness of vacuum-assisted closure (VAC) therapy in the healing of chronic diabetic foot ulcers. Annals Academy of Medicine Singapore, 39, 353- 358.
- Mueller, M.J., Zou, D., Bohnert, K.L., Tuttle, L.J. and Sinacore, D.R. (2008) Plantar stresses on the neuropathic foot during barefoot walking. Physical Therapy, 88, 1375- 1384. doi:10.2522/ptj.20080011
- Chen, M.Y., Huang, W.C., Peng, Y.S., Guo, J.S., Chen, C.P., Jong M.C. and Lin H.C. (2011) Effectiveness of a health promotion program for farmers and fishermen with type 2 diabetes in Taiwan. Journal of Advanced Nursing, 67, 2060-2067. doi:10.1111/j.1365-2648.2011.05678.x
- Hiatt, W.R. (2008) Can measuring the ankle-brachial index improve public health? Journal of the American College of Cardiology, 52, 1743-1744. doi:10.1016/j.jacc.2008.08.035
- Arts, E.A., Landewe-Cleuren, S.A.N.T., Schaper, N.C. and Vrijhoef, H.J.M. (2012) The cost-effectiveness of substituting physicians with diabetes nurse specialists: A randomized controlled trial with 2-year follow-up. Journal of Advanced Nursing, 68, 1224-1234. doi:10.1111/j.1365-2648.2011.05797.x
NOTES
*Corresponding author.

